Abstract
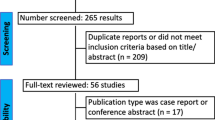
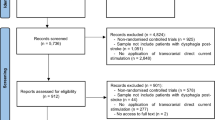
Transcranial stimulation has been proposed as an alternative rehabilitation therapy for adults with post-stroke dysphagia (PSD). This systematic review sought to determine the effectiveness of transcranial stimulation in patients with post-stroke dysphagia to improve swallowing function. From inception to January 3, 2021, an extensive search was conducted in PubMed, EMBASE, Cochrane, CINAHL, and Scopus, Web of Science. The randomized controlled trials (RCTs) included studies in adults aged 18 years and older who suffered from post-stroke dysphagia. Using Hedges' g as effect size, meta-analyses were conducted using random-effects models. To investigate potential sources of heterogeneity, subgroup analyses, and multivariable meta-regression analyses were conducted. Sixteen RCTs were included in this review, and 13 RCTs were used for meta-analysis. The meta-analysis showed that a large effect size in improving swallowing function after repetitive Transcranial Magnetic Stimulation (g = − 0.86, 95% CI – 1.57, − 0.16) and medium effect size in Transcranial Direct Current Stimulation (g = − 0.61, 95% CI − 1.04, − 0.17) at post-intervention, respectively. Subgroup and meta-regression analysis indicated that stimulation of the esophagus cortical area and middle-aged adults had a greater effect on swallowing function. The overall certainty of evidence assessed using the GRADE approach was low. Despite the positive results, transcranial stimulation requires additional research to reach definitive conclusions about the optimal stimulation protocol and to achieve the greatest benefit. Future trials should be more rigorous and include a larger sample size to demonstrate the efficacy of transcranial stimulation. Transcranial stimulation enables a more efficacious approach to dysphagia mitigation in PSD rehabilitation.




Similar content being viewed by others
References
Johnson W, Onuma O, Owolabi M, Sachdev S. Stroke: a global response is needed. Bull World Health Organ. 2016;94:634–634.
Chilukuri P, Odufalu F, Hachem C. Dysphagia. Mo Med. 2018;115(3):206–10.
Banasik JL, Copstead L-EC. Pathophysiology. 6th ed. Saunders: Elsevier; 2018.
Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke. Stroke. 2005;36(12):2756–63.
Armstrong JR, Mosher BD. Aspiration pneumonia after stroke: intervention and prevention. Neurohospitalist. 2011;1(2):85–93.
Bouziana SD, Tziomalos K. Malnutrition in patients with acute stroke. J Nutr Metab. 2011;2011:167898.
Cohen DL, Roffe C, Beavan J, et al. Post-stroke dysphagia: a review and design considerations for future trials. Int J Stroke. 2016;11(4):399–411.
Easterling C. 25 Years of dysphagia rehabilitation: what have we done, what are we doing, and where are we going? Dysphagia. 2017;32(1):50–4.
Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018. https://doi.org/10.1002/14651858.CD000323.pub3.
González-Fernández M, Ottenstein L, Atanelov L, Christian AB. Dysphagia after stroke: an overview. Curr Phys Med Rehabil Rep. 2013;1(3):187–96.
Albizu A, Indahlastari A, Woods AJ. Non-invasive brain stimulation. In: Gu D, Dupre ME, editors. Encyclopedia of gerontology and population aging. Cham: Springer International Publishing; 2019. p. 1–8.
Hosp JA, Luft AR. Cortical plasticity during motor learning and recovery after ischemic stroke. Neural Plast. 2011;2011:871296.
Mondino M, Bennabi D, Poulet E, Galvao F, Brunelin J, Haffen E. Can transcranial direct current stimulation (tDCS) alleviate symptoms and improve cognition in psychiatric disorders? World J Biol Psychiatry. 2014;15(4):261–75.
Fitzgerald PB, Fountain S, Daskalakis ZJ. A comprehensive review of the effects of rTMS on motor cortical excitability and inhibition. Clin Neurophysiol. 2006;117(12):2584–96.
Nitsche MA, Cohen LG, Wassermann EM, et al. Transcranial direct current stimulation: state of the art 2008. Brain Stimul. 2008;1(3):206–23.
Chail A, Saini R, Bhat P, Srivastava K, Chauhan V. Transcranial magnetic stimulation: a review of its evolution and current applications. Ind Psychiatry J. 2018;27(2):172–80.
Lefaucheur J-P. Chapter 37—Transcranial magnetic stimulation. In: Levin KH, Chauvel P, editors. Handbook of clinical neurology, vol. 160. Elsevier; 2019. p. 559–80.
