Abstract
Background
Robotic-assisted surgery is increasing and there is a need for a structured and evidence-based curriculum to learn basic robotic competencies. Relevant training tasks, eligible trainees, realistic learning goals, and suitable training methods must be identified. We sought to develop a common curriculum that can ensure basic competencies across specialties.
Methods
Two robotic surgeons from all departments in Denmark conducting robotic-assisted surgery within gynecology, urology, and gastrointestinal surgery, were invited to participate in a three-round Delphi study to identify learning goals and rank them according to relevance for a basic curriculum. An additional survey was conducted after the Delphi rounds on what training methods were considered best for each learning goal and who (console surgeon/patient-side assistant) should master each learning goal.
Results
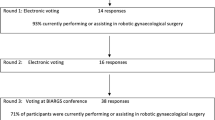
Fifty-six robotic surgeons participated and the response rates were 86%, 89%, and 77%, for rounds 1, 2 and 3, respectively. The Delphi study identified 40 potential learning goals, of which 29 were ranked as essential, e.g., Understand the link between arm placement and freedom of movement or Be able to perform emergency un-docking. In the additional survey, the response rate was 70%. Twenty-two (55%) of the identified learning goals were found relevant for the patient-side assistant and twenty-four (60%) were linked to a specific suitable learning method with > 75% agreement.
Conclusions
Our findings can help training centers plan their training programs concerning educational content and methods for training/learning. Furthermore, patient-side assistants should also receive basic skills training in robotic surgery.

Similar content being viewed by others
Data availability
The datasets used for this study are available from the corresponding author on reasonable request.
References
Intuitive Surgical Announces Preliminary Fourth Quarter and Full Year 2019 Results. https://isrg.intuitive.com/news-releases/news-release-details/intuitive-announces-preliminary-fourth-quarter-and-full-year. Accessed 16 Nov 2020
Veronesi G, Dorn P, Dunning J, Cardillo G, Schmid RA, Collins J, Baste JM, Limmer S, Shahin GMM, Egberts JH, Pardolesi A, Meacci E, Stamenkovic S, Casali G, Rueckert JC, Taurchini M, Santelmo N, Melfi F, Toker A (2018) Outcomes from the Delphi process of the thoracic robotic curriculum development committee. Eur J Cardiothorac Surg 53:1173–1179. https://doi.org/10.1093/ejcts/ezx466
Peters BS, Armijo PR, Krause C, Choudhury SA, Oleynikov D (2018) Review of emerging surgical robotic technology. Surg Endosc 32:1636–1655. https://doi.org/10.1007/s00464-018-6079-2
Kowalewski KF, Schmidt MW, Proctor T, Pohl M, Wennberg E, Karadza E, Romero P, Kenngott HG, Müller-Stich BP, Nickel F (2018) Skills in minimally invasive and open surgery show limited transferability to robotic surgery: results from a prospective study. Surg Endosc 32:1656–1667. https://doi.org/10.1007/s00464-018-6109-0
Gillespie BM, Gillespie J, Boorman RJ, Granqvist K, Stranne J, Erichsen-Andersson A (2020) The impact of robotic-assisted surgery on team performance: a systematic mixed studies review. Hum Factors. https://doi.org/10.1177/0018720820928624
Gawande AA, Zinner MJ, Studdert DM, Brennan TA (2003) Analysis of errors reported by surgeons at three teaching hospitals. Surgery 133:614–621. https://doi.org/10.1067/msy.2003.169
Muaddi H, El HM, Choi WJ, Lillie E, de Mestral C, Nathens A, Stukel TA, Karanicolas PJ (2020) Clinical outcomes of robotic surgery compared to conventional surgical approaches (Laparoscopic or Open). Ann Surg. https://doi.org/10.1097/sla.0000000000003915
