Abstract
The main causes of voice disorders in children with adverse vocal behavior include benign lesions of the vocal folds caused by voice abuse or misuses, such as vocal fold nodules, vocal fold polyps, and laryngitis. Long-term voice disorders can affect the physical and mental health of children. Reviewing the literature of the last two decades on “Vocal Fold Nodules,” “Vocal Fold Polyp,” “Voice disorder,” “Voice Abuse,” “Voice Misuse,” “Pediatrics,” and “Children” with the appropriate Boolean operators.
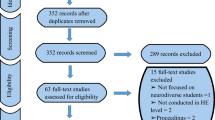
Conclusion: A total of 315 results were returned on an initial PubMed search. All articles from 2000 to 2022 written in English or Chinese were screened. Duplicate articles, those relating to adults only or concerned with the malignant lesion of the vocal cord, were excluded, resulting in 196 articles of interest. Relevant references and books have also been consulted, and we provide a review of the pathogenesis, diagnosis, and treatment of these maladaptive vocal behavioral voice disorders.
What is Known: • Hoarseness is the most common voice symptom in children, and there are various causes of hoarseness in children. However, there is a lack of reviews on voice disorders caused by adverse vocal habits in children. • Voice training is a conservative treatment method for children with voice disorders , and it is important to clarify the factors that influence the effectiveness of voice training for children. | |
What is New: • This review of the personality and family characteristics of children with adverse vocal behavioural voice disorders provides a valuable guide to the clinical planning of subsequent treatment. • This article discusses and summarises some of the factors that may influence the effectiveness of voice training in children and collates some of the scales and questionnaires currently used in children that are important in predicting the effectiveness of voice training. |
Similar content being viewed by others
Data availability
Data availability is not applicable to this article as no new data were created or analyzed in this study.
References
Ma EP, Yu CH (2013) Listeners’ attitudes toward children with voice problems. J Speech Lang Hear Res 5:1409–1415. https://doi.org/10.1044/1092-4388(2013/11-0242)
Gray SD (2000) Cellular physiology of the vocal folds. Otolaryngol Clin North Am 4:679–698. https://doi.org/10.1016/s0030-6665(05)70237-1
Ishii K, Yamashita K, Akita M, Hirose H (2000) Age-related development of the arrangement of connective tissue fibers in the lamina propria of the human vocal fold. Ann Otol Rhinol Laryngol 11:1055–1064. https://doi.org/10.1177/000348940010901112
Swain SK, Nahak B, Sahoo L, Munjal S, Sahu MCJIJoCH (2019) Pediatric dysphonia-a review 1:1–5
Hou LZ, Han DM, Xu W, Zhang L, Ye JY, Wang J (2005) Voice spectrum analysis of hoarseness and benign hyperplastic vocal cord disease in children. Otolaryng Head Neck 12:771–774
Baker BM, Blackwell PB (2004) Identification and remediation of pediatric fluency and voice disorders. J Pediatr Health Care 2:87–94. https://doi.org/10.1016/j.pedhc.2003.09.008
Kuhn MA (2014) Histological changes in vocal fold growth and aging. Curr Opin Otolaryngol Head Neck Surg 6:460–465. https://doi.org/10.1097/moo.0000000000000108
Hartnick CJ, Rehbar R, Prasad V (2005) Development and maturation of the pediatric human vocal fold lamina propria. Laryngoscope 1:4–15. https://doi.org/10.1097/01.mlg.0000150685.54893.e9
Boseley ME, Hartnick CJ (2006) Development of the human true vocal fold: depth of cell layers and quantifying cell types within the lamina propria. Ann Otol Rhinol Laryngol 10:784–788. https://doi.org/10.1177/000348940611501012
