Abstract
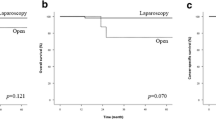
Laparoscopic D3 lymph node dissection for transverse colon cancer is technically demanding because of complicated anatomy. Here, we reviewed the vascular structure of the transverse mesocolon, explored the extent of the base of the transverse mesocolon, and evaluated the feasibility and oncological safety of D3 lymph node dissection. We retrospectively reviewed the clinical records of 42 patients with advanced transverse colon cancer who underwent curative surgery and D3 dissection at Kyushu University Hospital between January 2008 and December 2015. We examined the venous and arterial anatomy of the transverse mesocolon of each resection and compared surgical outcomes between patients who underwent laparoscopic D3 (Lap D3) and open D3 (Open D3) dissection. Patients included two with Stage I, 18 with Stage II, 20 with Stage III, and two with Stage IVA. Thirty-six (85.7%) and six (14.3%) patients underwent Lap D3 or Open D3, respectively. The tumor sizes of the Open D3 and Lap D3 groups were 7.8 and 3.7 cm, respectively (P < 0.001). The Lap D3 group had significantly less blood loss (26 mL vs 272 mL, P = 0.002). The other outcomes of the two groups were not significantly different, including 3-year overall survival (87.7% vs 83.3%, P = 0.385). We observed four patterns of the middle colic artery (MCA) arising from the superior mesenteric artery (SMA), and the frequency of occurrence of a single MCA was 64.3%. The right-middle colic vein (MCV) was present in 92.9% of resections and served as a tributary of the gastrocolic trunk, and 90.5% of the left MCVs drained into the superior mesenteric vein (SMV). The root of the transverse mesocolon was broadly attached to the head of the pancreas and to the surfaces of the SMV and SMA. Laparoscopic D3 lymph node dissection may be tolerated by patients with advanced transverse colon cancer.



Similar content being viewed by others
References
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69:613–616
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation–technical notes and outcome. Colorectal Dis 11:354–364; discussion 364 – 355
West NP, Hohenberger W, Weber K, Perrakis A, Finan PJ, Quirke P (2010) Complete mesocolic excision with central vascular ligation produces an oncologically superior specimen compared with standard surgery for carcinoma of the colon. J Clin Oncol 28:272–278
Culligan K, Coffey JC, Kiran RP, Kalady M, Lavery IC, Remzi FH (2012) The mesocolon: a prospective observational study. Colorectal Dis 14:421–428; discussion 428–430
Mike M, Kano N (2014) Laparoscopic surgery for colon cancer: a review of the fascial composition of the abdominal cavity. Surg Today. 45:129–39
Lacy AM, Garcia-Valdecasas JC, Delgado S, Castells A, Taura P, Pique JM, Visa J (2002) Laparoscopy-assisted colectomy versus open colectomy for treatment of non-metastatic colon cancer: a randomised trial. Lancet 359:2224–2229
Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Pahlman L, Cuesta MA, Msika S, Morino M, Lacy AM, Group COcLoORS (2005) Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. The Lancet Oncol 6:477–484
Yamamoto S, Inomata M, Katayama H, Mizusawa J, Etoh T, Konishi F, Sugihara K, Watanabe M, Moriya Y, Kitano S, Japan Clinical Oncology Group Colorectal Cancer Study G (2014) Short-term surgical outcomes from a randomized controlled trial to evaluate laparoscopic and open D3 dissection for stage II/III colon cancer: Japan Clinical Oncology Group Study JCOG 0404. Ann Surg 260:23–30
Japanese Society for Cancer of the Colon and Rectum (2013) Japanese classification of colorectal carcinoma. The 8th edition. Kanehara & CO, LTD, Tokyo
