Abstract
Objectives
Cricopharyngeus muscle dysfunction (CPMD) is a common cause for progressive dysphagia and can lead to dietary restriction, reduced nutrition, weight loss, and pneumonia. Controversy exists whether CPMD is best managed with primary surgical treatment of the cricopharyngeus muscle and who represents a good surgical candidate.
Methods
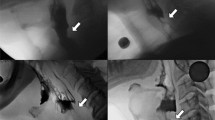
Retrospective review of patients diagnosed with CPMD who underwent surgical treatment were evaluated through prospectively collected pre- and postoperative Eating Assessment Tool-10 (EAT-10) and Functional Oral Intake Scale (FOIS). Videofluoroscopic swallowing studies (VFSS) were reviewed for presence or absence of a high-pressure barium stream through the upper esophageal sphincter, termed the jet phenomenon (JP).
Results
We identified 42 patients with CPMD who underwent surgical treatment and had serial Eating Assessment Tool (EAT-10) measures obtained pre- and postoperatively. Mean EAT-10 scores improved by 12.1 points (95%CI = 8.6–15.6), p < 0.0001. There was a significantly greater improvement among patients with JP (|∆EAT-10|= 17.0, 95%CI = 12.5–21.4) compared to those without (|∆EAT-10|= 6.2, 95%CI = 1.6–10.8), p = 0.0013. Patients with JP also showed improved FOIS score (p = 0.0023) while those without JP did not.
Conclusion
This study provides the initial report on the utility of JP as a VFSS feature that is strongly associated with improved outcomes following surgical treatment of CPMD. Further work determining the physiologic correlates responsible for JP will help clarify its predictive capabilities.
Level of Evidence
Level 3.

Similar content being viewed by others
References
Hoy M, Domer A, Plowman EK, Loch R, Belafsky P. Causes of dysphagia in a tertiary-care swallowing center. Ann Otol Rhinol Laryngol. 2013;122:335–8. https://doi.org/10.1177/000348941312200508.
Allen JE. Cricopharyngeal function or dysfunction: what’s the deal? Curr Opin Otolaryngol Head Neck Surg. 2016;24:494–9.
Yin T, Jardine M, Miles A, Allen J. What is a normal pharynx? A videofluoroscopic study of anatomy in older adults. Eur Arch Oto-Rhino-Laryngol. 2018;275:2317–23.
Kelly JH. Management of upper esophageal sphincter disorders: indications and complications of myotomy. Am J Med. 2000;108(Suppl 4a 4):43–6. https://doi.org/10.1016/S0002-9343(99)00334-4.
Knigge MA, Thibeault SL. Swallowing outcomes after cricopharyngeal myotomy: a systematic review. Head Neck. 2018;40:203–12. https://doi.org/10.1002/HED.24977.
Sanei-Moghaddam A, Kumar S, Jani P, Brierley C. Cricopharyngeal myotomy for cricopharyngeus stricture in an inclusion body myositis patient with hiatus hernia: a learning experience. BMJ Case Rep. 2013. https://doi.org/10.1136/bcr-2012-008058.
Triadafilopoulos G, Hallstone A, Nelson-Abbott H, Bedinger K. Oropharyngeal and esophageal interrelationships in patients with nonobstructive dysphagia. Dig Dis Sci. 1992;37:551–7. https://doi.org/10.1007/BF01307579.
Reedy EL, Herbert TL, Bonilha HS. Visualizing the esophagus during modified barium swallow studies: a systematic review. Am J Speech-Lang Pathol. 2021;30:761–71. https://doi.org/10.1044/2020_AJSLP-20-00255.
Nativ-Zeltzer N, Rameau A, Kuhn MA, Kaufman M, Belafsky PC. The relationship between hiatal hernia and cricopharyngeus muscle dysfunction. Dysphagia. 2019;34:391–6.
