Abstract
Purpose
We examined how migration background is associated with awareness and usage of psycho-oncology services.
Methods
Oncologists in community-based practices and outpatient clinics asked their patients and their relatives to complete a questionnaire. Migrants were purposely over-sampled. The questionnaire was provided in Arabic, English, Farsi, French, German, Hindi, Kurdish, Pashto, Russian, Somali, Turkish, Urdu, and Vietnamese.
Results
From 9 collaborators, 177 participants were enrolled (130 with and 47 without migration background). The existence of outpatient cancer counselling centres was known to 38% of the participants without and 32% with migration background, self-help groups to 32 vs. 12%, and psychotherapy to 43 vs. 25%. Respondents from the Near and Middle East were less likely to know about psychotherapy (odds ratio (OR) 0.1, p = 0.01); those from the Commonwealth of the Independent States or former Yugoslavia were less often informed about self-help groups (OR 0.1, p = 0.06). Migrants retrieved information less frequently from the internet than non-migrants (10 vs. 25%). At least one service had been used by 27% of migrants and 42% of non-migrants (OR 0.5, p = 0.06). After adjusting for gender, age, education, and patient-relative status, there was no evidence for an association between migration background and service use.
Conclusions
Migrants should be better informed about psychotherapy and self-help groups, in particular the ones coming from the Near or Middle East and the Commonwealth of the Independent States or former Yugoslavia.
The under-use of psychosocial services can largely be explained by confounding factors. Therefore, these factors must always be taken into account when analysing the use of psychosocial services in the aforementioned populations.
Similar content being viewed by others
Background
It is well known that people who have migrated to Western European countries use various types of health care—such as prevention, early detection, visits to general practitioners, rehabilitation, or community mental health care—less frequently than the autochthonous population, despite them having the same frequency and severity of diseases (Ahmad et al. 2021; Klein et al. 2018; Larchanche 2012; Wiessner et al. 2020; Zeeb et al. 2004). There are several reasons and mechanisms responsible for this under-use, for example being unaware of the existence of certain services (Larchanche 2012), language barriers (Fang and Baker 2013; Hyatt et al. 2018), not feeling entitled to use the services (Brenman 2021; Larchanche 2012), fear (Fang and Baker 2013), shame (Coleman-Brueckheimer et al. 2009; Fang and Baker 2013), a façading behaviour (Pergert 2017), misconceptions about treatment effects (James et al. 2011; Lourens 2013; Williams et al. 2019), or structural barriers such as financial problems and a lack of insurance (Fang and Baker 2013; Riccetti et al. 2022a, b). Often, it will be a mixture of several reasons.
It is not easy to pin down the “core causes” because migrants are not a homogeneous group of people. They have various cultural and personal backgrounds, different reasons for migration, and are in different phases of the migration process. The term “migrant” is in this respect misleading in its simplicity. Migration research faces the challenge of covering a breadth of aspects of migration—which is often done in large studies where all migrants are treated as one category (Zeeb et al. 2004; Zeissig et al. 2015)—and analysing the complexity of the phenomenon in-depth, often realised by including only certain groups, e.g. only individuals with a Russian or Turkish background, into the study (Cilenti et al. 2021; Erim et al. 2011; Graham et al. 2013; Morawa and Erim 2016; Ronellenfitsch et al. 2009). The first approach may deliver results that are too broad to effectively develop concrete suggestions for improvement of care, while the latter one might result in suggestions only relevant to certain groups of people. It was therefore our aim to find a balance between breadth and depth in our study investigating the use of psycho-oncological care by patients with a migrant background.
In Europe, only a few studies have investigated the care needs and treatment receipt of migrants in psycho-oncology (Ng et al. 2013; Weis et al. 2021; Zeissig et al. 2015). Most research on this topic stems from the United States or Canada (Riccetti et al. 2021) showing, for example, that African American and Hispanic women with cancer often report information needs regarding financial problems and not being able to provide for their families (Maguire et al. 2015), whereas this issue is less often mentioned by Chinese patients (Lim et al. 2017).
However, translating these findings to the European context is not directly possible because of the large differences in the health care systems.
Investigating the topic of psycho-oncology specifically seemed necessary because in some countries, mental health problems are severely stigmatised, resulting in the concealment of such problems and denial of the need to seek professional help (Saxena et al. 2007). Moreover, culture and religion can be associated with what people consider to be the cause of mental health problems (Lim et al. 2015; Sheikh and Furnham 2000), which in turn also influences the likelihood of using mental health care. For these reasons, it is possible that cancer patients and relatives with a migration background who experience mental health problems suffer from triple stigmatisation: being a member of an ethnic minority, having cancer, and suffering mentally. This may result in reduced use of psychosocial care (Merbach et al. 2006).
We, therefore, aimed to explore the awareness and the use of psycho-oncological services as well as specific treatment needs of immigrants from certain predefined regions of origin versus non-migrants in Germany.
More specifically, our research questions were:
-
1.
What is the proportion of cancer patients and their relatives with and without a migration background who are informed about psychosocial services?