Nitsche MA, Paulus W. Excitability changes induced in the human motor cortex by weak transcranial direct current stimulation. J Physiol. 2000;527(3):633–9.
Matsumoto H, Ugawa Y. Adverse events of tDCS and tACS: a review. Clin Neurophysiol Pract. 2017;2:19–25.
Robbins J, Butler SG, Daniels SK, et al. Swallowing and dysphagia rehabilitation: translating principles of neural plasticity into clinically oriented evidence. J Speech Lang Hear Res. 2008;51(1):S276–300.
Wang H-Y, Crupi D, Liu J, et al. Repetitive transcranial magnetic stimulation enhances BDNF–TrkB signaling in both brain and lymphocyte. J Neurosci. 2011;31(30):11044–54.
Kim D-Y, Park H-S, Park S-W, Kim J-H. The impact of dysphagia on quality of life in stroke patients. Medicine. 2020. https://doi.org/10.1097/MD.0000000000021795.
Ekberg O, Hamdy S, Woisard V, Wuttge-Hannig A, Ortega P. Social and psychological burden of dysphagia: its impact on diagnosis and treatment. Dysphagia. 2002;17(2):139–46.
Cheng I, Sasegbon A, Hamdy S. Effects of neurostimulation on poststroke dysphagia: a synthesis of current evidence from randomized controlled trials. Neuromodulation. 2020. https://doi.org/10.1111/ner.13327.
Pisegna JM, Kaneoka A, Pearson WG Jr, Kumar S, Langmore SE. Effects of non-invasive brain stimulation on post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. Clin Neurophysiol. 2016;127(1):956–68.
Marchina S, Pisegna JM, Massaro JM, et al. Transcranial direct current stimulation for post-stroke dysphagia: a systematic review and meta-analysis of randomized controlled trials. J Neurol. 2021;268(1):293–304.
Yang SN, Pyun SB, Kim HJ, Ahn HS, Rhyu BJ. Effectiveness of non-invasive brain stimulation in dysphagia subsequent to stroke: a systemic review and meta-analysis. Dysphagia. 2015;30(4):383–91.
Chiang CF, Lin MT, Hsiao MY, Yeh YC, Liang YC, Wang TG. Comparative efficacy of noninvasive neurostimulation therapies for acute and subacute poststroke dysphagia: a systematic review and network meta-analysis. Arch Phys Med Rehabil. 2019;100(4):739-750.e734.
Liao X, Xing G, Guo Z, et al. Repetitive transcranial magnetic stimulation as an alternative therapy for dysphagia after stroke: a systematic review and meta-analysis. Clin Rehabil. 2017;31(3):289–98.
Bath PM, Lee HS, Everton LF. Swallowing therapy for dysphagia in acute and subacute stroke. Cochrane Database Syst Rev. 2018;10(10):Cd000323.
Dionísio A, Duarte IC, Patrício M, Castelo-Branco M. Transcranial magnetic stimulation as an intervention tool to recover from language, swallowing and attentional deficits after stroke: a systematic review. Cerebrovasc Dis. 2018;46(3–4):176–83.
Sebastianelli L, Versace V, Martignago S, et al. Low-frequency rTMS of the unaffected hemisphere in stroke patients: a systematic review. Acta Neurol Scand. 2017;136(6):585–605.
Gorelick PB. The global burden of stroke: persistent and disabling. Lancet Neurol. 2019;18(5):417–8.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
The EndNote Team. EndNote. EndNote. X9 ed. Philadelphia, PA: Clarivate; 2013.
Li T, Higgins JPT, Deeks JJ. Chapter 5: Collecting data. Cochrane. Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019) Web site. https://training.cochrane.org/handbook/current/chapter-05. Published 2019. Accessed 3 Jan 2021.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res. 2005;5(1):13.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res. 2014;14(1):135.
Higgins JPT, Altman DG, Gøtzsche PC, et al. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343:d5928.
Fleiss JL, Levin B, Paik MC. Statistical methods for rates and proportions. New York: Wiley; 2013.
Stata: Release 16. [computer program]. College Station, TX: StataCorp LLC2019.
Rosenthal R, Cooper H, Hedges L. Parametric measures of effect size. The Handbook of Research Synthesis. 1994;621(2):231–44.
Hedges LV, Olkin I. Statistical methods for meta-analysis. Cambridge: Academic Press; 2014.