Benjamin T, Zackria S, Lopez R, Richter J, Thota PN. Upper esophageal sphincter abnormalities and high-resolution esophageal manometry findings in patients with laryngopharyngeal reflux. Scand J Gastroenterol. 2017;52:816–21. https://doi.org/10.1080/00365521.2017.1322139.
Balouch B, Vaid A, Vontela S, Alnouri G, Sataloff RT. Anatomic and manometric abnormalities of the upper and lower esophageal sphincters in patients with reflux disease. J Voice. 2022. https://doi.org/10.1016/J.JVOICE.2021.11.008.
Chavez YH, Ciarleglio MM, Clarke JO, Nandwani M, Stein E, Roland BC. Upper esophageal sphincter abnormalities: frequent finding on high-resolution esophageal manometry and associated with poorer treatment response in achalasia. J Clin Gastroenterol. 2015;49:17–23. https://doi.org/10.1097/MCG.0000000000000157.
Blais P, Bennett MC, Gyawali CP. Upper esophageal sphincter metrics on high-resolution manometry differentiate etiologies of esophagogastric junction outflow obstruction. Neurogastroenterol Motil. 2019. https://doi.org/10.1111/NMO.13558.
Henderson RD, Hanna WM, Henderson RF, Marryatt G. Myotomy for reflux-induced cricopharyngeal dysphagia: five year review. J Thorac Cardiovasc Surg. 1989;98:428–33.
Williams RBH, Ali GN, Hunt DR, Wallace KL, Cook IJ. Cricopharyngeal myotomy does not increase the risk of esophagopharyngeal acid regurgitation. Am J Gastroenterol. 1999;94:3448–54. https://doi.org/10.1111/j.1572-0241.1999.01507.x.
Allen J, White CJ, Leonard R, Belafsky PC. Effect of cricopharyngeus muscle surgery on the pharynx. Laryngoscope. 2010;120:1498–503.
Yip HT, Leonard R, Kendall KA. Cricopharyngeal myotomy normalizes the opening size of the upper esophageal sphincter in cricopharyngeal dysfunction. Laryngoscope. 2006;116:93–6. https://doi.org/10.1097/01.mlg.0000184526.89256.85.
Wu PI, Szczesniak MM, Omari T, Lam TY, Wong M, Maclean J, et al. Cricopharyngeal peroral endoscopic myotomy improves oropharyngeal dysphagia in patients with Parkinson’s disease. Endosc Int open. 2021;9:E1811–9. https://doi.org/10.1055/A-1562-7107.
Fong R, Rumbach AF, Ward EC, Doeltgen SH, Sun N, Tsang R. Videofluoroscopic and manometric outcomes of cricopharyngeus balloon dilation for treatment of pharyngo-esophageal dysphagia associated with nasopharyngeal cancer: a case series. Laryngoscope Investig Otolaryngol. 2021;6:1077–87. https://doi.org/10.1002/LIO2.641.
Kos MP, David EF, Klinkenberg-Knol EC, Mahieu HF. Long-term results of external upper esophageal sphincter myotomy for oropharyngeal dysphagia. Dysphagia. 2010;25:169. https://doi.org/10.1007/S00455-009-9236-X.
Knigge MA, Thibeault S. Relationship between tongue base region pressures and vallecular clearance. Dysphagia. 2016;31:391–7. https://doi.org/10.1007/S00455-015-9688-0.
Rosen SP, Jones CA, Hoffman MR, Knigge MA, McCulloch TM. Pressure abnormalities in patients with Zenker’s diverticulum using pharyngeal high-resolution manometry. Laryngoscope Investig Otolaryngol. 2020;5:708–17. https://doi.org/10.1002/LIO2.434.
Krekeler BN, Davidson K, Kantarcigil C, Pearson W, Blair J, Martin-Harris B. Determining swallowing biomechanics underlying modified barium swallow impairment profile scoring using computational analysis of swallowing mechanics. J Speech Lang Hear Res. 2022. https://doi.org/10.1044/2022_JSLHR-22-00047.