Patel R, Donohue KD, Unnikrishnan H, Kryscio RJ (2015) Kinematic measurements of the vocal-fold displacement waveform in typical children and adult populations: quantification of high-speed endoscopic videos. J Speech Lang Hear Res 2:227–240. https://doi.org/10.1044/2015_jslhr-s-13-0056
Levendoski EE, Leydon C, Thibeault SL (2014) Vocal fold epithelial barrier in health and injury: a research review. J Speech Lang Hear Res 5:1679–1691. https://doi.org/10.1044/2014_jslhr-s-13-0283
Rousseau B, Suehiro A, Echemendia N, Sivasankar M (2011) Raised intensity phonation compromises vocal fold epithelial barrier integrity. Laryngoscope 2:346–351. https://doi.org/10.1002/lary.21364
Lee JM, Roy N, Park A, Muntz H, Redmond SM, Smith M (2022) Self-regulation in children with vocal fold nodules: a multilevel analysis. J Commun Disord 106203. https://doi.org/10.1016/j.jcomdis.2022.106203
Chaplin TM, Aldao A (2013) Gender differences in emotion expression in children: a meta-analytic review. Psychol Bull 4:735–765. https://doi.org/10.1037/a0030737
Chaplin TM (2015) Gender and emotion expression: a developmental contextual perspective. Emot Rev 1:14–21. https://doi.org/10.1177/1754073914544408
Boltezar IH, Burger ZR, Zargi M (1997) Instability of voice in adolescence: pathologic condition or normal developmental variation? J Pediatr 2:185–190. https://doi.org/10.1016/s0022-3476(97)70341-x
De Bodt MS, Ketelslagers K, Peeters T, Wuyts FL, Mertens F, Pattyn J, Heylen L, Peeters A, Boudewyns A, Van de Heyning P (2007) Evolution of vocal fold nodules from childhood to adolescence. J Voice 2:151–156. https://doi.org/10.1016/j.jvoice.2005.11.006
Liben LS, Bigler RS (2002) The developmental course of gender differentiation: conceptualizing, measuring, and evaluating constructs and pathways. Monogr Soc Res Child Dev 2:i-viii, 1–147; discussion 8–83.
Carding PN, Roulstone S, Northstone K (2006) The prevalence of childhood dysphonia: a cross-sectional study. J Voice 4:623–630. https://doi.org/10.1016/j.jvoice.2005.07.004
Smillie I, McManus K, Cohen W, Lawson E, Wynne DM (2014) The paediatric voice clinic. Arch Dis Child 10:912–915. https://doi.org/10.1136/archdischild-2013-305683
Lee JM, Roy N, Dietrich M (2019) Personality, psychological factors, and behavioral tendencies in children with vocal nodules: a systematic review. J Voice 6:945.e1-.e18. https://doi.org/10.1016/j.jvoice.2018.07.016
Lee JM, Roy N, Park A, Muntz H, Meier J, Skirko J, Smith M (2021) Personality in children with vocal fold nodules: a multitrait analysis. J Speech Lang Hear Res 10:3742–3758. https://doi.org/10.1044/2021_jslhr-21-00144
Tuzuner A, Demirci S, Oguz H, Ozcan KM (2017) Pediatric vocal fold nodule etiology: what are its usual causes in children? J Voice 4:506.e19-.e23. https://doi.org/10.1016/j.jvoice.2016.10.007
Kallvik E, Lindström E, Holmqvist S, Lindman J, Simberg S (2015) Prevalence of hoarseness in school-aged children. J Voice 2(260):e1-19. https://doi.org/10.1016/j.jvoice.2013.08.019
Reis-Rego Â, Santos PH, Santos G, Santos PC, Dias D, Vaz Freitas S, Carvalho I, Coutinho M, Feliciano T, Almeida C (2019) Behavioral profile of children with vocal fold nodules-a case-control study. J Voice 4:584.e1-.e4. https://doi.org/10.1016/j.jvoice.2018.02.009
Casper M, Abramson AL, Forman-Franco B (1981) Hoarseness in children: summer camp study. Int J Pediatr Otorhinolaryngol 1:85–89. https://doi.org/10.1016/0165-5876(81)90023-9
Clarós P, Porebska I, Clarós-Pujol A, Pujol C, Clarós A, López-Muñoz F, Kaczmarek KJJOH, Surgery N (2019) Association between the development of pediatric voice disorders and singing in children’s choir. 5:445–51