-
a.
Where and when were they informed? What are their preferences in this regard?
-
b.
In people with a migration background: In what language did they receive the information? What are their preferences in this regard? Do they know of such services from their country of origin?
-
a.
-
2.
What is the proportion of cancer patients and their relatives with and without a migration background who used psychosocial services?
-
3.
Is awareness or usage of psycho-social services associated with characteristics of the migration background (i.e., region of origin, nationality, reason for migration, time since migration) and local language proficiency? Does this differ between patients and relatives?
Methods
Study design and data collection
This was a multi-centre, cross-sectional study in Germany. Cancer patients and their relatives were enrolled via a nationwide network of community-based practices specialising in medical oncology (Scientific Institute of Office-based Haematologists and Oncologists [“Wissenschaftliches Institut der Niedergelassenen Hämatologen und Onkologen”], WINHO) and outpatient cancer clinics at university hospitals. The doctors or nurses informed the patients and their relatives about the study and asked them to participate. They were reimbursed for this work.
The patients and relatives received an information leaflet and a questionnaire which was available in 13 different languages: Arabic, English, Farsi, French, German, Hindi, Kurdish, Pashto, Russian, Somali, Turkish, Urdu, and Vietnamese. These languages had been chosen because they are spoken by the majority of cancer patients with a non-German mother tongue (authors' calculations based on data from the WINHO patient survey 2015, unpublished) or by major migrant groups in Germany (Bundesamt 2016). If the questionnaire had not been translated into the native language of the participant, it was handed out in another language, mostly English, French, or German, depending on their preference.
The doctors were asked to approach individuals from different regions according to a predefined sampling matrix (see “Definition of the region of origin” section). We aimed at including a certain number of individuals per region. Unfortunately, this became difficult because of the COVID-19 pandemic, which began shortly after our study started (Hempler et al. 2021a, b, c), leading to more workload for the medical staff and more difficult logistics in meeting patients and relatives for interviews (which were necessary for the development of the questionnaire). We also included a sample of patients and relatives without a migration background for comparison purposes.
Further inclusion criteria were: a verified cancer diagnosis (all phases of disease) and a minimum age of 18 years. The only exclusion criterion was when the patient/relative was born outside Germany but both parents were of German nationality at that time.
The participants put the completed questionnaires anonymously into boxes that were provided by the collaborators. Because of that procedure, written consent was not necessary. It was not documented who participated and who did not, because it was assumed that ensuring the anonymity of the survey would increase the willingness to participate in the survey, especially in hard-to-reach populations (Enticott et al. 2017). Hence, the clinical characteristics of the participants are all self-reported.
The study protocol and conduct were supported by a patient representative with a migration background.
Instrument
The questionnaire for this study was developed based on qualitative interviews with cancer patients who themselves or their parents had migrated to Germany and these patients’ relatives (Hempler et al. 2021a, b, c) and on qualitative interviews with cancer specialists (Hempler et al. 2021a, b, c). We asked about the following:
Characteristics of the migration background: country of birth, country of mother’s birth, country of father’s birth, year of migration, reason(s) for migration (e.g., refuge/asylum seeker/international protection, work, marriage).
German language proficiency: This was ascertained by asking whether the doctor-patient consultations need to be translated.
Awareness of services: We asked whether they were informed about cancer counselling centres, self-help groups, psychotherapy, and other types of support (with the possibility to write down what other types of support), and where they had been informed, and at what time during the course of treatment. Individuals who were born outside of Germany were asked whether they knew of such services from their country of origin. They were also asked in what language they had received the information and whether they had wished to receive it in another language.
Use of psychosocial services: Respondents indicated whether they had used cancer counselling centres, self-help groups, psychotherapy, and/or other types of support.
Emotional and social functioning were ascertained using the respective scales of the European Organization for Research and Treatment of Cancer Core Instrument (EORTC QLQ-C30) (Aaronson et al. 1993). Items were summarised and transformed to scores between 0 and 100. Higher scores indicate better functioning. Patients were grouped into “high distress” if their functioning was worse than the threshold of clinical importance (Giesinger et al. 2020).
Data analysis
Definition of a migration background
Individuals were defined as “having a migration background” if one or more of the following criteria were fulfilled:
-
(a)
they had been born outside of Germany
-
(b)
one or both of their parents were born outside of Germany
-
(c)
their nationality was not German or both German and non-German (dual citizen)
-
(d)
their mother tongue was not German
Further, we ascertained the generation of the migrants (first, second, or third generation).
Definition of the region of origin
The pre-defined regions of origin were: Near and Middle East (including North Africa); Sub-Saharan Africa; Southeast Asia and East Asia; Commonwealth of Independent States (including Ukraine and Georgia), the Baltic States, and former Yugoslavia (including Albania); European Union (except former Yugoslavia and the Baltic States) or North America (USA, Canada); all other countries. Individuals were coded as “coming from this region” if they or their parents were born in a country in this particular region. If patient and parents came from different regions, the region of the parents was used to define the region of origin. If mother and father came from different regions, the region of the mother was used.