Quality and Patient Safety Division (2013) Advisory on Robot-assisted surgery. In: Commonw. Massachusetts Board Regist. Med. https://www.mass.gov/doc/march-2013-robot-assisted-surgery-advisory/download. Accessed 22 Dec 2020
Herron DM, Marohn M, Advincula A, Aggarwal S, Palese M, Broderick T, Broeders I, Byer A, Curet M, Earle D, Giulianotti P, Grundfest W, Hashizume M, Kelley W, Lee D, Weinstein G, McDougall E, Meehan J, Melvin S, Menon M, Oleynikov D, Patel V, Satava R, Schwaitzberg S (2008) A consensus document on robotic surgery. Surg Endosc Other Interv Tech 22:313–325. https://doi.org/10.1007/s00464-007-9727-5
ERUS Robotic Curriculum. European Association of Urology. https://uroweb.org/section/erus/education/. Accessed 22 Dec 2020
Satava RM, Stefanidis D, Levy JS, Smith R, Martin JR, Monfared S, Timsina LR, Darzi AW, Moglia A, Brand TC, Dorin RP, Dumon KR, Francone TD, Georgiou E, Goh AC, Marcet JE, Martino MA, Sudan R, Vale J, Gallagher AG (2019) Proving the effectiveness of the fundamentals of robotic surgery (FRS) skills curriculum: a single-blinded multispecialty multi-institutional randomized control trial. Ann Surg. https://doi.org/10.1097/sla.0000000000003220
Stegemann AP, Ahmed K, Syed JR, Rehman S, Ghani K, Autorino R, Sharif M, Rao A, Shi Y, Wilding GE, Hassett JM, Chowriappa A, Kesavadas T, Peabody JO, Menon M, Kaouk J, Guru KA (2013) Fundamental skills of robotic surgery: a multi-institutional randomized controlled trial for validation of a simulation-based curriculum. Urology 81:767–774. https://doi.org/10.1016/j.urology.2012.12.033
Carpenter BT, Sundaram CP (2017) Training the next generation of surgeons in robotic surgery. Robot Surg Res Rev 4:39–44. https://doi.org/10.2147/rsrr.s70552
Brinkman W, de Angst I, Schreuder H, Schout B, Draaisma W, Verweij L, Hendrikx A, van der Poel H (2017) Current training on the basics of robotic surgery in the Netherlands: time for a multidisciplinary approach? Surg Endosc 31:281–287. https://doi.org/10.1007/s00464-016-4970-2
Schreuder HW, Wolswijk R, Zweemer RP, Schijven MP, Verheijen RH (2012) Training and learning robotic surgery, time for a more structured approach: a systematic review. BJOG 119:137–149. https://doi.org/10.1111/j.1471-0528.2011.03139.x
Thomas PA, Kern DE, Hughes MTCB (2015) Curriculum development for medical education: a six-step approach. Johns Hopkins University Press, Baltimore
Bjerrum F, Thomsen ASS (2018) Surgical simulation: current practices and future perspectives for technical skills training. Med Teach 40:668–675. https://doi.org/10.1080/0142159x.2018.1472754
Topperzer MK, Thellesen L, Hoffmann M, Larsen HB, Weibel M, Lausen B, Schmiegelow K, Sørensen JL (2020) Establishment of consensus on content and learning objectives for an interprofessional education in childhood cancer: a Delphi survey. BMJ Paediatr Open. https://doi.org/10.1136/bmjpo-2019-000634
Collins JW, Levy J, Stefanidis D, Gallagher A, Coleman M, Cecil T, Ericsson A, Mottrie A, Wiklund P, Ahmed K, Pratschke J, Casali G, Ghazi A, Gomez M, Hung A, Arnold A, Dunning J, Martino M, Vaz C, Friedman E, Baste JM, Bergamaschi R, Feins R, Earle D, Pusic M, Montgomery O, Pugh C, Satava RM (2019) Utilising the Delphi process to develop a proficiency-based progression train-the-trainer course for robotic surgery training. Eur Urol. https://doi.org/10.1016/j.eururo.2018.12.044