Schindler A, Capaccio P, Maruzzi P, Ginocchio D, Bottero A, Otraviani F (2007) Preliminary considerations on the application of the voice handicap index to paediatric dysphonia. Acta Otorhinolaryngol Ital 1:22–26
Boseley ME, Cunningham MJ, Volk MS, Hartnick CJ (2006) Validation of the Pediatric Voice-Related Quality-of-Life survey. Arch Otolaryngol Head Neck Surg 7:717–720. https://doi.org/10.1001/archotol.132.7.717
Zur KB, Cotton S, Kelchner L, Baker S, Weinrich B, Lee L (2007) Pediatric Voice Handicap Index (pVHI): a new tool for evaluating pediatric dysphonia. Int J Pediatr Otorhinolaryngol 1:77–82. https://doi.org/10.1016/j.ijporl.2006.09.004
Adriaansen A, Van Lierde K, Meerschman I, Everaert C, D'Haeseleer E (2022) Validity and Reliability of the Dutch Children’s Voice Handicap Index-10. J Voice. https://doi.org/10.1016/j.jvoice.2022.04.020
Krasnodębska P, Szkiełkowska A, Rosińska A, Skarżynski H (2020) Polish version of the pediatric Voice Handicap Index (pVHI). Int J Pediatr Otorhinolaryngol 110278. https://doi.org/10.1016/j.ijporl.2020.110278
Mesallam TA, Alabdulkarim B, AlQabbani AA, Bin Suhaym NA, AlAjlan S (2019) The Arabic translation, cultural adaptation, and validation of the pediatric voice-related quality of life survey. Int J Pediatr Otorhinolaryngol 2019:30–33. https://doi.org/10.1016/j.ijporl.2018.10.018
Lu D, Huang M, Li Z, Cheng IK, Yang H, Chen F, Wang H, Zou J (2019) Validation of the Mandarin Chinese version of the Pediatric Voice-Related Quality of Life (pVRQOL). J Voice 3:325–332. https://doi.org/10.1016/j.jvoice.2017.11.008
Salturk Z, Ozdemir E, Kumral TL, Sayin İ, Yelken K, Sari H, Berkiten G, Atar Y, Tutar B, Arslanoglu A et al (2018) Reliability and validation of the Turkish version of the Pediatric Voice-Related Quality of Life Survey. J Voice 4:514.e13-.e17. https://doi.org/10.1016/j.jvoice.2017.06.014
Lu D, Huang M, Cheng IK, Dong J, Yang H (2018) Comparison and correlation between the pediatric Voice Handicap Index and the Pediatric Voice-Related Quality-of-Life questionnaires. Medicine (Baltimore) 36:e11850. https://doi.org/10.1097/md.0000000000011850
Cohen W, Wynne DM (2015) Parent and child responses to the Pediatric Voice-Related Quality-of-Life Questionnaire. J Voice 3:299–303. https://doi.org/10.1016/j.jvoice.2014.08.004
Ricci-Maccarini A, De Maio V, Murry T, Schindler A (2013) Development and validation of the Children’s Voice Handicap Index-10 (CVHI-10). J Voice 2:258.e23-.e28. https://doi.org/10.1016/j.jvoice.2012.10.006
Ricci-Maccarini A, De Maio V, Murry T, Schindler A (2016) Development and validation of the Children’s Voice Handicap Index-10 for parents. J Voice 1:120–126. https://doi.org/10.1016/j.jvoice.2014.10.004
Yağcıoğlu D, Aydınlı FE, Aslan G, Kirazlı M, Köse A, Doğan N, Akbulut S, Yılmaz T, Özcebe E (2022) Development, validation, and reliability of the Teacher-Reported Pediatric Voice Handicap Index. Lang Speech Hear Serv Sch 1:69–87. https://doi.org/10.1044/2021_lshss-21-00033
Mackiewicz-Nartowicz H, Sinkiewicz A, Bielecka A (2011) Laryngovideostroboscopy in children–diagnostic possibilities and constraints. Int J Pediatr Otorhinolaryngol 8:1015–1017. https://doi.org/10.1016/j.ijporl.2011.05.006
Zacharias SR, Brehm SB, Weinrich B, Kelchner L, Tabangin M, de Alarcon A (2016) Feasibility of clinical endoscopy and stroboscopy in children with bilateral vocal fold lesions. Am J Speech Lang Pathol 4:598–604. https://doi.org/10.1044/2016_ajslp-15-0071