If the country of birth was unknown, the language of the questionnaire was used as a proxy to define the region if it was sufficiently clear. For example, if the questionnaire was in Russian, the region was coded as “Commonwealth of Independent States”. If, however, the questionnaire was in English and no other information about the country of birth or mother tongue was available, the region was left as “unknown”.
Statistical approach
Group differences between participants with and without a migration background were explored with chi-square and t-tests. Then, the association of characteristics of the migration background (i.e., region of origin, nationality, reason for migration, time since migration) and German language proficiency with awareness and use of psychosocial services were investigated using binary logistic regression analyses while adjusting for gender, age, and education. Emotional and social functioning were not adjusted for because they were considered to be on the causal pathway.
We report the odds ratios (OR) and use 95% confidence intervals to quantify statistical uncertainty.
Potential effect modification by patient-relative status was explored using Mantel–Haenszel tests and likelihood-ratio tests.
Statistical analyses were performed using STATA 15 (StataCorp 2017, College Station, TX: StataCorp LP).
Results
Sample
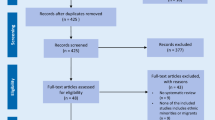
In total, 184 completed questionnaires were collected during the study period (June to September 2021). In 7 of them, the migration status could not be clearly classified, leaving 177 for the analysis. Among them, 130 had a migration background and 47 did not (for details see Table 1). The regions of origin were primarily the Near and the Middle East and the Commonwealth of Independent States. No patient from Sub-Saharan Africa was enrolled.
Participants with and without a migration background differed in many demographic aspects (Table 1), which is why these variables were taken into account when comparing the groups regarding awareness and use of psychosocial services.
Among the participants with a migration background, 117 (90%) were first-generation migrants (Table 1).
Emotional and social functioning
Among participants from all regions, emotional and social functioning were below the means of the general population (Supplemental Material, eFigure 1). Participants with a migration background had an average score of 60.3 in emotional functioning, while non-migrants had a mean score of 53.2 (p = 0.18). The percentage of self-reported increased emotional distress was 57% in migrants and 72% in non-migrants (p = 0.07).
Social functioning was on average better in migrants than in non-migrants (58.5 versus 41.5, p = 0.005). The proportion of self-reported increased social distress was 47% among migrants and 60% among non-migrants (p = 0.14).
Awareness of psychosocial services
Among the participants, 38% of non-migrants and 32% of migrants reported being aware of cancer counselling centres (p = 0.04), 32 and 12% of self-help groups (p = 0.002), 43 and 25% of psychotherapy (p = 0.03), and 13 and 8% of other support (p = 0.21). Other support options mentioned included: consultation-liaison services, social services at the hospital, general practitioners, and staff of health care insurance. The number of services known ranged from 0 to 4, with an average of 1.3 (in those without migration: 1.5, in those with migration: 1.2, p = 0.04). At least one of the services was known to 87% of the respondents without and 86% with a migration background (OR 0.89, p = 0.85).
Of the respondents who were born outside of Germany (n = 107), 7 (7%) said they knew about such services in their country of origin, 85 (79%) said there were none, and 15 (14%) did not reply to this question. Notably, none of the patients/relatives from (South-) East Asia and from other non-EU/non-North American countries knew about such services in their country of origin, while 10% (n = 4) of the ones from the Commonwealth of Independent States did.
Sources of information
The majority of the respondents received information about services in the hospital and/or community-based practices (Table 2). The internet (10 vs. 25%, p = 0.02) and flyers (6 vs. 15%, p = 0.08) were less often mentioned as an information source by patients and relatives with a migration background. They also generally had fewer other sources of information compared to non-migrants (1 vs. 10%, p = 0.01).
Preferred and actual time-point of information
The most often preferred time-point for information about psychosocial services was at the time of diagnosis and at several time points during the disease trajectory (Fig. 1). They most frequently received this information during acute treatment.
There were few differences between respondents from different regions regarding preferences. For example, people from the Near and Middle East as well as those from other countries outside of the EU and North America more often expressed the wish to receive information already at diagnosis, whereas individuals from East and Southeast Asia less often did so (Fig. 1).
Language of information material
Among the migrants (n = 130), the majority (64%) had received information about psychosocial services in German only, 10% in another language, 8% both in German and another language, and 18% did not answer this question.
The other languages were Turkish (n = 9), Russian (n = 4), English (n = 2) as well as Arabic, Ukrainian, Urdu, Serbian/Bosnian/Croatian (each with n = 1), or not further specified (n = 5).
A total of 17 (13%) said they had wished they had received information in another language, 68 (52%) were satisfied with the language they had received, and 45 (35%) did not answer this question. The most frequently mentioned language in which patients hat wished to receive information was Russian (n = 11), followed by Dutch (n = 2), Polish, Bulgarian, Lithuanian, and Indonesian (each with n = 1).