Jackson D, White IR, Thompson SG. Extending DerSimonian and Laird’s methodology to perform multivariate random effects meta-analyses. Stat Med. 2010;29(12):1282–97.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions version 6.0 (updated July 2019). The Cochrane Collaboration. www.handbook.cochrane.org. Published 2019. Accessed 3 Jan 2021.
Richardson M, Garner P, Donegan S. Interpretation of subgroup analyses in systematic reviews: a tutorial. Clin Epidemiology Glob Health. 2019;7(2):192–8.
Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions. In: The Cochrane Collaboration2011: http://training.cochrane.org/handbook. Accessed 3 Jan 2021.
Borenstein M, Higgins J. Meta-analysis and subgroups. Prev Sci. 2013;14(2):134–43.
Ranganathan P, Pramesh CS, Aggarwal R. Common pitfalls in statistical analysis: logistic regression. Perspect Clin Res. 2017;8(3):148–51.
GRADEpro Guideline Development Tool [computer program]. McMaster University and Evidence Prime Inc; 2020.
Schünemann H, Higgins J, Vist G, et al. Chapter 14: Completing ‘Summary of Findings’ tables and grading the certainty of the evidence. https://training.cochrane.org/handbook/current/chapter-14#_Ref419904527. Published 2020. Accessed 3 Jan 2021.
Shi L, Lin L. The trim-and-fill method for publication bias: practical guidelines and recommendations based on a large database of meta-analyses. Medicine. 2019. https://doi.org/10.1097/MD.0000000000015987.
Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Terrin N, Schmid CH, Lau J, Olkin I. Adjusting for publication bias in the presence of heterogeneity. Stat Med. 2003;22(13):2113–26.
Pustejovsky JE, Rodgers MA. Testing for funnel plot asymmetry of standardized mean differences. Res Synth Methods. 2019;10(1):57–71.
Schwarzer G, Carpenter J, Rücker G. Empirical evaluation suggests Copas selection model preferable to trim-and-fill method for selection bias in meta-analysis. J Clin Epidemiol. 2010;63(3):282–8.
Copas J. What works?: Selectivity models and meta-analysis. J R Stat Soc Ser A Stat Soc. 1999;162(1):95–109.
Ahn YH, Sohn HJ, Park JS, et al. Effect of bihemispheric anodal transcranial direct current stimulation for dysphagia in chronic stroke patients: a randomized clinical trial. J Rehabil Med. 2017;49(1):30–5.
Cheng IKY, Chan KMK, Wong CS, et al. Neuronavigated high-frequency repetitive transcranial magnetic stimulation for chronic post-stroke dysphagia: a randomized controlled study. J Rehabil Med. 2017;49(6):475–81.
Du J, Yang F, Liu L, et al. Repetitive transcranial magnetic stimulation for rehabilitation of poststroke dysphagia: a randomized, double-blind clinical trial. Clin Neurophysiol. 2016;127(3):1907–13.
Khedr EM, Abo-Elfetoh N. Therapeutic role of rTMS on recovery of dysphagia in patients with lateral medullary syndrome and brainstem infarction. J Neurol Neurosurg Psychiatry. 2010;81(5):495–9.
Khedr EM, Abo-Elfetoh N, Rothwell JC. Treatment of post-stroke dysphagia with repetitive transcranial magnetic stimulation. Acta Neurol Scand. 2009;119(3):155–61.
Kumar S, Wagner CW, Frayne C, et al. Noninvasive brain stimulation may improve stroke-related dysphagia: a pilot study. Stroke. 2011;42(4):1035–40.
Lim KB, Lee HJ, Yoo J, Kwon YG. Effect of low-frequency rTMS and NMES on subacute unilateral hemispheric stroke with dysphagia. Ann Rehabil Med. 2014;38(5):592–602.
Park E, Kim MS, Chang WH, et al. Effects of bilateral repetitive transcranial magnetic stimulation on post-stroke dysphagia. Brain Stimul. 2016;10(1):75–82.
Park JW, Oh JC, Lee JW, Yeo JS, Ryu KH. The effect of 5Hz high-frequency rTMS over contralesional pharyngeal motor cortex in post-stroke oropharyngeal dysphagia: a randomized controlled study. Neurogastroenterol Motil. 2013;25(4):324-330+e250.
Pingue V, Priori A, Malovini A, Pistarini C. Dual transcranial direct current stimulation for poststroke dysphagia: a randomized controlled trial. Neurorehabil Neural Repair. 2018;32(6–7):635–44.
Sawan SAE, Reda AM, Kamel AH, Ali MAM. Transcranial direct current stimulation (tDCS): its effect on improving dysphagia in stroke patients. Egypt J Neurol Psychiatr Neurosurg. 2020. https://doi.org/10.1186/s41983-020-00246-4.
