Abstract
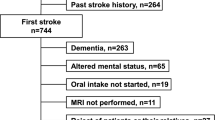
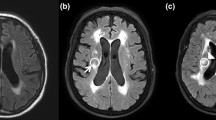
Oropharyngeal dysphagia is a highly prevalent post-stroke complication commonly associated with topographically specific gray-matter damage. In contrast, the role of damage to the extensive white matter brain network (leukoaraiosis) in post-stroke oropharyngeal dysphagia has not yet been clarified. We aim to assess the role of leukoaraiosis in post-stroke oropharyngeal dysphagia. We designed a cross-sectional study and retrospectively collected from our database patients with dysphagia affected by a recent stroke and on whom both a brain 1.5 T-MRI and a videofluoroscopy had been performed. Leukoaraiosis was assessed in brainstem and in cerebral regions (periventricular or deep) with Fazekas scale. Penetration-Aspiration-Scale and time to laryngeal vestibule closure and to upper esophageal sphincter opening were analyzed. Study population (n = 121; 57% men, 75.5 ± 9.4y) presented mostly supratentorial ischemic PACI-type strokes. Of the patients, 86% had unsafe swallows (PAS = 3.97 ± 2.04); 94.2% had cerebral leukoaraiosis (Fazekas = 3.36 ± 1.7) and 42.1% had brainstem-leukoaraiosis, hypertension being the main risk factor. We found both significant positive associations between degree of periventricular-leukoaraiosis and total-leukoaraiosis and presence of risk of aspirations (p = 0.016 and p = 0.023, respectively); and a correlation between periventricular-leukoaraiosis and PAS scale severity (r = 0.179, p = 0.049). No correlations/associations were found between stroke volume and dysphagia in this study. Our study supports a role for leukoaraiosis in the pathophysiology of dysphagia. Stroke is associated with chronic short-connection/circuit injury and damage to periventricular white matter long connections is a relevant neuro-pathophysiological mechanism contributing to impaired safety of swallow in post-stroke oropharyngeal dysphagia patients.



Similar content being viewed by others
References
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–63. https://doi.org/10.1161/01.STR.0000190056.76543.eb.
Rofes L, Muriana D, Palomeras E, et al. Prevalence, risk factors and complications of oropharyngeal dysphagia in stroke patients: a cohort study. Neurogastroenterol Motil. 2018;30:1–10. https://doi.org/10.1111/nmo.13338.
Clave PSR. Dysphagia: current reality and scope of the problem. Nat Rev Gastroenterol Hepatol. 2015. https://doi.org/10.1038/nrgastro.2015.49.
Vilardell N, Rofes L, Arreola V, et al. Videofluoroscopic assessment of the pathophysiology of chronic poststroke oropharyngeal dysphagia. Neurogastroenterol Motil. 2017. https://doi.org/10.1111/nmo.13111.
Cabib C, Ortega O, Vilardell N, Mundet L, Clavé P, Rofes L. Chronic post-stroke oropharyngeal dysphagia is associated with impaired cortical activation to pharyngeal sensory inputs. Eur J Neurol. 2017. https://doi.org/10.1111/ene.13392.
Cabib C, Nascimento W, Rofes L, Arreola V, Tomsen N, Mundet L (2019) Neurophysiological and Biomechanical Evaluation of the Mechanisms Which Impair Safety of Swallow in Chronic Post-stroke Patients. Transl stroke Res.
Cabib C, Ortega O, Kumru H, et al. Neurorehabilitation strategies for poststroke oropharyngeal dysphagia: from compensation to the recovery of swallowing function. Ann N Y Acad Sci. 2016;1380:121–38. https://doi.org/10.1111/nyas.13135.
Hamdy S, Aziz Q, Thompson DG, Rothwell JC. Physiology and pathophysiology of the swallowing area of human motor cortex. Neural Plast. 2001;8:91–7. https://doi.org/10.1155/NP.2001.91.