Use of psychosocial services
The most frequently used psychosocial service both in migrants and non-migrants was psychotherapy (12 and 28%, respectively, p = 0.01). Outpatient cancer counselling centres had been visited by 8% of migrants and 4% of non-migrants (p = 0.42), self-help groups by 1% of migrants and 9% of non-migrants (p = 0.01), other support by 5% of migrants and 15% of non-migrants (p = 0.04). The sum of services used ranged from none to 4, with an average of 0.3 in migrants and 0.6 in non-migrants (p = 0.01).
At least one service was used by 27% of migrants and 42% of non-migrants (odds ratio 0.5, p = 0.06).
Association of migration background characteristics with awareness and use of psychosocial services
We found no effect modifications by patient-relative status; hence, we included it as a potential confounder in the models. Reasons for migration and time since migration had too many missing values and were therefore excluded. As self-help groups were only used by 5 respondents, we used the combined use of psychosocial services as the outcome variable (either cancer counselling service or psychotherapy or self-help group or other service or a combination of these).
When adjusting for age, gender, and education, there were only a few associations of migration background characteristics with awareness and usage of psychosocial services (Table 3): respondents from the European Union or North America had 11 times the odds of being informed about cancer counselling centres; those from the Near and Middle East were less likely to be informed about psychotherapy; those from the Commonwealth of the Independent States, the Baltic States or former Yugoslavia were less often informed about self-help groups.
Women had 2.4 times the chance of being informed about cancer counselling centres (p = 0.08), whereas no differences in awareness about other services were present. Being informed about psychotherapy was negatively correlated with the age of the responders (OR 0.9, p < 0.01). Compared to responders with compulsory education only, the ones with post-compulsory training (OR 0.2, p = 0.01) and a university degree (OR 0.2, p = 0.02) were less likely to be aware of psychotherapy.
Use of psychosocial services was less likely among people from the Near and Middle East and more likely in those with German nationality, though the confidence intervals were large in both cases (Table 3). Women were more likely to use psychosocial services compared to men (OR 2.7, p = 0.07), and with increasing age, the odds of using services decreased (OR 0.9, p = 0.05). There was no evidence for an independent effect of education on psychosocial services use.
Discussion
With this study, we examined how cancer patients (and their relatives) with a migration background are informed about psychosocial services and how often they make use of it compared to non-migrants.
A recent study from the UK (Ahmad et al. 2021) found that the prevalence of common mental disorders did not differ between ethnic groups if socioeconomic and demographic characteristics were taken into account. Treatment receipt, however, did. Asian, non-British white, and especially black people received treatment less often (i.e., antidepressant medication, counselling or therapy, talking to a general practitioner for mental, nervous or emotional complaint, visiting a community mental health specialist in the past 12 months). Even more concerning is the finding that these inequalities increased between 2007 and 2014 despite the “Improving Access to Psychological Therapies (IAPT)” programme that was launched there in 2008 to decrease inequalities in mental health care.
We also found considerable differences regarding awareness and usage of psycho-oncological services. However, some of them were likely due to confounding factors. For example, the proportion of men was higher in migrants than in non-migrants. It is well known that men use psychosocial services less often than women (Bayer et al. 2020; Doherty and Kartalova-O'doherty 2010; Oliffe and Phillips 2008; Plakun 2021) , and this effect was present in our study, too. Hence, part of the differences between migrants and non-migrants in the use of psychosocial services can be explained by gender. This again underlines the notion that it is not enough to provide special services to “migrants in general”, but we must identify the vulnerable groups among them; we must ask what groups of patients and relatives need what type of support.
Still, even when taking gender, age, education, and relative status into account, in our study, people coming from the Near and Middle East were clearly less likely to be informed about psychotherapy and hence less able to use these services, which is in line with the results of Ahmad et al. (2021). As this result was also adjusted for German language proficiency, it is unlikely that this under-information is solely due to communication barriers. Possible reasons for this result could be related to lacking cultural sensibility on the side of health care providers or underlying cultural/religious beliefs not captured in this study on the side of patients.
Another relevant point was that in the group of migrants, the proportion of relatives was higher than in the non-migrants, and relatives were also less frequently informed about the various services. This is in line with other research showing that relatives are less often aware that they are entitled to use psycho-oncological services (Billaudelle et al. 2022; Meyer et al. 2015; Singer et al. 2022).
The limited power of our study is another explanation for this “loss” of association when adjusting for other variables and looking in more detail at which factors of the migration background might play a role. Our aim had been to include about 50 patients per region, but this became difficult due to the COVID-19 pandemic. For example, relatives were not allowed to accompany patients anymore, making it more difficult to hand out the questionnaires to them. In addition, the doctors in the practices were barely able to perform their usual daily workload and could not approach as many patients as they usually would (Hempler et al. 2021a, b, c). Colleagues from two outpatient clinics offered to help and indeed enrolled about a third of all participants. However, the study period could not be extended due to the end of funding and so some cells in the sampling matrix remained empty (for people from Sub-Saharan Africa) or filled with fewer than 50 individuals. This is a clear limitation of our study.
