Abstract
Background
Although bariatric surgery is the most effective treatment for obesity and weight-related comorbid diseases, utilization rates are disproportionately low among non-white patients. We sought to understand if variation in baseline characteristics or access to care exists between white and non-white patients.
Methods
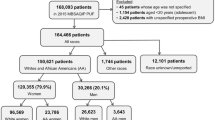
Using a statewide bariatric-specific data registry, we evaluated all patients who underwent bariatric surgery between 2006 and 2020 and completed a preoperative baseline questionnaire, which included a question about self-identification of race. Patient characteristics, co-morbidities, and time from initial preoperative clinic evaluation to date of surgery were compared among racial groups.
Results
A total of 73,141 patients met inclusion criteria with 18,741 (25.5%) self-identified as non-white. These included Black/African American (n = 11,904), Hispanic (n = 3448), Asian (n = 121), Native Hawaiian/Pacific Islander (n = 41), Middle Eastern (n = 164), Multiple (n = 2047) and other (n = 608). Non-white males were the least represented group, accounting for only 4% of all bariatric cases performed. Non-white patients were more likely to be younger (43.0 years vs. 46.6 years, p < 0.0001), disabled (16% vs. 11.4%, p < 0.0001) and have Medicaid (8.4% vs. 3.8%, p < 0.0001) when compared to white patients, despite having higher rates of college education (78.0% vs. 76.6, p < 0.0001). In addition, median time from initial evaluation to surgery was also longer among non-white patients (157 days vs. 127 days, p < 0.0001), despite having higher rates of patients with a body mass index above 50 kg/m2 (39.0% vs. 33.2%, p < 0.0001).
Conclusions
Non-white patients undergoing bariatric surgery represent an extremely diverse group of patients with more socioeconomic disadvantages and longer wait times when compared to white patients despite presenting with higher rates of severe obesity. Current guidelines and referral patterns for bariatric surgery may not be equitable and need further examination when considering the management of obesity within diverse populations to reduce disparities in care—of which non-white males are particularly at risk.

Similar content being viewed by others
References
Ogden CL, Fryar CD, Martin CB et al (2020) Trends in obesity prevalence by race and hispanic origin—1999-2000 to 2017–2018. JAMA 324(12):1208–1210. https://doi.org/10.1001/jama.2020.14590
Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, Schoelles K (2004) Bariatric surgery: a systematic review and meta-analysis. JAMA 292:1724–1737
Varban O, Dimick J (2019) Bariatric surgery: safe, effective, and underutilized. Fam Med 51(7):552–554
Yermilov I, McGory ML, Shekelle PW, Ko CY, Maggard MA (2009) Appropriateness criteria for bariatric surgery: beyond the NIH guidelines. Obesity 17(8):1521–1527
Alvarez R, Matusko N, Stricklen AL, Ross R, Buda CM, Varban OA (2018) Factors associated with bariatric surgery utilization among eligible candidates: who drops out? Surg Obes Relat Dis 14(12):1903–1910
Pitzul KB, Jackson T, Crawford S et al (2014) Understanding disposition after referral for bariatric surgery: when and why patients referred do not undergo surgery. Obes Surg 24(1):134–140
Nguyen NT, Masoomi H, Magno CP, Nguyen XMT, Laugenour K, Lane J (2011) Trends in use of bariatric surgery, 2003–2008. J Am Coll Surg 213(2):261–266. https://doi.org/10.1016/j.jamcollsurg.2011.04.030
Nguyen GC, Patel AM (2013) Racial disparities in mortality in patients undergoing bariatric surgery in the USA. Obes Surg 23(10):1508–1514
Johnson-Mann C, Martin AN, Williams MD, Hallowell PT, Schirmer B (2019) Investigating racial disparities in bariatric surgery referrals. Surg Obes Relat Dis 15(4):615–620
Campos GM, Khoraki J, Browning MG, Pessoa BM, Mazzini GS, Wolfe L (2020) Changes in utilization of bariatric surgery in the United States from 1993 to 2016. Ann Surg 271(2):201–209
Martin M, Beekley A, Kjorstad R, Sebesta J (2010) Socioeconomic disparities in eligibility and access to bariatric surgery: a national population-based analysis. Surg Obes Related Dis 6(1):8–15
Hecht LM, Pester B, Braciszewski JM et al (2020) Socioeconomic and racial disparities in bariatric surgery. Obes Surg 30:1–5
Sundbom M, Franzén S, Ottosson J, Svensson AM (2020) Superior socioeconomic status in patients with type 2 diabetes having gastric bypass surgery: a case-control analysis of 10 642 individuals. BMJ Open Diabetes Res Care 8(1):e000989
Flum DR, Khan TV, Dellinger EP (2007) Toward the rational and equitable use of bariatric surgery. JAMA 298(12):1442–1444
Wood MH, Carlin AM, Ghaferi AA et al (2019) Association of race with bariatric surgery outcomes. JAMA Surg 154(5):e190029
Harvin G, DeLegge M, Garrow DA (2008) The impact of race on weight loss after Roux-en-Y gastric bypass surgery. Obes Surg 18(1):39–42
Mocanu V, Dang JT, Switzer N, Madsen K, Birch DW, Karmali S (2020) Sex and race predict adverse outcomes following bariatric surgery: an MBSAQIP analysis. Obes Surg 30(3):1093–1101
Alvarez R, Bonham AJ, Buda CM, Carlin AM, Ghaferi AA, Varban OA (2019) Factors associated with long wait times for bariatric surgery. Ann Surg 270(6):1103–1109
On racism: a new standard for publishing on racial health inequities|health affairs blog. https://www.healthaffairs.org/do/https://doi.org/10.1377/forefront.20200630.939347/full/. Accessed 3 Sept 2021
Haider AH, Scott VK, Rehman KA et al (2013) Racial disparities in surgical care and outcomes in the United States: a comprehensive review of patient, provider, and systemic factors. J Am Coll Surg 216(3):482-492.e12. https://doi.org/10.1016/j.jamcollsurg.2012.11.014
Weis BD (2003) Health Literacy: A Manual for Clinicians. Chicago, IL: American Medical Association, American Medical Foundation. National Institutes of Health. How to Write Easy to Read Health Materials: National Library of Medicine Website.