Eltringham SA, Kilner K, Gee M, et al. Impact of Dysphagia Assessment and Management on Risk of Stroke-Associated Pneumonia: A Systematic Review. Cerebrovasc Dis. 2018;46:97–105. https://doi.org/10.1159/000492730.
Prins ND, Scheltens P. White matter hyperintensities, cognitive impairment and dementia: an update. Nat Rev Neurol. 2015;11:157–65. https://doi.org/10.1038/NRNEUROL.2015.10.
Alberts MJ, Horner J, Gray L, Brazer SR (1992) Aspiration after stroke: lesion analysis by brain MRI. Dysphagia 7(3):170–3).
Cola MG, Daniels SK, Corey DM, Lemen LC, Romero M, Foundas AL. Relevance of subcortical stroke in dysphagia. Stroke. 2010;41:482–6. https://doi.org/10.1161/STROKEAHA.109.566133.
Mihai PG, Otto M, Domin M, Platz T, Hamdy S, Lotze M. Brain imaging correlates of recovered swallowing after dysphagic stroke: a fMRI and DWI study. Neuroimage. 2016;12:1013–21. https://doi.org/10.1016/J.NICL.2016.05.006.
Moon HI, Nam JS, Leem MJ, Kim KH. Periventricular white matter lesions as a prognostic factor of swallowing function in older patients with mild stroke. Dysphagia. 2017;32:480–6. https://doi.org/10.1007/S00455-017-9788-0.
Galovic M, Leisi N, Pastore-Wapp M, et al. Diverging lesion and connectivity patterns influence early and late swallowing recovery after hemispheric stroke. Hum Brain Mapp. 2017;38:2165–76. https://doi.org/10.1002/HBM.23511.
Fandler S, Gattringer T, Eppinger S, et al. Frequency and predictors of dysphagia in patients with recent small subcortical infarcts. Stroke. 2017;48:213–5. https://doi.org/10.1161/STROKEAHA.116.015625.
Wilmskoetter J, Bonilha L, Martin-Harris B, Elm JJ, Horn J, Bonilha HS. Mapping acute lesion locations to physiological swallow impairments after stroke. Neuroimage. 2019. https://doi.org/10.1016/J.NICL.2019.101685.
Fazekas F, Chawluk J, Alavi A, Hurtig H, Zimmerman R. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987;149:351–6. https://doi.org/10.2214/ajr.149.2.351.
Alvar A, Hahn Arkenberg R, McGowan B, Cheng H, Malandraki GA. The role of white matter in the neural control of swallowing: a systematic review. Front Hum Neurosci. 2021. https://doi.org/10.3389/fnhum.2021.628424.
Van Swieten JC, Koudstaal PJ, Visser MC, Schouten H, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7. https://doi.org/10.1161/01.STR.19.5.604.
Bamford J, Sandercock P, Dennis M, Warlow C, Burn J. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet. 1991;337:1521–6. https://doi.org/10.1016/0140-6736(91)93206-O.
Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996;11:93–8.
Rofes L, Arreola V, Romea M, et al. Pathophysiology of oropharyngeal dysphagia in the frail elderly. Neurogastroenterol Motil. 2010;22:1–9. https://doi.org/10.1111/j.1365-2982.2010.01521.x.
Rofes L, Arreola V, López I, et al. Effect of surface sensory and motor electrical stimulation on chronic poststroke oropharyngeal dysfunction. Neurogastroenterol Motil. 2013;25:888–96. https://doi.org/10.1111/nmo.12211.
Bolivar-Prados M (2019) ESSD labelling system, comparison vs other systems. European Society for Swallowing Disorders 9th Congress, Vienna.
Arreola V, Ortega O, Álvarez-Berdugo D, et al. Effect of transcutaneous electrical stimulation in chronic poststroke patients with oropharyngeal dysphagia: 1-year results of a randomized controlled trial. Neurorehabil Neural Repair. 2021. https://doi.org/10.1177/15459683211023187.
Griffanti L, Jenkinson M, Suri S, et al. Classification and characterization of periventricular and deep white matter hyperintensities on MRI: a study in older adults. Neuroimage. 2018;170:174–81. https://doi.org/10.1016/J.NEUROIMAGE.2017.03.024.