A positive feature is that we were able to enrol quite a few people from the Near and Middle East and the Commonwealth of Independent States. We could provide the questionnaire in several languages which is considered to be good practice to increase participation in studies with migrants (Reiss et al. 2013). By this, we were able to reduce the selection bias due to missing language proficiency. Our results also underline that patients and relatives often prefer to receive information in their native language. This is not only necessary for the “transfer of knowledge” in people with limited language proficiency it also gives a sense of familiarity in a situation of increased insecurity, which is also important for those who perfectly speak the language of the health care professional (Hempler et al. 2021a, b, c). Another aspect can be related to being able to speak in the native language: In many cultures, the women are responsible for taking care of the family’s health. Hence, using the mother tongue can be related to being cared for and feeling comforted (Arghavanian et al. 2020; Graham et al. 1985; Mesler et al. 2022; Zhang et al. 2019).
Research found that to ease access for migrants, health care not only needs translation of consultations or information material but also culturally sensitive approaches and openness to the “otherness” of the patients (Merbach 2019; Röhnsch and Flick 2015; Schrank et al. 2017). In a multi-centre randomised controlled trial, Hölzel et al. showed that information material was evaluated to be more useful by patients of Russian, Turkish, Polish, and Italian origin who had depression or chronic low back pain if it was culturally sensitive in contrast to a simple translation (Holzel et al. 2016). This effect was larger in patients with low levels of acculturation.
Hence, translating information material about psychosocial services and adapting it culturally for the various migrant groups seems very valuable. However, our study also showed the challenges of such an endeavour. Instead of one set of questionnaires, we sent 13 sets to our collaborators—one in each language. This needs to be stored somewhere in the clinic or practice. A possible solution would be to provide this material online. However, we found that the migrants in our study used the internet less often than non-migrants; it would therefore be advisable that the doctor or nurse prints the information out and hands it to the patients and relatives.
Another relevant aspect is the doctor–patient-relationship. Our interviews and survey of doctors indicate that they experience issues with the doctor–patient-relationship more often with patients from the Near or Middle East, Sub-Saharan Africa, and the Commonwealth of Independent States (Hempler et al. 2021a, b, c; Hermes-Moll et al. 2022; Riccetti et al. 2022a, b). The doctors themselves often related these problems in the relationship to language barriers. However, it is also possible that other factors, more or less unconsciously, influence the way they communicate with patients coming from countries or cultures they feel unfamiliar with. For example, they may expect that patients from specific countries or of a certain gender are not interested in taking up psychotherapy due to stereotypes and thus do not provide such information. As a consequence, some patients may be left less well informed about the services they could use. In combination with the patient’s own feelings of not being entitled to use services (Brenman 2021; Larchanche 2012), fears (Fang et al. 2013), or feelings of shame (Coleman-Brueckheimer et al. 2009; Fang et al. 2013), this can lead to psycho-oncological under-care for these patients. To counter such processes, it might be advisable to set up a standard procedure where all patients and relatives, independent of their ethnic or religious background, are asked about their need for support and are informed about available services—not only that they exist but also what they can offer and how to access them (Hermes-Moll et al. 2022).
An important limitation of our study is that respondents from Southeast and East Asia and from Sub-Saharan Africa could not be enrolled as often as we had hoped, resulting in small numbers and making it more difficult to compare awareness and usage of psychosocial services in these groups with other groups.
Another problem was that not all participants completed the crucial questions about migration background due to a mistake (logical inconsistency) in the questionnaire. As the data collection was anonymised, they could not be contacted and health care staff could not complete this information. This further reduced the sample size (7 questionnaires had to be excluded).
Clinical implications
Cancer patients and their relatives who have a migration background are not as well informed about psychosocial services as non-migrants. Only 12% of them use psychotherapy compared to 28% of patients and relatives without a migration background. These differences can largely be explained by differences in age, gender, and education, which are in turn related to the awareness and use of psychosocial services. To support cancer patients and their relatives, clinicians should provide information about psycho-oncological services at the time of diagnosis as well as during the course of the treatment, optimally in the patients’ native language and culturally adapted. Moreover, information should be provided in a standardized way, so that everybody is equally informed, independent of their age, gender, education, religion, culture, languages spoken, etc. This is already a requirement for hospitals to be certified by the German Cancer Society (Herschbach and Mandel 2011; Kowalski et al. 2016) and is a recommendation for the outpatient sector, too (Hermes-Moll et al. 2022).
Psychosocial problems and care needs should also be ascertained using instruments in the language the patient prefers. The instruments could be stored electronically in multiple languages and then be printed out when needed.
Further, more and better training of medical staff in culturally sensitive counselling is needed. This should already start during university, but must be continued over the entire span of their career.
How the services can be provided in their mother tongue remains an open question. It requires further research and probably the development of new, innovative programs.
The establishment of culturally specific patient support groups in corresponding languages might also be helpful.
Conclusions
Cancer patients and their relatives with a migration background should receive more information about psychotherapy and self-help groups in particular. This is especially true for people coming from the Near or Middle East regarding information about psychotherapy and for people from the Commonwealth of the Independent States or former Yugoslavia regarding information about self-help groups.