Watanabe T, Itabashi M, Shimada Y, Tanaka S, Ito Y, Ajioka Y, Hamaguchi T, Hyodo I, Igarashi M, Ishida H, Ishihara S, Ishiguro M, Kanemitsu Y, Kokudo N, Muro K, Ochiai A, Oguchi M, Ohkura Y, Saito Y, Sakai Y, Ueno H, Yoshino T, Boku N, Fujimori T, Koinuma N, Morita T, Nishimura G, Sakata Y, Takahashi K, Tsuruta O, Yamaguchi T, Yoshida M, Yamaguchi N, Kotake K, Sugihara K, Japanese Society for Cancer of the C, Rectum (2015) Japanese Society for Cancer of the Colon and Rectum (JSCCR) Guidelines 2014 for treatment of colorectal cancer. Int J Clin Oncol 20:207–239
Morikawa E, Yasutomi M, Shindou K, Matsuda T, Mori N, Hida J, Kubo R, Kitaoka M, Nakamura M, Fujimoto K et al (1994) Distribution of metastatic lymph nodes in colorectal cancer by the modified clearing method. Dis Colon Rectum 37:219–223
Hida J, Yasutomi M, Maruyama T, Fujimoto K, Uchida T, Okuno K (1997) The extent of lymph node dissection for colon carcinoma: the potential impact on laparoscopic surgery. Cancer 80:188–192
West NP, Kobayashi H, Takahashi K, Perrakis A, Weber K, Hohenberger W, Sugihara K, Quirke P (2012) Understanding optimal colonic cancer surgery: comparison of Japanese D3 resection and European complete mesocolic excision with central vascular ligation. J Clin Oncol 30:1763–1769
Akiyoshi T, Kuroyanagi H, Fujimoto Y, Konishi T, Ueno M, Oya M, Yamaguchi T (2010) Short-term outcomes of laparoscopic colectomy for transverse colon cancer. J Gastrointest Surg 14:818–823
Yamamoto M, Okuda J, Tanaka K, Kondo K, Tanigawa N, Uchiyama K (2012) Clinical outcomes of laparoscopic surgery for advanced transverse and descending colon cancer: a single-center experience. Surg Endosc 26:1566–1572
Mulder SA, Kranse R, Damhuis RA, Ouwendijk RJ, Kuipers EJ, van Leerdam ME (2012) The incidence and risk factors of metachronous colorectal cancer: an indication for follow-up. Dis Colon Rectum 55:522–531
Battersby NJ, Coupland A, Bouliotis G, Mirza N, Williams JG (2014) Metachronous colorectal cancer: a competing risks analysis with consideration for a stratified approach to surveillance colonoscopy. J Surg Oncol 109:445–450
Fernandez-Cebrian JM, Gil Yonte P, Jimenez-Toscano M, Vega L, Ochando F (2013) Laparoscopic colectomy for transverse colon carcinoma: a surgical challenge but oncologically feasible. Colorectal Dis 15:e79–e83
Mistrangelo M, Allaix ME, Cassoni P, Giraudo G, Arolfo S, Morino M (2014) Laparoscopic versus open resection for transverse colon cancer. Surg Endosc. 29:2196–2202
Stelzner S, Hohenberger W, Weber K, West NP, Witzigmann H, Wedel T (2015) Anatomy of the transverse colon revisited with respect to complete mesocolic excision and possible pathways of aberrant lymphatic tumor spread. Int J Colorectal Dis. 31:377–84
Edge SBBD, Compton CC, Fritz AG, Greene FL, Trotti D (2010) AJCC cancer staging manual. Springer, New York
Koizumi M, Horiguchi M (1990) Accessory arteries supplying the human transverse colon. Acta Anat (Basel) 137:246–251
Amonoo-Kuofi HS, el-Badawi MG, el-Naggar ME (1995) Anomalous origins of colic arteries. Clin Anat 8:288–293
Kanda Y (2013) Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transpl 48:452–458
Feng B, Sun J, Ling TL, Lu AG, Wang ML, Chen XY, Ma JJ, Li JW, Zang L, Han DP, Zheng MH (2012) Laparoscopic complete mesocolic excision (CME) with medial access for right-hemi colon cancer: feasibility and technical strategies. Surg Endosc 26:3669–3675
Kim MK, Won DY, Lee JK, Kang WK, Kye BH, Cho HM, Kim HJ, Kim JG (2015) Laparoscopic surgery for transverse colon cancer: short- and long-term outcomes in comparison with conventional open surgery. J Laparoendosc Adv Surg Tech A 25:982–989
Kotake K, Mizuguchi T, Moritani K, Wada O, Ozawa H, Oki I, Sugihara K (2014) Impact of D3 lymph node dissection on survival for patients with T3 and T4 colon cancer. Int J Colorectal Dis 29:847–852