Shigematsu T, Fujishima I, Ohno K. Transcranial direct current stimulation improves swallowing function in stroke patients. Neurorehabil Neural Repair. 2012;27(4):363–9.
Suntrup-Krueger S, Ringmaier C, Muhle P, et al. Randomized trial of transcranial direct current stimulation for poststroke dysphagia. Ann Neurol. 2018;83(2):328–40.
Tarameshlu M, Ansari NN, Ghelichi L, Jalaei S. The effect of repetitive transcranial magnetic stimulation combined with traditional dysphagia therapy on poststroke dysphagia: a pilot double-blinded randomized-controlled trial. Int J Rehabil Res. 2018;42(2):133–8.
Ünlüer N, Temuçin Ç, Demir N, Serel Arslan S, Karaduman AA. Effects of low-frequency repetitive transcranial magnetic stimulation on swallowing function and quality of life of post-stroke patients. Dysphagia. 2019;34(3):360–71.
Yang EJ, Baek SR, Shin J, et al. Effects of transcranial direct current stimulation (tDCS) on post-stroke dysphagia. Restor Neurol Neurosci. 2012;30(4):303–11.
Fewtrell MS, Kennedy K, Singhal A, et al. How much loss to follow-up is acceptable in long-term randomised trials and prospective studies? Arch Dis Child. 2008;93(6):458–61.
Schünemann H, Brożek J, Guyatt G, Oxman A. GRADE handbook for grading quality of evidence and strength of recommendations. The GRADE Working Group Web site. https://www.guidelinedevelopment.org. Published 2013. Accessed 3 Jan 2021.
Sandrini M, Cohen LG. Chapter 40—Noninvasive brain stimulation in neurorehabilitation. In: Lozano AM, Hallett M, editors. Handbook of clinical neurology, vol. 116. Amsterdam: Elsevier; 2013. p. 499–524.
Turner RM, Bird SM, Higgins JPT. The impact of study size on meta-analyses: examination of underpowered studies in cochrane reviews. PLoS ONE. 2013;8(3):e59202.
Aziz Q, Rothwell JC, Hamdy S, Barlow J, Thompson DG. The topographic representation of esophageal motor function on the human cerebral cortex. Gastroenterology. 1996;111(4):855–62.
Shaheen H, Aziz Q, Rothwell JC, et al. Recovery of swallowing after dysphagic stroke relates to functional reorganization in the intact motor cortex. Gastroenterology. 1998;115(5):1104–12.
Hamdy S, Aziz Q, Rothwell JC, et al. Recovery of swallowing after dysphagic stroke relates to functional reorganization in the intact motor cortex. Gastroenterology. 1998;115(5):1104–12.
Wagner T, Valero-Cabre A, Pascual-Leone A. Noninvasive human brain stimulation. Annu Rev Biomed Eng. 2007;9(1):527–65.
Madhavan A. Preclinical dysphagia in community dwelling older adults: what should we look for? Am J Speech Lang Pathol. 2021;30(2):833–43.
Wirth R, Dziewas R, Beck AM, et al. Oropharyngeal dysphagia in older persons—from pathophysiology to adequate intervention: a review and summary of an international expert meeting. Clin Interv Aging. 2016;11:189–208.
Viera AJ, Bangdiwala SI. Eliminating bias in randomized controlled trials: importance of allocation concealment and masking. Fam Med. 2007;39(2):132–7.
Burkhead LM, Sapienza CM, Rosenbek JC. Strength-training exercise in dysphagia rehabilitation: principles, procedures, and directions for future research. Dysphagia. 2007;22(3):251–65.
Acknowledgements
We would like to acknowledge all the study author in this review for contributing their knowledge.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not- for-profit sectors.
Author information
Authors and Affiliations
Contributions
SWT, YL, and STL conceived and guided the study; SWT and AW carried out the literature searches; SWT and AW extracted the data; SWT and AW assessed the study quality; SWT and LJC performed the statistical analysis; SWT, YL, LJC, and STL wrote the manuscript; LJC formatted the manuscript and ensure proper data management; SWT, AW, LJC, SHW, YL, and STL revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethical Approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Tan, S.W., Wu, A., Cheng, L.J. et al. The Effectiveness of Transcranial Stimulation in Improving Swallowing Outcomes in Adults with Poststroke Dysphagia: A Systematic Review and Meta-analysis. Dysphagia 37, 1796–1813 (2022). https://doi.org/10.1007/s00455-022-10424-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00455-022-10424-6