Migrants also use psychosocial services less often than non-migrants. However, this difference can largely be explained by confounding factors such as gender, age, education, and being a relative versus a patient. These factors must therefore always be taken into account when analysing service use in migrant populations.
Data availability
The data that support the findings of this study are available on reasonable request from the corresponding author. The data are not publicly available due to privacy restrictions.
References
Aaronson N, Ahmedzai S, Bergmann B, Bullinger M, Cull A, Duez NJ, Filiberti A, Flechtner H, De Haes JCJM, Kaasa S, Klee M, Osoba D, Razavi D, Rofe PB, Schraub S, Sneeuw K, Sullivan M, Takeda F, Life FTESGOQO (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: A Quality-of-Life Instrument for Use in International Clinical Trials in Oncology. J Nat Cancer Institute 85:365–376
Ahmad G, Mcmanus S, Cooper C, Hatch S, Das-Munshi J (2021) Prevalence of common mental disorders and treatment receipt for people from ethnic minority backgrounds in England: repeated cross-sectional surveys of the general population in 2007 and 2014. Br J Psychiatry. https://doi.org/10.1192/bjp.2021.179
Arghavanian FE, Roudsari RL, Heydari A, Bahmani MND (2020) Pregnant women’s experiences of social roles: An ethnophenomenological study. Iran J Nurs Midwifery Res 25:31–39
Bayer O, Billaudelle F, Alt J, Heß G, Specht M, Höfinghoff B, Riedel P, Wickert M, Hechtner M, Singer S (2020) What prevents men from visiting outpatient cancer counseling centers. A Qualitative Study. Der Onkologe 26:1047–1055
Billaudelle F, Bayer O, Hechtner M, Taylor K, Lang J, Alt J, Fried M, Singer S (2022) “That was a tip from my physician”- Gender-specific pathways of patients and relatives to outpatient psychosocial cancer counselling centres - a qualitative study. Psycho-Oncology 31(6):1022–1030
Brenman NF (2021) Placing precarity: access and belonging in the shifting landscape of UK mental health care. Cult Med Psychiatry 45:22–41
Bundesamt S (2016) Bevölkerung und Erwerbstätigkeit - Bevölkerung mit Migrationshintergrund 2016. Statistisches Bundesamt, Wiesbaden
Cilenti K, Rask S, Elovainio M, Lilja E, Kuusio H, Koskinen S, Koponen P, Castaneda AE (2021) Use of health services and unmet need among Adults of Russian, Somali, and Kurdish Origin in Finland. Int J Environ Res Public Health 18:21
Coleman-Brueckheimer K, Spitzer J, Koffman J (2009) Involvement of Rabbinic and communal authorities in decision-making by haredi Jews in the UK with breast cancer: an interpretative phenomenological analysis. Soc Sci Med 68:323–333
Doherty DT, Kartalova-O’doherty Y (2010) Gender and self-reported mental health problems: Predictors of help seeking from a general practitioner. Br J Health Psychol 15:213–228
Enticott JC, Shawyer F, Vasi S, Buck K, Cheng IH, Russell G, Kakuma R, Minas H, Meadows G (2017) A systematic review of studies with a representative sample of refugees and asylum seekers living in the community for participation in mental health research. BMC Med Res Methodol 17:37
Erim Y, Morawa E, Ozdemir DF, Senf W (2011) Prevalence, comorbidity and severity of psychosomatic disorders in outpatients with Turkish Migration Background. Psychother Psychosom Med Psychol 61:472–480
Fang DM, Baker DL (2013) Barriers and facilitators of cervical cancer screening among women of Hmong origin. J Health Care Poor Underserved 24:540–555
Giesinger JM, Loth FLC, Aaronson NK, Arraras JI, Caocci G, Efficace F, Groenvold M, Van Leeuwen M, Petersen MA, Ramage J, Tomaszewski KA, Young T, Holzner B (2020) Thresholds for clinical importance were established to improve interpretation of the EORTC QLQ-C30 in clinical practice and research. J Clin Epidemiol 118:1–8
Graham H (1985) Providers, negotiators, and mediators: women as the hidden carers. In: Lewin E, Oleson V (eds) Women, health, and healing. Tavistock, New York, pp 25–52
Graham N, Gwyther L, Tiso T, Harding R (2013) Traditional healers’ views of the required processes for a "Good Death’’ Among Xhosa patients pre- and post-death. J Pain Symptom Manage 46:386–394
Hempler I, Riccetti N, Heidt V, Singer S, Hermes-Moll K (2021a) “We knew it was going to be tough, but we didn’t expect this!” Experiences with the inclusion of cancer patients with a migrant background and their relatives in the field of psycho-oncology. Z Evid Fortbild Qual Gesundhwes 166:55–59
Hempler I, Riccetti N, Hermes-Moll K, Heidt V, Singer S (2021b) Psycho-oncological care for people with a migration background and their relatives - results of semi-structured interviews with physicians. Psychother Psychosom Med Psychol 71:335–342