Hosseini P, Tadavarthi Y, Martin-Harris B, Pearson WG. Functional modules of pharyngeal swallowing mechanics. Laryngoscope Investig Otolaryngol. 2019;4:341–6. https://doi.org/10.1002/LIO2.273.
Randall DR, Chan R, Gomes D, Walker K. Natural history of cricopharyngeus muscle dysfunction symptomatology. Dysphagia. 2021. https://doi.org/10.1007/S00455-021-10355-8.
Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJPM, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. 2015;27:160–74. https://doi.org/10.1111/nmo.12477.
Crary MA, Carnaby Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86:1516–20. https://doi.org/10.1016/j.apmr.2004.11.049.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the eating assessment tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117:919–24. https://doi.org/10.1177/000348940811701210.
Belafsky PC, Rees CJ, Allen J, Leonard RJ. Pharyngeal dilation in cricopharyngeus muscle dysfunction and Zenker diverticulum. Laryngoscope. 2010;120:889–94.
Randall DR, Evangelista LM, Kuhn MA, Belafsky PC. Improved symptomatic, functional, and fluoroscopic outcomes following serial “series of three” double-balloon dilation for cricopharyngeus muscle dysfunction. J Otolaryngol—Head Neck Surg. 2018;47:35. https://doi.org/10.1186/s40463-018-0278-7.
Drazner MH. The progression of hypertensive heart disease. Circulation. 2011;123:327–34. https://doi.org/10.1161/CIRCULATIONAHA.108.845792.
Lee JW, Randall DR, Evangelista LM, Kuhn MA, Belafsky PC. Subjective assessment of videofluoroscopic swallow studies. Otolaryngol—Head Neck Surg (United States). 2017;156:901–5. https://doi.org/10.1177/0194599817691276.
Cock C, Omari T. Diagnosis of swallowing disorders: how we interpret pharyngeal manometry. Curr Gastroenterol Rep. 2017. https://doi.org/10.1007/S11894-017-0552-2.
Berg HM, Persky MS, Jacobs JB, Cohen NL. Cricopharyngeal myotomy: a review of surgical results in patients with cricopharyngeal achalasia of neurogenic origin. Laryngoscope. 1985;95:1337–40. https://doi.org/10.1288/00005537-198511000-00008.
Ozgursoy OB, Salassa JR. Manofluorographic and functional outcomes after endoscopic laser cricopharyngeal myotomy for cricopharyngeal bar. Otolaryngol—Head Neck Surg (United States). 2010;142:735–40. https://doi.org/10.1016/j.otohns.2009.08.020.
Ali GN, Wallace KL, Laundl TM, Hunt DR, DeCarle DJ, Cook IJ. Predictors of outcome following cricopharyngeal disruption for pharyngeal dysphagia. Dysphagia. 1997;12:133–9. https://doi.org/10.1007/PL00009527.
Ren Y, Tang X, Chen F, Deng Z, Wu J, Nei S, et al. Myotomy of distal esophagus influences proximal esophageal contraction and upper esophageal sphincter relaxation in patients with achalasia after peroral endoscopic myotomy. J Neurogastroenterol Motil. 2016;22:78–85. https://doi.org/10.5056/JNM15098.
Acknowledgements
The authors acknowledge the mentors, colleagues, and collaborators within the physician and speech language pathology practices from whom we have had the opportunity to learn, and from which we were introduced to the jet phenomenon term and its role in dysphagia assessment. We did not create the term and cannot determine who the first person to do so was, so this manuscript acknowledges his or her keen observation and the subsequent collective knowledge.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Randall, D.R., Young-Speirs, M. & Walker, K. Association of the “Jet Phenomenon” with Positive Symptom Outcome Following Surgical Treatment of Cricopharyngeus Muscle Dysfunction. Dysphagia 38, 1440–1446 (2023). https://doi.org/10.1007/s00455-023-10573-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-023-10573-2