Giralt-Steinhauer E, Medrano S, Soriano-Tárraga C, et al. Brainstem leukoaraiosis independently predicts poor outcome after ischemic stroke. Eur J Neurol. 2018;25:1086–92. https://doi.org/10.1111/ENE.13659.
Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27:1304–5. https://doi.org/10.1161/01.STR.27.8.1304.
Paciaroni M, Mazzotta G, Corea F, et al. Dysphagia following stroke. Eur Neurol. 2014;51:162–7. https://doi.org/10.1159/000077663.
Cabral J, Kringelbach ML, Deco G. Functional connectivity dynamically evolves on multiple time-scales over a static structural connectome: models and mechanisms. Neuroimage. 2017;160:84–96. https://doi.org/10.1016/J.NEUROIMAGE.2017.03.045.
Toscano M, Cecconi E, Capiluppi E, et al. Neuroanatomical, clinical and cognitive correlates of post-stroke dysphagia. Eur Neurol. 2015;74:171–7. https://doi.org/10.1159/000441056.
de Groot JC, de Leeuw FE, Oudkerk M, et al. Periventricular cerebral white matter lesions predict rate of cognitive decline. Ann Neurol. 2002;52:335–41. https://doi.org/10.1002/ANA.10294.
Pantoni L, Fierini F, Poggesi A, LADIS Study Group. Impact of cerebral white matter changes on functionality in older adults: an overview of the LADIS Study results and future directions. Geri Geron Int. 2015;15:10–6. https://doi.org/10.1111/GGI.12665.
Bolandzadeh N, Davis JC, Tam R, Handy TC, Liu-Ambrose T. The association between cognitive function and white matter lesion location in older adults: a systematic review. BMC Neurol. 2012. https://doi.org/10.1186/1471-2377-12-126.
Jo SY, Hwang JW, Pyun SB. Relationship between cognitive function and dysphagia after stroke. Ann Rehabil Med. 2017;41:564–72. https://doi.org/10.5535/ARM.2017.41.4.564.
Hamdy S, Aziz Q, Rothwell JC, Hobson A, Barlow J, Thompson DG. Cranial nerve modulation of human cortical swallowing motor pathways. Am J Physiol. 1997;272:G802–8. https://doi.org/10.1152/ajpgi.1997.272.4.G802.
Acknowledgements
Assistance with data collection received from Laura Bonamusa, statistical help received from Elisabet Palomeras and Jane Lewis for English editing assistance.
Funding
This study was supported by research grants from: Investigación Clínica Independiente, Instituto de Salud Carlos III (ICI20/00117); CIBERehd, Acción Estratégica en Disfagia, Instituto de Salud Carlos III (EHD20PI02); Fondo de Investigaciones Sanitarias, Instituto de Salud Carlos III (PI18/00241); and The Territorial Competitiveness Specialization Project (PECT) of Mataro-Maresme (PRE/161/2019) financed by the Government of Catalunya-Generalitat de Catalunya within the framework of the European Regional Developments Funds of Catalonia Operational Programme 2014–2020.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the submitted manuscript. C. Cabib, O. Ortega, P. Clavé and N. Guanyabens have participate on design, analysis and writing the manuscript, while A. Ungueti, M Duh and M. Fernandez have performed the interpretation of radiologic data and helped with the writing and revision. V. Arreola and W. Do Nascimento help to get and analyze the VFS data as well as revise and contribute with final version of the document. At last E. Palomeras, have participated in drafting the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics Approval
The study protocol was approved by the Ethical Committee of the Hospital de Mataró (CEIm 27/19).
Informed Consent
It is a retrospective observational study, based on usual clinical practice, so the informed consent is not available.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guanyabens, N., Cabib, C., Ungueti, A. et al. The Impact of Periventricular Leukoaraiosis in Post-stroke Oropharyngeal Dysphagia: A Swallowing Biomechanics and MRI-Based Study. Dysphagia 38, 856–865 (2023). https://doi.org/10.1007/s00455-022-10509-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10509-2