Abstract
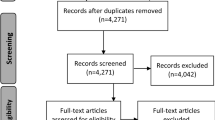
Puree is commonly prescribed for patients with mastication and bolus formation difficulties, but its appearance might negatively impact appetite and intake. Molded puree is marketed to be an alternative to traditional puree, but the process of molding puree could alter the properties of the food significantly and lead to different swallowing physiology as compared to puree. The current study investigated the differences between traditional and molded puree in terms of swallowing physiology and perception in healthy individuals. Thirty two participants were included. Two outcomes were used to quantify the oral preparatory and oral phase. Fibreoptic endoscopic evaluation of swallowing was used to assess the pharyngeal phase as it could retain the purees in their original form. Six outcomes were collected. Perceptual rating of the purees were provided by participants in six domains. Molded puree required significantly more masticatory cycles (p < 0.001) and longer time for ingestion (p < 0.001). Molded puree had longer swallow reaction time (p = 0.001) and more inferior site of swallow initiation (p = 0.007) compared with traditional puree. Participants’ satisfaction with the appearance, texture and overall of molded puree was significantly greater. Molded puree was perceived to be more difficult to chew and swallow. This study established that the two types of puree were different in various aspects. The study also provided important clinical implications regarding the use of molded puree as a form of texture modified diet (TMD) in patients with dysphagia. The results could serve as the foundation of larger cohort studies on the effect of various TMDs on patients with dysphagia.


Similar content being viewed by others
References
Steele CM, Alsanei WA, Ayanikalath S, Barbon CE, Chen J, Cichero JA, et al. The influence of food texture and liquid consistency modification on swallowing physiology and function: a systematic review. Dysphagia. 2015;30(1):2–26. https://doi.org/10.1007/s00455-014-9578-x.
Perlman PW, Cohen MA, Setzen M, Belafsky PC, Guss J, Mattucci KF, et al. The risk of aspiration of pureed food as determined by flexible endoscopic evaluation of swallowing with sensory testing. Otolaryngol Head Neck Surg. 2004;130(1):80–3. https://doi.org/10.1016/j.otohns.2003.09.026.
Nowson CA, Sherwin AJ, McPhee JG, Wark JD, Flicker L. Energy, protein, calcium, vitamin D and fibre intakes from meals in residential care establishments in Australia. Asia Pac J Clin Nutr. 2003;12(2):172–7.
Dick A, Bhandari B, Dong X, Prakash S. Feasibility study of hydrocolloid incorporated 3D printed pork as dysphagia food. Food Hydrocoll. 2020;107:105940. https://doi.org/10.1016/j.foodhyd.2020.105940.
Smith R, Bryant L, Reddacliff C, Hemsley B. A review of the impact of food design on the mealtimes of people with swallowing disability who require texture-modified food. International Journal of Food Design. 2022;7(1):7–28. https://doi.org/10.1386/ijfd_00034_1.
Smith R, Bryant L, Hemsley B. Allied health professionals’ views on the use of 3D food printing to improve the mealtime quality of life for people with dysphagia: impact, cost, practicality, and potential. Am J Speech Lang Pathol. 2022;31(4):1868–77. https://doi.org/10.1044/2022_ajslp-21-00391.
Pu D, Choi YY, Chan KM, Poon MM. Modifying puree meals in residential aged care facilities: a multi-centre feasibility and acceptability study. Geriatrics (Basel). 2021;6(4):108. https://doi.org/10.3390/geriatrics6040108.
MyCareHealthcare. 2022. https://mch.hk. Accessed 22 June 2022.
Cassens D, Johnson E, Keelan S. Enhancing taste, texture, appearance, and presentation of pureed food improved resident quality of life and weight status. Nutr Rev. 1996;54(1 2):S51–4. https://doi.org/10.1111/j.1753-4887.1996.tb03790.x.
Stahlman LB, Garcia JM, Et C, Smit AB, Hoag L, Chambers DH. Perceptual ratings for pureed and molded peaches for individuals with and without impaired swallowing. Dysphagia. 2001;16(4):254–62. https://doi.org/10.1007/s00455-001-0084-6.
Strother H, Moss R, McSweeney MB. Comparison of 3D printed and molded carrots produced with gelatin, guar gum and xanthan gum. J Texture Stud. 2020;51(6):852–60. https://doi.org/10.1111/jtxs.12545.
St.James’Settlement. Graceful Meal. 2022. https://www.sjscafe.com/pages/gm?locale=en. Accessed 30 June 2022.
Wong Y. Nutritious Puree - “Fine dining” for the elderly. 2020. https://www.healthyd.com/articles/expert-blog/營養糊餐-院舍精緻糊餐-體弱長者的fine-dining. Accessed 30 June 2022.
Kwan K. Thoughtful puree - View from the professional. 2020. https://ol.mingpao.com/ldy/cultureleisure/culture/20201116/1605466132875/專家札記-貼心軟餐-別致造型開胃口. Accessed 30 June 2022.
Beck AM, Kjaersgaard A, Hansen T, Poulsen I. Systematic review and evidence based recommendations on texture modified foods and thickened liquids for adults (above 17 years) with oropharyngeal dysphagia—An updated clinical guideline. Clin Nutr. 2018;37(6):1980–91. https://doi.org/10.1016/j.clnu.2017.09.002.
Belafsky PC, Mouadeb DA, Rees CJ, Pryor JC, Postma GN, Allen J, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol. 2008;117(12):919–24. https://doi.org/10.1177/000348940811701210.