Zacharias SRC, de Alarcon A, Deliyski DD (2022) Quantitative analysis of vocal fold vibration using high-speed videoendoscopy in children with and without bilateral lesions. J Voice 2:176–182. https://doi.org/10.1016/j.jvoice.2020.05.009
Zacharias SRC, Deliyski DD, Gerlach TT (2018) Utility of laryngeal high-speed videoendoscopy in clinical voice assessment. J Voice 2:216–220. https://doi.org/10.1016/j.jvoice.2017.05.002
Deliyski DD, Powell ME, Zacharias SR, Gerlach TT, de Alarcon A (2015) Experimental investigation on minimum frame rate requirements of high-speed videoendoscopy for clinical voice assessment. Biomed Signal Process Control 2015:21–28. https://doi.org/10.1016/j.bspc.2014.11.007
Deliyski DD, Petrushev PP, Bonilha HS, Gerlach TT, Martin-Harris B, Hillman RE (2008) Clinical implementation of laryngeal high-speed videoendoscopy: challenges and evolution. Folia Phoniatr Logop 1:33–44. https://doi.org/10.1159/000111802
Phadke KV, Vydrová J, Domagalská R, Švec JG (2017) Evaluation of clinical value of videokymography for diagnosis and treatment of voice disorders. Eur Arch Otorhinolaryngol 11:3941–3949. https://doi.org/10.1007/s00405-017-4726-1
Lee MGY, Millar J, Rose E, Jones A, Wood D, Luitingh TL, Zannino D, Brink J, Konstantinov IE, Brizard CP et al (2018) Laryngeal ultrasound detects a high incidence of vocal cord paresis after aortic arch repair in neonates and young children. J Thorac Cardiovasc Surg 6:2579–2587. https://doi.org/10.1016/j.jtcvs.2017.12.133
Ongkasuwan J, Devore D, Hollas S, Jones J, Tran B (2017) Laryngeal ultrasound and pediatric vocal fold nodules. Laryngoscope 3:676–678. https://doi.org/10.1002/lary.26209
McLaughlin RA, Noble PB, Sampson DD (2014) Optical coherence tomography in respiratory science and medicine: from airways to alveoli. Physiology (Bethesda) 5:369–380. https://doi.org/10.1152/physiol.00002.2014
Sharma GK, Ahuja GS, Wiedmann M, Osann KE, Su E, Heidari AE, Jing JC, Qu Y, Lazarow F, Wang A et al (2015) Long-range optical coherence tomography of the neonatal upper airway for early diagnosis of intubation-related subglottic injury. Am J Respir Crit Care Med 12:1504–1513. https://doi.org/10.1164/rccm.201501-0053OC
Coughlan CA, Chou LD, Jing JC, Chen JJ, Rangarajan S, Chang TH, Sharma GK, Cho K, Lee D, Goddard JA et al (2016) In vivo cross-sectional imaging of the phonating larynx using long-range Doppler optical coherence tomography. Sci Rep 22792. https://doi.org/10.1038/srep22792
Benboujja F, Hartnick C (2018) Clinical and surgical implications of intraoperative optical coherence tomography imaging for benign pediatric vocal fold lesions. Int J Pediatr Otorhinolaryngol 111–119. https://doi.org/10.1016/j.ijporl.2018.08.036
Benboujja F, Greenberg M, Nourmahnad A, Rath N, Hartnick C (2021) Evaluation of the human vocal fold lamina propria development using optical coherence tomography. Laryngoscope 9:E2558–E2565. https://doi.org/10.1002/lary.29516
Gramuglia AC, Tavares EL, Rodrigues SA, Martins RH (2014) Perceptual and acoustic parameters of vocal nodules in children. Int J Pediatr Otorhinolaryngol 2:312–316. https://doi.org/10.1016/j.ijporl.2013.11.032
Reynolds V, Buckland A, Bailey J, Lipscombe J, Nathan E, Vijayasekaran S, Kelly R, Maryn Y, French N (2012) Objective assessment of pediatric voice disorders with the Acoustic Voice Quality Index. J Voice 5(672):e1-7. https://doi.org/10.1016/j.jvoice.2012.02.002
Bilal N, Selcuk T, Sarica S, Alkan A, Orhan İ, Doganer A, Sagiroglu S, Kılıc MA (2019) Voice acoustic analysis of pediatric vocal nodule patients using ratios calculated with biomedical image segmentation. J Voice 2:195–203. https://doi.org/10.1016/j.jvoice.2017.11.010