Hempler I, Riccetti N, Kalie L, Heidt V, Singer S, Hermes-Moll K (2021c) “It was too much, too soon, too foreign” Barriers and needs in the psycho-oncological care of people with a migration background and their relatives. Onkologe 12:1233–1240
Hermes-Moll K, Hempler I, Riccetti N, Heymanns J, Heller JK, Schwaner I, Mosthaf F, Fried M, Fuchs M, Mönnighoff U, Heidt V, Singer S (2022) Krebserkrankte mit Migrationshintergrund - Empfehlungen zur psychosozialen und psychoonkologischen Versorgung. InFo Hämatol Onkol 25:72–80
Herschbach P, Mandel T (2011) Psychoonkologische Versorgung Im Nationalen Krebsplan. Onkologe 17:1107–1114
Holzel LP, Ries Z, Kriston L, Dirmaier J, Zill JM, Rummel-Kluge C, Niebling W, Bermejo I, Harter M (2016) Effects of culture-sensitive adaptation of patient information material on usefulness in migrants: a multicentre, blinded randomised controlled trial. BMJ Open 6:11
Hyatt A, Lipson-Smith R, Gough K, Butow P, Jefford M, Hack TF, Hale S, Zucchi E, White S, Ozolins U, Schofield P (2018) Culturally and linguistically diverse oncology patients’ perspectives of consultation audio-recordings and question prompt lists. Psychooncology 27:2180–2188
James A, Daley CM, Greiner KA (2011) “Cutting” on cancer: Attitudes about cancer spread and surgery among primary care patients in the USA. Soc Sci Med 73:1669–1673
Klein J, Von Dem Knesebeck O (2018) Inequalities in health care utilization among migrants and non-migrants in Germany: a systematic review. Int J Equity Health 17:10
Kowalski C, Ferencz J, Singer S, Weis I, Wesselmann S (2016) Frequency of psycho-oncologic and social service counseling in cancer centers relative to center site and hospital characteristics: Findings from 879 center sites in Germany, Austria, Switzerland, and Italy. Cancer 122:3538–3545
Larchanche S (2012) Intangible obstacles: Health implications of stigmatization, structural violence, and fear among undocumented immigrants in France. Soc Sci Med 74:858–863
Lim A, Hoek HW, Blom JD (2015) The attribution of psychotic symptoms to jinn in Islamic patients. Transcult Psychiatry 52:18–32
Lim BT, Butow P, Mills J, Miller A, Goldstein D (2017) Information needs of the Chinese community affected by cancer: a systematic review. Psychooncology 26:1433–1443
Lourens M (2013) An exploration of Xhosa speaking patients’ understanding of cancer treatment and its influence on their treatment experience. J Psychosoc Oncol 31:103–121
Maguire R, Kotronoulas G, Simpson M, Paterson C (2015) A systematic review of the supportive care needs of women living with and beyond cervical cancer. Gynecol Oncol 136:478–490
Merbach M, Wittig U, Braehler E (2006) Migrants’ attitudes to psychosocial consultation. Psychol Health 21:102–102
Merbach M (2019) Sich irritieren lassen: Femdheit und Befremden in der Arbeit mit geflüchteten Menschen. Vandenhoeck & Ruprecht
Mesler RM, Leary RB, Montford WJ (2022) The relationships between masculine gender role discrepancy, discrepancy stress and men’s health-related behavior. Personal Individ Differ 184:111205
Meyer A, Keszte J, Wollbrück D, Dietz A, Oeken J, Vogel H-J, Koscielny S, Breitenstein K, Schock J, Pabst F, Bourkas S, Singer S (2015) Psychological distress and need for psycho-oncological support in spouses of total laryngectomised cancer patients - results from the first 3 years after surgery. Support Care Cancer 23:1331–1339
Morawa E, Erim Y (2016) Traumatic events, posttraumatic stress disorder and utilization of psychotherapy in immigrants of Polish Origin in Germany. Psychother Psychosom Med Psychol 66:369–376
Ng CG, Boks MPM, Smeets HM, Zainal NZ, De Wit NJ (2013) Prescription patterns for psychotropic drugs in cancer patients; a large population study in the Netherlands. Psychooncology 22:762–767
Oliffe JL, Phillips MJ (2008) Men, depression and masculinities: a review and recommendations. J Mens Health 5:194–202
Pergert P (2017) Facading in transcultural interactions: examples from pediatric cancer care in Sweden. Psychooncology 26:1013–1018
Plakun E (2021) Improving access to psychotherapy: implications of wit versus united behavioral health. J Psychiatr Pract 27:199–202
Reiss K, Makarova N, Spallek J, Zeeb H, Razum O (2013) Identification and sampling of people with migration background for epidemiological studies in Germany. Gesundheitswesen 75:E49–E58
Riccetti N, Werner A, Ernst M, Hempler I, Singer S (2021) Migrants and ethnic minorities with cancer: an umbrella review on their information and supportive care needs. Onkologe 27:133–144