Safeer RS, Keenan J (2005) Health literacy: the gap between physicians and patients. Am Fam Physician 72(3):463–468
Zhou AQ, Lee HY, Lee RM (2019) Who has low health literacy and does it matter for depression? Findings from aggregated and disaggregated racial/ethnic groups. Cultur Divers Ethnic Minor Psychol 25(1):73–81. https://doi.org/10.1037/cdp0000210
Birkmeyer NJ, Gu N (2012) Race, socioeconomic status, and the use of bariatric surgery in Michigan. Obes Surg 22(2):259–265
Ames GE, Maynard JR, Collazo-Clavell ML, Clark MM, Grothe KB, Elli EF (2020) Rethinking patient and medical professional perspectives on bariatric surgery as a medically necessary treatment. Mayo Clin Proc 95(3):527–540. https://doi.org/10.1016/j.mayocp.2019.09.019
Wee CC, Huskey KW, Bolcic-Jankovic D, Colten ME, Davis RB, Hamel M (2014) Sex, race, and consideration of bariatric surgery among primary care patients with moderate to severe obesity. J Gen Intern Med 29(1):68–75
Santry HP, Lauderdale DS, Cagney KA, Rathouz PJ, Alverdy JC, Chin MH (2007) Predictors of patient selection in bariatric surgery. Ann Surg 245(1):59–67. https://doi.org/10.1097/01.sla.0000232551.55712.b3
Allison KC, Grilo CM, Masheb RM, Stunkard AJ (2005) Binge eating disorder and night eating syndrome: a comparative study of disordered eating. J Consult Clin Psychol 73(6):1107
Taylor T, Wrapson W, Dewes O, Taufa N, Siegert RJ (2019) Preoperative bariatric surgery programme barriers facing Pacific patients in Auckland, New Zealand as perceived by health sector professionals: a qualitative study. BMJ Open 9(11):e029525. https://doi.org/10.1136/bmjopen-2019-029525
Al-Ozairi E, Al Kandari J, AlHaqqan D, AlHarbi O, Masters Y, Syed AA (2015) Obesity surgery and Ramadan: a prospective analysis of nutritional intake, hunger and satiety and adaptive behaviours during fasting. Obes Surg 25(3):523–529
Daldal E, Dagmura H, Dasiran F, Okan I, Bulbuloglu E (2021) Ramadan fasting increases socialization in patients who underwent sleeve gastrectomy: an observational study. Obes Surg 31(6):2576–2582
Razak F, Anand SS, Shannon H et al (2007) Defining obesity cut points in a multiethnic population. Circulation 115(16):2111–2118. https://doi.org/10.1161/CIRCULATIONAHA.106.635011
Low S, Chin MC, Ma S, Heng D, Deurenberg-Yap M (2009) Rationale for redefining obesity in Asians. Ann Acad Med Singap 38(1):66
Bennet L, Stenkula K, Cushman SW, Brismar K (2016) BMI and waist circumference cut-offs for corresponding levels of insulin sensitivity in a Middle Eastern immigrant versus a native Swedish population—the MEDIM population based study. BMC Public Health 16(1):1–12. https://doi.org/10.1186/s12889-016-3892-1
Pories WJ et al (2021) Beyond the BMI: the search for better guidelines for bariatric surgery. Obesity. https://doi.org/10.1038/oby.2010.8
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Varban, Finks, and Ghaferi receive salary support from Blue Cross Blue Shield of Michigan for leadership and participation in the Michigan Bariatric Surgery Collaborative. Dr. Ghaferi is President of the Association of Academic Surgery. Ms. Jiang, Mr. Bonham, and Drs. Shen, Bonner, and Millis have no conflict of interest or financial ties to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shen, M.R., Jiang, S., Millis, M.A. et al. Racial variation in baseline characteristics and wait times among patients undergoing bariatric surgery. Surg Endosc 37, 564–570 (2023). https://doi.org/10.1007/s00464-022-09292-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-022-09292-w