Meredith ML, Theis SM, McMurray JS, Zhang Y, Jiang JJ (2008) Describing pediatric dysphonia with nonlinear dynamic parameters. Int J Pediatr Otorhinolaryngol 12:1829–1836. https://doi.org/10.1016/j.ijporl.2008.09.004
Esen Aydinli F, Özcebe E, İncebay Ö (2019) Use of cepstral analysis for differentiating dysphonic from normal voices in children. Int J Pediatr Otorhinolaryngol 107–113. https://doi.org/10.1016/j.ijporl.2018.10.029
Demirci AN, Köse A, Aydinli FE, İncebay Ö, Yilmaz T (2021) Investigating the cepstral acoustic characteristics of voice in healthy children. Int J Pediatr Otorhinolaryngol 110815. https://doi.org/10.1016/j.ijporl.2021.110815
Hampala V, Garcia M, Švec JG, Scherer RC, Herbst CT (2016) Relationship between the electroglottographic signal and vocal fold contact area. J Voice 2:161–171. https://doi.org/10.1016/j.jvoice.2015.03.018
Patel RR, Ternström S (2021) Quantitative and qualitative electroglottographic wave shape differences in children and adults using voice map-based analysis. J Speech Lang Hear Res 8:2977–2995. https://doi.org/10.1044/2021_jslhr-20-00717
Szklanny K, Gubrynowicz R, Ratyńska J, Chojnacka-Wądołowska D (2019) Electroglottographic and acoustic analysis of voice in children with vocal nodules. Int J Pediatr Otorhinolaryngol 82–88. https://doi.org/10.1016/j.ijporl.2019.03.030
Hseu AF, Spencer G, Woodnorth G, Kagan S, Kawai K, Nuss RC (2021) Barriers to voice therapy in dysphonic children. J Voice. https://doi.org/10.1016/j.jvoice.2021.01.008
Feinstein H, Abbott KV (2021) Behavioral treatment for benign vocal fold lesions in children: a systematic review. Am J Speech Lang Pathol 2:772–788. https://doi.org/10.1044/2020_ajslp-20-00304
Hartnick C, Ballif C, De Guzman V, Sataloff R, Campisi P, Kerschner J, Shembel A, Reda D, Shi H, Sheryka Zacny E et al (2018) Indirect vs direct voice therapy for children with vocal nodules: a randomized clinical trial. JAMA Otolaryngol Head Neck Surg 2:156–163. https://doi.org/10.1001/jamaoto.2017.2618
Guzman M, Acuña G, Pacheco F, Peralta F, Romero C, Vergara C, Quezada C (2018) The impact of double source of vibration semioccluded voice exercises on objective and subjective outcomes in subjects with voice complaints. J Voice 6:770.e1-.e9. https://doi.org/10.1016/j.jvoice.2017.08.021
Meerschman I, Van Lierde K, Ketels J, Coppieters C, Claeys S, D’haeseleer E (2019) Effect of three semi-occluded vocal tract therapy programmes on the phonation of patients with dysphonia: lip trill, water-resistance therapy and straw phonation. Int J Lang Commun Disord 1:50–61
Zhuge P, You H, Wang H, Zhang Y, Du H (2016) An analysis of the effects of voice therapy on patients with early vocal fold polyps. J Voice 6:698–704. https://doi.org/10.1016/j.jvoice.2015.08.013
Hseu AF, Spencer G, Jo S, Kagan S, Thompson K, Woodnorth G, Nuss RC (2021) Telehealth for treatment of pediatric dysphonia. J Voice. https://doi.org/10.1016/j.jvoice.2021.11.007
van Leer E, Lewis B, Porcaro N (2021) Effect of an iOS app on voice therapy adherence and motivation. Am J Speech Lang Pathol 1:210–227. https://doi.org/10.1044/2020_ajslp-19-00213
de Oliveira AG, Fabbron EMG (2021) Play-based strategies for speech therapy and vocal health face-to-face and distance learning actions for children distance learning actions for children: an integrative literature review. J Voice. https://doi.org/10.1016/j.jvoice.2021.09.016
Watson NA, Orton KA, Hall A (2022) Fifteen-minute consultation: guide to paediatric voice disorders. Arch Dis Child Educ Pract Ed 2:101–104. https://doi.org/10.1136/archdischild-2020-321134