Riccetti N, Felberbaum R, Flock F, Kühn T, Leinert E, Schwentner L, Singer S, Taylor K, Wöckel A, Janni W (2022a) Financial difficulties in breast cancer survivors with and without migration background in Germany – results from the prospective multicentre cohort study BRENDA II. Support Care Cancer. https://doi.org/10.1007/s00520-022-07074-7
Riccetti N, Hempler I, Hermes-Moll K, Heidt V, Bayer O, Walawgo T, Merbach M, Singer S (2022b) Linguistic barriers in communication between oncologists and cancer patients with migration background in Germany: an explorative analysis based on the perspective of the oncologists from the mixed-methods study POM. Res Health Serv Regions. https://doi.org/10.1007/s43999-022-00001-7
Röhnsch G, Flick U (2015) Representations of care of migrants from the former Soviet Union with alcohol or drug problems in Germany. Psychiatr Prax 42:370–376
Ronellenfitsch U, Kyobutungi C, Ott JJ, Paltiel A, Razum O, Schwarzbach M, Winkler V, Becher H (2009) Stomach cancer mortality in two large cohorts of migrants from the Former Soviet Union to Israel and Germany: are there implications for prevention? Eur J Gastroenterol Hepatol 21:319–326
Saxena S, Thornicroft G, Knapp M, Whiteford H (2007) Global Mental Health 2 - Resources for mental health: scarcity, inequity, and inefficiency. Lancet 370:878–889
Schrank B, Rumpold T, Amering M, Masel EK, Watzke H, Schur S (2017) Pushing boundaries-culture-sensitive care in oncology and palliative care: a qualitative study. Psychooncology 26:763–769
Sheikh S, Furnham A (2000) A cross-cultural study of mental health beliefs and attitudes towards seeking professional help. Soc Psychiatry Psychiatr Epidemiol 35:326–334
Singer S, Kojima E, Deppisch L, Taylor K, Wickert M, Riedel P, Alt J, Heß G, Hechtner M, Bayer O (2022) What is the best time for psychosocial counselling from the perspective of cancer patients and their relatives? A multi-centre qualitative study. Counsel Psychother Res. https://doi.org/10.1002/capr.12488
Weis J, Dresch C, Bartsch HH, Kurlemann U, Maiwald P, Rademaker AL, Valentini J, Joos S, Heidt V (2021) Barriers in the application process for oncological rehabilitation: a nationwide expert study. Rehabilitation 60:95–101
Wiessner C, Keil T, Krist L, Zeeb H, Dragano N, Schmidt B, Ahrens W, Berger K, Castell S, Fricke J, Fuhrer A, Gastell S, Greiser H, Guo F, Jaeschke L, Jochem C, Jockel KH, Kaaks R, Koch-Gallenkamp L, Krause G, Kuss O, Legath N, Leitzmann M, Lieb W, Meinke-Franze C, Meisinger C, Mikolajczyk R, Obi N, Pischon T, Schipf S, Schmoor C, Schramm S, Schulze MB, Sowarka N, Waniek S, Wigmann C, Willich SN, Becher H (2020) Persons with migration background in the German National Cohort (NAKO)-sociodemographic characteristics and comparisons with the German autochthonous population. Bundesgesundheitsblatt-Gesund 63:279–289
Williams ED, Whitaker KL, Piano M, LaV M (2019) Ethnic differences in barriers to symptomatic presentation in primary care: a survey of women in England. Psychooncology 28:2336–2343
Zeeb H, Baune BT, Vollmer W, Cremer D, Kramer A (2004) Health situation of and health service provided for adult migrants - a survey conducted during school admittance examinations. Gesundheitswesen 66:76–84
Zeissig SR, Singer S, Koch L, Zeeb H, Merbach M, Bertram H, Eberle A, Schmid-Höpfner S, Holleczek B, Waldmann A, Arndt V (2015) Utilisation of psychosocial and informational services in immigrant and non-immigrant German cancer survivors. Psychooncology 24:919–925
Zhang ZD, Zhang L, Zu XQ, Liu TS, Zheng JW (2019) From neighboring behavior to mental health in the community: the role of gender and work-family conflict. Int J Environ Res Public Health 16:2101
Acknowledgements
We are very grateful to the doctors and medical staff who helped to enrol participants: Roswitha Fuchs, Andreas Köhler, Beate Jung (Langen), Martina Haibach (Erlangen), Ralf Meyer (Bremen), Barbara Ruf (Offenburg), Eva Trescher (Karlsruhe), and Alexandra Hesse (Goslar).
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the German Cancer Aid (#70113529).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Susanne Singer received funding from Lilly for reviewing submissions for their Quality-Of-Life-Award, outside of this study. The other authors declare that they have no conflict of interest.
Ethical standards
Ethical approval was obtained from the Ethics Committee of the state of Rhineland-Palatinate, Germany (2019-14424).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Singer, S., Riccetti, N., Hempler, I. et al. Awareness and use of psychosocial care among cancer patients and their relatives—a comparison of people with and without a migration background in Germany. J Cancer Res Clin Oncol 149, 1733–1745 (2023). https://doi.org/10.1007/s00432-022-04091-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00432-022-04091-1