Nayahangan LJ, Van Herzeele I, Konge L, Koncar I, Cieri E, Mansilha A, Debus S, Eiberg JP (2019) Achieving consensus to define curricular content for simulation based education in vascular surgery: a europe wide needs assessment initiative. Eur J Vasc Endovasc Surg 58:284–291. https://doi.org/10.1016/j.ejvs.2019.03.022
Jensen RD, Paltved C, Jaensch C, Durup J, Beier-Holgersen R, Konge L, Nayahangan L, Madsen AH (2021) Identifying technical skills and clinical procedures in surgery for a simulation-based curriculum: a national general needs assessment. Surg Endosc. https://doi.org/10.1007/s00464-020-08235-7
Jones J, Hunter D (1995) Consensus methods for medical and health services research. BMJ 311:376–380. https://doi.org/10.1136/bmj.311.7001.376
Khamis NN, Satava RM, Alnassar SA, Kern DE (2016) A stepwise model for simulation-based curriculum development for clinical skills, a modification of the six-step approach. Surg Endosc 30:279–287. https://doi.org/10.1007/s00464-015-4206-x
Hackett S, Masson H, Phillips S (2006) Exploring consensus in practice with youth who are sexually abusive: findings from a Delphi study of practitioner views in the United Kingdom and the Republic of Ireland. Child Maltreat 11:146–156. https://doi.org/10.1177/1077559505285744
Thellesen L, Hedegaard M, Bergholt T, Colov NP, Hoegh S, Sorensen JL (2015) Curriculum development for a national cardiotocography education program: a Delphi survey to obtain consensus on learning objectives. Acta Obs Gynecol Scand 94:869–877. https://doi.org/10.1111/aogs.12662
Thomsen ASS, la Cour M, Paltved C, Lindorff-Larsen KG, Nielsen BU, Konge L, Nayahangan LJ (2018) Consensus on procedures to include in a simulation-based curriculum in ophthalmology: a national Delphi study. Acta Ophthalmol 96:519–527. https://doi.org/10.1159/00049343110.1111/aos.13700
Gargon E, Crew R, Burnside G, Williamson PR (2019) Higher number of items associated with significantly lower response rates in COS Delphi surveys. J Clin Epidemiol 108:110–120. https://doi.org/10.1016/j.jclinepi.2018.12.010
Rusch P, Kimmig R, Lecuru F, Persson J, Ponce J, Degueldre M, Verheijen R (2018) The society of european robotic gynaecological surgery (SERGS) Pilot Curriculum for robot assisted gynecological surgery. Arch Gynecol Obstet 297:415–420. https://doi.org/10.1007/s00404-017-4612-5
ERUS Robotic Curriculum. European Association of Urology. https://uroweb.org/section/erus/education/. Accessed 17 Nov 2020
Ismail A, Wood M, Ind T, Gul N, Moss E (2020) The development of a robotic gynaecological surgery training curriculum and results of a Delphi study. BMC Med Educ 20:1–7. https://doi.org/10.1186/s12909-020-1979-y
Haynes AB, Weiser TG, Berry WR, Lipsitz SR, Breizat A-HS, Dellinger EP, Herbosa T, Joseph S, Kibatala PL, Lapitan MCM, Merry AF, Moorthy K, Reznick RK, Taylor B, Gawande AA (2009) A surgical safety checklist to reduce morbidity and mortality in a global population. N Engl J Med 360:491–499. https://doi.org/10.1056/nejmsa0810119
Khalafallah YM, Bernaiche T, Ranson S, Liu C, Collins DT, Dort J, Hafner G (2020) Residents’ views on the impact of robotic surgery on general surgery education. J Surg Educ. https://doi.org/10.1016/j.jsurg.2020.10.003
Ahmed K, Khan R, Mottrie A, Lovegrove C, Abaza R, Ahlawat R, Ahlering T, Ahlgren G, Artibani W, Barret E, Cathelineau X, Challacombe B, Coloby P, Khan MS, Hubert J, Michel MS, Montorsi F, Murphy D, Palou J, Patel V, Piechaud PT, Van Poppel H, Rischmann P, Sanchez-Salas R, Siemer S, Stoeckle M, Stolzenburg JU, Terrier JE, Thüroff JW, Vaessen C, Van Der Poel HG, Van Cleynenbreugel B, Volpe A, Wagner C, Wiklund P, Wilson T, Wirth M, Witt J, Dasgupta P (2015) Development of a standardised training curriculum for robotic surgery: a consensus statement from an international multidisciplinary group of experts. BJU Int 116:93–101. https://doi.org/10.1111/bju.12974