Ebersole B, Soni RS, Moran K, Lango M, Devarajan K, Jamal N (2018) The role of occupational voice demand and patient-rated impairment in predicting voice therapy adherence. J Voice 3:325–331. https://doi.org/10.1016/j.jvoice.2017.06.002
Starmer HM, Liu Z, Akst LM, Gourin C (2014) Attendance in voice therapy: can an interdisciplinary care model have an impact? Ann Otol Rhinol Laryngol 2:117–123
Braden MN, van Leer E, McConville K, Blakeslee SDM (2018) Patient, parent, and speech-language pathologists’ perceptions of pediatric voice therapy through interviews. Am J Speech Lang Pathol 4:1385–1404. https://doi.org/10.1044/2018_ajslp-17-0226
Fujiki RB, Thibeault SL (2022) Pediatric voice therapy: how many sessions to discharge? Am J Speech Lang Pathol 1–12. https://doi.org/10.1044/2022_ajslp-22-00111
Schöbinger R, Florin I, Reichbauer M, Lindemann H, Zimmer C (1993) Childhood asthma: mothers’ affective attitude, mother-child interaction and children’s compliance with medical requirements. J Psychosom Res 7:697–707. https://doi.org/10.1016/0022-3999(93)90098-z
Johnson PD, Cohen DA, Aiosa L, McGorray S, Wheeler T (1998) Attitudes and compliance of pre-adolescent children during early treatment of class II malocclusion. Clin Orthod Res 1:20–28. https://doi.org/10.1111/ocr.1998.1.1.20
Lee P, Zehgeer A, Ginsburg GS, McCracken J, Keeton C, Kendall PC, Birmaher B, Sakolsky D, Walkup J, Peris T et al (2019) Child and adolescent adherence with cognitive behavioral therapy for anxiety: predictors and associations with outcomes. J Clin Child Adolesc Psychol (sup1):S215–S226. https://doi.org/10.1080/15374416.2017.1310046
Chisholm V, Atkinson L, Donaldson C, Noyes K, Payne A, Kelnar C (2011) Maternal communication style, problem-solving and dietary adherence in young children with type 1 diabetes. Clin Child Psychol Psychiatry 3:443–458. https://doi.org/10.1177/1359104510373312
Clarke AT, Marshall SA, Mautone JA, Soffer SL, Jones HA, Costigan TE, Patterson A, Jawad AF, Power TJ (2015) Parent attendance and homework adherence predict response to a family-school intervention for children with ADHD. J Clin Child Adolesc Psychol 1:58–67. https://doi.org/10.1080/15374416.2013.794697
Chappuy H, Tréluyer JM, Faesch S, Giraud C, Chéron G (2010) Length of the treatment and number of doses per day as major determinants of child adherence to acute treatment. Acta Paediatr 3:433–437. https://doi.org/10.1111/j.1651-2227.2009.01601.x
Butcher JL, Nasr SZ (2015) Direct observation of respiratory treatments in cystic fibrosis: parent-child interactions relate to medical regimen adherence. J Pediatr Psychol 1:8–17. https://doi.org/10.1093/jpepsy/jsu074
Greening L, Stoppelbein L, Konishi C, Jordan SS, Moll G (2007) Child routines and youths’ adherence to treatment for type 1 diabetes. J Pediatr Psychol 4:437–447. https://doi.org/10.1093/jpepsy/jsl029
Ishizuya A, Enomoto M, Tachimori H, Takahashi H, Sugihara G, Kitamura S, Mishima K (2021) Risk factors for low adherence to methylphenidate treatment in pediatric patients with attention-deficit/hyperactivity disorder. Sci Rep 1:1707. https://doi.org/10.1038/s41598-021-81416-z
Drew LM, Berg C, Wiebe DJ (2010) The mediating role of extreme peer orientation in the relationships between adolescent-parent relationship and diabetes management. J Fam Psychol 3:299–306. https://doi.org/10.1037/a0019352
Baeyens D, Lierman A, Roeyers H, Hoebeke P, Walle JV (2009) Adherence in children with nocturnal enuresis. J Pediatr Urol 2:105–109. https://doi.org/10.1016/j.jpurol.2008.10.002
Modi AC, Morita DA, Glauser TA (2008) One-month adherence in children with new-onset epilepsy: white-coat compliance does not occur. Pediatrics 4:e961–e966. https://doi.org/10.1542/peds.2007-1690
