Abstract
Background
The optimal approach at treating infected biliary stents at the time of cholangitis remains unknown. This study aims to compare the efficacy of stent exchange versus stent sweeping/stent-in-stent approaches at treating cholangitis.
Methods
The study was a retrospective cohort study. Patients with biliary stents and cholangitis were included. Outcomes were rate of recurrent cholangitis and time to recurrent cholangitis in those whose stents were left in place (stent sweeping and stent-in-stent) compared to those whose stents were removed (stent exchange). Primary analysis included patients with metal biliary stents only. Secondary analysis included those with metal and plastic biliary stents.
Results
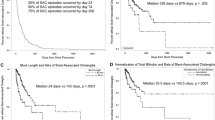
A total of 182 patients (age 64 ± 12;89 F) with a metal biliary stent(s) at index cholangitis were included. Of these, 40 (22%) had stents removed, i.e., stent exchange. The remaining 142 (78%) did not have stent removal (97 with stent-in-stent and 45 with stent sweeping). Recurrent cholangitis occurred in 22.5% and 42.3% in the stent removal and non-removal groups, respectively (p = 0.02). Stent removal remained a negative predictor of recurrent cholangitis after controlling for age, sex, history of diabetes, and chemotherapy (OR 0.39, p = 0.03). Median time from index cholangitis to recurrent cholangitis was shorter for patients whose stents were not removed compared to those whose stents were removed (182 vs 450 days, p = 0.011). On Cox regression model, stent removal remained a negative predictor of recurrent cholangitis after controlling for age, sex, history of diabetes, and chemotherapy (HR 0.41, p = 0.01). The findings persisted in the secondary analysis including both metal and plastic biliary stents (303 patients).
Conclusion
Biliary stent removal with stent exchange at the time of cholangitis appears to be more effective at preventing recurrent cholangitis than leaving an infected stent in the biliary system.


Similar content being viewed by others
References
Charcot M (1877) Comparison avec la fievre uroseptique. Lecons sur les maladies du foie des voies biliares et des reins. Paris: Bourneville et Sevestre. De la fievre hepatique symptomatique; pp 176–85
Reynolds BM, Dargan EL (1959) Acute obstructive cholangitis; a distinct clinical syndrome. Ann Surg 150(2):299–303
Kimura Y, Takada T, Kawarada Y, Nimura Y, Hirata K, Sekimoto M, Yoshida M, Mayumi T, Wada K, Miura F, Yasuda H, Yamashita Y, Nagino M, Hirota M, Tanaka A, Tsuyuguchi T, Strasberg SM, Gadacz TR (2007) Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg 14(1):15–26
Gigot JF, Leese T, Dereme T, Coutinho J, Castaing D, Bismuth H (1989) Acute cholangitis: multivariate analysis of risk factors. Ann Surg 209:435–438. https://doi.org/10.1097/00000658-198904000-00008
Saharia PC, Cameron JL (1976) Clinical management of acute cholangitis. Surg Gynecol Obstet 142:369–372
Thompson JE Jr, Pitt HA, Doty JE, Coleman J, Irving C (1990) Broad spectrum penicillin as an adequate therapy for acute cholangitis. Surg Gynecol Obstet 171:275–282
Basoli A, Schietroma M, De Santis A, Colella A, Fiocca F, Speranza V (1986) Acute cholangitis: diagnostic and therapeutic problems. Ital J Surg Sci 16:261–267
Huibregtse K, Carr-Locke DL, Cremer M et al (1992) Biliary stent occlusion—a problem solved with self-expanding metal stents? European Wallstent Study Group. Endoscopy 24(5):391–394
Knyrim K, Wagner HJ, Pausch J et al (1993) A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy 25(3):207–212
Kiriyama S, Takada T, Strasberg SM et al (2012) New diagnostic criteria and severity assessment of acute cholangitis in revised Tokyo Guidelines. J Hepatobiliary Pancreat Sci 19(5):548–556
Miura F, Takada T, Stransberg SM et al (2013) TG13 flowchart for the management of acute cholangitis and cholecystitis. J Hepatobiliary Pancreat Sci 20:47–54
Ridtitid W, Rerknimitr R, Janchai A et al (2010) Outcome of second interventions for occluded metallic stents in patients with malignant biliary obstruction. Surg Endosc 42:2216–2220
Togawa O, Kawabe T, Isayama H et al (2008) Management of occluded uncovered metallic stents in patients with malignant distal biliary obstructions using covered metallic stents. J Clin Gastroenterol 42:546–549
Bueno JT, Gerdes H, Kurtz RC (2003) Endoscopic management of occluded biliary Wallstents: a cancer center experience. Gastrointest Endosc 58:879–884
Rogant JN, Jain D, Siddiqui UD et al (2008) Analysis of endoscopic management of occluded metal biliary stents at a single tertiary care center. Gastrointest Endosc 68:676–682
Tham TC, Carr-Locke DL, Vandervoort J et al (1998) Management of occluded biliary Wallstents. Gut 42:703–707
Yoon WJ, Ryu JK, Lee JW et al (2010) Endoscopic management of occluded metal biliary stents: metal versus 10F plastic stents. World J Gastroenterol 14:5347–5352
Libby ED, Leung JW (1996) Prevention of biliary stent clogging: a clinical review. Am J Gastroenterol 91:1301–1308
Leung JW, Liu Y, Chan RC et al (2000) Early attachment of anaerobic bacteria may play an important role in biliary stent blockage. Gastrointest Endosc 52:725–729
van Berkel AM, van Marle J, Groen AK et al (2005) Mechanisms of biliary stent clogging: confocal laser scanning and scanning electron microscopy. Endoscopy 37:729–734
Donelli G, Guaglianone E, Di Rosa R et al (2007) Plastic biliary stent occlusion: factors involved and possible preventive approaches. Clin Med Res 5:53–60
Moesch C, Sautereau D, Cessot F et al (1991) Physicochemical and bacteriological analysis of the contents of occluded biliary endoprostheses. Hepatology 13:1142–1146
An YH, Friedman RJ (1998) Concise review of mechanisms of bacterial adhesion to biomaterial surfaces. J BiomedMaterRes 43:338–348
Yu JL, Anderson R, Wang LQ (1995) Fibronectin on the surface of biliary drain materials: a role in bacterial adherence. J Surg Res 59:596–600
Landau O, Kott I, Deutsch AA et al (1992) Multifactorial analysis of septic bile and septic complications in biliary surgery. World J Surg 16:962–964
Hashimoto J, Morizane C, Kondo S et al (2011) Incidence and risk factors for cholangitis during systemic chemotherapy among patients with advanced biliary tract cancer. J Clin Oncol 29:313
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Pichamol Jirapinyo, Mohd AlSamman, and Christopher Thompson have no conflicts of interest or financial ties to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jirapinyo, P., AlSamman, M.A. & Thompson, C.C. Impact of infected stent removal on recurrent cholangitis with time-to-event analysis. Surg Endosc 33, 4109–4115 (2019). https://doi.org/10.1007/s00464-019-06714-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-019-06714-0