Al-Jundi W, Wild J, Ritchie J, Daniels S, Robertson E, Beard J (2016) Assessing the nontechnical skills of surgical trainees: views of the theater team. J Surg Educ 73:222–229. https://doi.org/10.1016/j.jsurg.2015.10.008
Prineas S, Mosier K, Mirko C, Guicciardi S (2021) Non-technical skills in healthcare. In: Donaldson L, Ricciardi W, Sheridan S, Tartaglia R (eds) Textbook of patient safety and clinical risk management. Springer International Publishing, Cham, pp 413–434
Raison N, Wood T, Brunckhorst O, Abe T, Ross T, Challacombe B, Khan MS, Novara G, Buffi N, Van Der Poel H, McIlhenny C, Dasgupta P, Ahmed K (2017) Development and validation of a tool for non-technical skills evaluation in robotic surgery-the ICARS system. Surg Endosc 31:5403–5410. https://doi.org/10.1007/s00464-017-5622-x
Diamond IR, Grant RC, Feldman BM, Pencharz PB, Ling SC, Moore AM, Wales PW (2014) Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 67:401–409. https://doi.org/10.1016/j.jclinepi.2013.12.002
Zhao B, Lam J, Hollandsworth HM, Lee AM, Lopez NE, Abbadessa B, Eisenstein S, Cosman BC, Ramamoorthy SL, Parry LA (2020) General surgery training in the era of robotic surgery: a qualitative analysis of perceptions from resident and attending surgeons. Surg Endosc 34:1712–1721. https://doi.org/10.1007/s00464-019-06954-0
Kumar R, Hemal AK (2006) The “scrubbed surgeon” in robotic surgery. World J Urol 24:144–147. https://doi.org/10.1007/s00345-006-0068-0
Fong Y, Buell JF, Collins J, Martinie J, Bruns C, Tsung A, Clavien PA, Nachmany I, Edwin B, Pratschke J, Solomonov E, Koenigsrainer A, Giulianotti PC (2020) Applying the Delphi process for development of a hepatopancreaticobiliary robotic surgery training curriculum. Surg Endosc 34:4233–4244. https://doi.org/10.1007/s00464-020-07836-6
Burden C, Fox R, Lenguerrand E, Hinshaw K, Draycott TJ, James M (2014) Curriculum development for basic gynaecological laparoscopy with comparison of expert trainee opinions; Prospective cross-sectional observational study. Eur J Obstet Gynecol Reprod Biol 180:1–7. https://doi.org/10.1016/j.ejogrb.2014.05.036
Acknowledgements
We would like to thank all the participants in the Delphi panel, their departments and hospitals: Rigshospitalet (Copenhagen), Herlev Hospital, University Hospital Zealand; Køge and Roskilde, Aalborg University Hospital, Aarhus University Hospital, Region Hospital Herning, Region Hospital Holstebro, Odense University Hospital, Hospital Sønderjylland, Lillebaelt Hospital, and Hospital of South West Jutland.
Funding
This study is part of a Ph.D. project funded by the University of Southern Denmark (Faculty scholarship for Peter Hertz). The funder did not influence the protocol development or had access to the data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Peter Hertz, Flemming Bjerrum, Kim Houlind, Pernille Tine Jensen, Mikkel Lønborg Friis, Jan Jepsen, Lars Bundgaard and Lars Konge have no conflicts of interest or financial ties to disclose.
Ethical approval
The study was submitted to the Regional Ethical Committee of Southern Denmark, which found that ethical approval was not required (Journal No. 201920000-88).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Hertz, P., Houlind, K., Jepsen, J. et al. Identifying curriculum content for a cross-specialty robotic-assisted surgery training program: a Delphi study. Surg Endosc 36, 4786–4794 (2022). https://doi.org/10.1007/s00464-021-08821-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-021-08821-3