Cheung K, Dierckx B, El Marroun H, Hillegers MHJ, Stricker BH, Visser LE (2021) Methylphenidate treatment adherence and persistence in children in the Netherlands. J Child Adolesc Psychopharmacol 3:205–213. https://doi.org/10.1089/cap.2020.0125
Medford E, Hare DJ, Carpenter K, Rust S, Jones S, Wittkowski A (2017) Treatment adherence and psychological wellbeing in maternal carers of children with phenylketonuria (PKU). JIMD Rep 107–114. https://doi.org/10.1007/8904_2017_23
Mackner LM, Crandall WV (2005) Oral medication adherence in pediatric inflammatory bowel disease. Inflamm Bowel Dis 11:1006–1012. https://doi.org/10.1097/01.mib.0000186409.15392.54
Pascoe JE, Sawnani H, Mayer OH, McConnell K, McDonough JM, White C, Rutkowski AM, Amin RS, Modi AC (2017) Adherence and barriers to hyperinsufflation in children with congenital muscular dystrophy. Pediatr Pulmonol 7:939–945. https://doi.org/10.1002/ppul.23645
Falkenstein K, Flynn L, Kirkpatrick B, Casa-Melley A, Dunn S (2004) Non-compliance in children post-liver transplant. Who are the culprits? Pediatr Transplant 3:233–6. https://doi.org/10.1111/j.1399-3046.2004.00136.x
Sonbay Yılmaz ND, Afyoncu C, Ensari N, Yıldız M, Gür Ö E (2021) The effect of the mother’s participation in therapy on children with vocal fold nodules. Ann Otol Rhinol Laryngol 11:1263–1267. https://doi.org/10.1177/00034894211002430
Kollbrunner J, Seifert E (2013) Functional hoarseness in children: short-term play therapy with family dynamic counseling as therapy of choice. J Voice 5:579–588. https://doi.org/10.1016/j.jvoice.2013.01.010
King SN, Davis L, Lehman JJ, Ruddy BH (2012) A model for treating voice disorders in school-age children within a video gaming environment. J Voice 5:656–663. https://doi.org/10.1016/j.jvoice.2011.08.002
Verdolini Abbott K (2013) Some guiding principles in emerging models of voice therapy for children. Semin Speech Lang 2:80–93. https://doi.org/10.1055/s-0033-1342979
Martins RHG, Siqueira DB, Dias NH, Gramuglia ACJ (2020) Laryngeal microsurgery for the treatment of vocal nodules and cysts in dysphonic children. Folia Phoniatr Logop 4:325–330. https://doi.org/10.1159/000502477
Pedersen M, McGlashan J (2012) Surgical versus non-surgical interventions for vocal cord nodules. Cochrane Database Syst Rev 6:Cd001934. https://doi.org/10.1002/14651858.CD001934.pub2
Hooper CR (2004) Treatment of voice disorders in children. Lang Speech Hear Serv Sch 4:320–326. https://doi.org/10.1044/0161-1461(2004/031)
Dohar JE, Shaffer AD, White KE (2019) Pediatric dysphonia: it’s not about the nodules. Int J Pediatr Otorhinolaryngol 147–152. https://doi.org/10.1016/j.ijporl.2019.06.031
Landa M, Palicio I, Álvarez L, Martínez Z (2017) A review of our experience in phonosurgery in children. Acta Otorrinolaringol Esp (Engl Ed) 5:269–273. https://doi.org/10.1016/j.otorri.2016.11.008
Hseu A, Ongkasuwan JJOCoNA (2019) Beyond nodules—diagnostic and treatment options in pediatric voice disorders 5:949–56
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Hui Yang and Sixi Yi had the idea for the article. Sixi Yi performed the literature search and data analysis. The first draft of the manuscript was written by Sixi Yi, Hui Yang critically revised the work. And, all authors commented on previous versions of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yi, S., Yang, H. Update on the pediatric adverse vocal behavior voice disorders: a clinical practice review. Eur J Pediatr 182, 2485–2497 (2023). https://doi.org/10.1007/s00431-023-04879-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-023-04879-4