Groher ME. Dysphagia : clinical management in adults and children. In: Crary MA, editor. Third edition ed. St. Louis: Mosby; 2020.
Cichero JA, Lam P, Steele CM, Hanson B, Chen J, Dantas RO, et al. Development of international terminology and definitions for texture-modified foods and thickened fluids used in dysphagia management: the IDDSI framework. Dysphagia. 2017;32(2):293–314. https://doi.org/10.1007/s00455-016-9758-y.
Langmore SE. History of fiberoptic endoscopic evaluation of swallowing for evaluation and management of pharyngeal dysphagia: changes over the years. Dysphagia. 2017;32(1):27–38. https://doi.org/10.1007/s00455-016-9775-x.
Costa MM. Videofluoroscopy: the gold standard exam for studying swallowing and its dysfunction. Arq Gastroenterol. 2010;47(4):327–8. https://doi.org/10.1590/s0004-28032010000400001.
Dietsch AM, Solomon NP, Steele CM, Pelletier CA. The effect of barium on perceptions of taste intensity and palatability. Dysphagia. 2014;29(1):96–108. https://doi.org/10.1007/s00455-013-9487-4.
Prikladnicki A, Santana MG, Cardoso MC. Protocols and assessment procedures in fiberoptic endoscopic evaluation of swallowing: an updated systematic review. Braz J Otorhinolaryngol. 2021. https://doi.org/10.1016/j.bjorl.2021.03.002.
Humbert IA, Sunday KL, Karagiorgos E, Vose AK, Gould F, Greene L, et al. Swallowing kinematic differences across frozen, mixed, and ultrathin liquid boluses in healthy adults: age, sex, and normal variability. J Speech Lang Hear Res. 2018;61(7):1544–59. https://doi.org/10.1044/2018_JSLHR-S-17-0417.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11(2):93–8.
Mozzanica F, Lorusso R, Robotti C, Zambon T, Corti P, Pizzorni N, et al. Effect of age, sex, bolus volume, and bolus consistency on whiteout duration in healthy subjects during FEES. Dysphagia. 2019;34(2):192–200. https://doi.org/10.1007/s00455-018-9961-0.
Neubauer PD, Rademaker AW, Leder SB. The yale pharyngeal residue severity rating scale: an anatomically defined and image-based tool. Dysphagia. 2015;30(5):521–8. https://doi.org/10.1007/s00455-015-9631-4.
Huckabee ML, McIntosh T, Fuller L, Curry M, Thomas P, Walshe M, et al. The Test of Masticating and Swallowing Solids (TOMASS): reliability, validity and international normative data. Int J Lang Commun Disord. 2018;53(1):144–56. https://doi.org/10.1111/1460-6984.12332.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–90. https://doi.org/10.1037//1040-3590.6.4.284.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74. https://doi.org/10.2307/2529310.
Steele CM, Grace-Martin K. Reflections on clinical and statistical use of the penetration-aspiration scale. Dysphagia. 2017;32(5):601–16. https://doi.org/10.1007/s00455-017-9809-z.
Saha D, Bhattacharya S. Hydrocolloids as thickening and gelling agents in food: a critical review. J Food Sci Technol. 2010;47(6):587–97. https://doi.org/10.1007/s13197-010-0162-6.
Tu J, Brennan M, Brennan C. An insight into the mechanism of interactions between mushroom polysaccharides and starch. Curr Opin Food Sci. 2021;37:17–25. https://doi.org/10.1016/j.cofs.2020.07.005.
Watanabe Y, Hirano H, Arai H, Morishita S, Ohara Y, Edahiro A, et al. Relationship between frailty and oral function in community-dwelling elderly adults. J Am Geriatr Soc. 2017;65(1):66–76. https://doi.org/10.1111/jgs.14355.
Cioncoloni D, Casali S, Ginanneschi F, Carone M, Veronica B, Rossi A, et al. Major motor-functional determinants associated with poor self-reported health-related quality of life in myasthenia gravis patients. Neurol Sci. 2016;37(5):717–23. https://doi.org/10.1007/s10072-016-2556-3.
Logemann JA. Evaluation and treatment of swallowing disorders. Austin: PRO-ED; 1995.
Martin-Harris B, Brodsky MB, Michel Y, Lee FS, Walters B. Delayed initiation of the pharyngeal swallow: normal variability in adult swallows. J Speech Lang Hear Res. 2007;50(3):585–94. https://doi.org/10.1044/1092-4388(2007/041).
Namasivayam-MacDonald AM, Alomari N, Attner L, Benjamin RD, Chill A, Doka S, et al. A retrospective analysis of swallowing function and physiology in patients living with dementia. Dysphagia. 2022;37(4):900–8. https://doi.org/10.1007/s00455-021-10350-z.
Gandhi P, Mancopes R, Sutton D, Plowman EK, Steele CM. The Frequency of atypical and extreme values for pharyngeal phase swallowing measures in mild parkinson disease compared to healthy aging. J Speech Lang Hear Res. 2021;64(8):3032–50. https://doi.org/10.1044/2021_JSLHR-21-00084.
Acknowledgements
The authors would like to thank all participants and helpers who assisted with participant recruitment.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wong, M.K.L., Ku, P.K.M., Tong, M.C.F. et al. Endoscopic and observational findings of swallowing of traditional and molded puree in healthy individuals. Dysphagia 38, 1363–1370 (2023). https://doi.org/10.1007/s00455-023-10565-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-023-10565-2