Storli KE, Sondenaa K, Furnes B, Nesvik I, Gudlaugsson E, Bukholm I, Eide GE (2013) Short term results of complete (D3) vs. standard (D2) mesenteric excision in colon cancer shows improved outcome of complete mesenteric excision in patients with TNM stages I–II. Tech Coloproctol. 18:557–564
Chang GJ, Rodriguez-Bigas MA, Skibber JM, Moyer VA (2007) Lymph node evaluation and survival after curative resection of colon cancer: systematic review. J Natl Cancer Inst 99:433–441
Toyota S, Ohta H, Anazawa S (1995) Rationale for extent of lymph node dissection for right colon cancer. Dis Colon Rectum 38:705–711
Bertelsen CA, Bols B, Ingeholm P, Jansen JE, Jepsen LV, Kristensen B, Neuenschwander AU, Gogenur I (2014) Lymph node metastases in the gastrocolic ligament in patients with colon cancer. Dis Colon Rectum 57:839–845
Perrakis A, Weber K, Merkel S, Matzel K, Agaimy A, Gebbert C, Hohenberger W (2014) Lymph node metastasis of carcinomas of transverse colon including flexures. Consideration of the extramesocolic lymph node stations. Int J Colorectal Dis 29:1223–1229
Ricciardi R, Baxter NN (2007) Association versus causation versus quality improvement: setting benchmarks for lymph node evaluation in colon cancer. J Natl Cancer Inst 99:414–415
Schlachta CM, Mamazza J, Poulin EC (2007) Are transverse colon cancers suitable for laparoscopic resection? Surg Endosc 21:396–399
Mori S, Kita Y, Baba K, Yanagi M, Tanabe K, Uchikado Y, Kurahara H, Arigami T, Uenosono Y, Mataki Y, Okumura H, Nakajo A, Maemura K, Natsugoe S (2017) Laparoscopic complete mesocolic excision via combined medial and cranial approaches for transverse colon cancer. Surg Today 47:643–649
Hirasaki Y, Fukunaga M, Sugano M, Nagakari K, Yoshikawa S, Ouchi M (2014) Short- and long-term results of laparoscopic surgery for transverse colon cancer. Surg Today 44:1266–1272
Yamaguchi S, Kuroyanagi H, Milsom JW, Sim R, Shimada H (2002) Venous anatomy of the right colon: precise structure of the major veins and gastrocolic trunk in 58 cadavers. Dis Colon Rectum 45:1337–1340
Spasojevic M, Stimec BV, Dyrbekk AP, Tepavcevic Z, Edwin B, Bakka A, Ignjatovic D (2013) Lymph node distribution in the d3 area of the right mesocolon: implications for an anatomically correct cancer resection. A postmortem study. Dis Colon Rectum 56:1381–1387
Clancy C, O’Leary DP, Burke JP, Redmond HP, Coffey JC, Kerin MJ, Myers E (2014) A meta-analysis to determine the oncological implications of conversion in laparoscopic colorectal cancer surgery: the official journal of the Association of Coloproctology of Great Britain and Ireland. Colorectal Dis. 17:482–490
Ignjatovic D, Sund S, Stimec B, Bergamaschi R (2007) Vascular relationships in right colectomy for cancer: clinical implications. Tech Coloproctol 11:247–250
Spasojevic M, Stimec BV, Fasel JF, Terraz S, Ignjatovic D (2011) 3D relations between right colon arteries and the superior mesenteric vein: a preliminary study with multidetector computed tomography. Surg Endosc 25:1883–1886
Spasojevic M, Stimec BV, Gronvold LB, Nesgaard JM, Edwin B, Ignjatovic D (2011) The anatomical and surgical consequences of right colectomy for cancer. Dis Colon Rectum 54:1503–1509
Acknowledgements
We thank Edanz Group (https://www.edanzediting.com/ac) for editing a draft of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Drs. Ueki, Nagai, Manabe, Koba, Nagayoshi, and Nakamura have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Ueki, T., Nagai, S., Manabe, T. et al. Vascular anatomy of the transverse mesocolon and bidirectional laparoscopic D3 lymph node dissection for patients with advanced transverse colon cancer. Surg Endosc 33, 2257–2266 (2019). https://doi.org/10.1007/s00464-018-6516-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-018-6516-2