Abstract
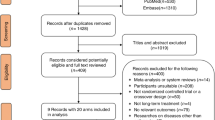
Nearly all asthma predictive tools estimate the future risk of asthma development. However, there is no tool to predict the probability of successful ICS cessation at an early age. Therefore, we aimed to determine the predictors of successful ICS cessation in preschool wheezers, and developed a simple predictive tool for clinical practice. This was a retrospective cohort study involving preschool wheezers who had undergone an ICS therapeutic trial during 2015–2020 at the University Hospital, Southern, Thailand. A predictive scoring system was developed using a nomogram to estimate the probability of successful ICS cessation. We calculated area under ROC curve and used a calibration plot for assessing the tool’s performance. A total of 131 medical records were eligible for analysis. Most of the participants were male (68.9%). More than half of the preschool wheezers had successful ICS cessation after an initial therapeutic trial regimen. The predictors of less successful ICS cessation were perinatal oxygen use [OR 0.10 (0.01, 0.70), P = 0.02], allergic rhinitis [OR 0.20 (0.08, 0.56), P = 0.002], blood eosinophil count > 500 cell/mm3 [OR 0.20 (0.06, 0.67), P = 0.008], and previous ICS use > 6 months [OR 0.30 (0.09, 0.72), P = 0.009].
Conclusions: Predictors of less successful ICS cessation were the following: perinatal oxygen use, allergic rhinitis, blood eosinophil count > 500 cell/mm3, and previous ICS use > 6 months. A simple predictive score developed in this study may help general practitioners to be more confident in making a decision regarding the discontinuation of ICS after initial therapeutic trials.
What is Known: • Early allergic sensitization is associated with reduced chances of inhaled corticosteroid cessation at school age. • Prolonged ICS is associated with the emergence of adverse effect and discontinuing too early can result in recurrence symptoms. | |
What is New: • Requirement of oxygen support within 7 days after birth in term neonate is a postnatal factor associated with less successful ICS cessation. • We propose a simple predictive tool with easily available clinical parameters (perinatal oxygen use, allergic rhinitis, blood eosinophil count, parental asthma history, and duration of previous ICS use) to determine the timing of inhalational corticosteroid cessation in preschool wheezers. |



Similar content being viewed by others
Abbreviations
- AUC:
-
Area under the curve
- GINA:
-
Global Initiative for Asthma
- ICS:
-
Inhaled corticosteroids
- ROC:
-
Receiver operating characteristics curve
- SABA:
-
Short-acting beta-2-agonist
References
Ozdogan S, Tabakci B, Demirel AS et al (2015) The evaluation of risk factors for recurrent hospitalizations resulting from wheezing attacks in preschool children. Ital J Pediatr 41:91. https://doi.org/10.1186/s13052-015-0201-z
Mallol J, García-Marcos L, Solé D et al (2010) International prevalence of recurrent wheezing during the first year of life: variability, treatment patterns and use of health resources. Thorax 65:1004. https://doi.org/10.1136/thx.2009.115188
Global Initiative for Asthma (2022) Global strategy for asthma management and prevention
Fitzpatrick AM, Bacharier LB, Guilbert TW et al (2019) Phenotypes of recurrent wheezing in preschool children: Identification by latent class analysis and utility in prediction of future exacerbation. J Allergy Clin Immunol Pract 7:915-924.e7. https://doi.org/10.1016/j.jaip.2018.09.016
Guilbert TW, Mauger DT, Lemanske RF (2014) Childhood asthma-predictive phenotype. J Allergy Clin Immunol Pract 2:664–670. https://doi.org/10.1016/j.jaip.2014.09.010
Zeiger RS, Mauger D, Bacharier LB et al (2011) Daily or intermittent budesonide in preschool children with recurrent wheezing. N Engl J Med 365:1990–2001. https://doi.org/10.1056/NEJMoa1104647
Guilbert TW, Boehmer SJ, Strunk RC et al (2006) Long-term inhaled corticosteroids in preschool children at high risk for asthma. N Engl J Med 13
Fainardi V, Santoro A, Caffarelli C (2020) Preschool wheezing: trajectories and long-term treatment. Front Pediatr 8. https://doi.org/10.3389/fped.2020.00240
Sitthisarunkul N, Sangsupawanich P, Anuntaseree W (2016) Negative skin prick test predicts asthma remission in preschool children. J Allergy Clin Immunol 4864:AB1. https://doi.org/10.1016/j.jaci.2015.12.011
Longo C, Blais L, Brownell M et al (2021) Association between asthma control trajectories in preschoolers and disease remission. Eur Respir J 57:2001897. https://doi.org/10.1183/13993003.01897-2020
Wanlapakorn N, Sritippayawan S, Deerojanawong J (2014) Prevalence of asthma, level of control and factors associated with asthma control in Thai elementary school students in Bangkok. Asian Pac J Allergy Immunol. 32:287–292. https://doi.org/10.12932/AP0464.32.4.2014
Wang AL, Datta S, Weiss ST, Tantisira KG (2019) Remission of persistent childhood asthma: Early predictors of adult outcomes. J Allergy Clin Immunol 143:1752-1759.e6. https://doi.org/10.1016/j.jaci.2018.09.038
Bao Y, Chen Z, Liu E et al (2017) Risk factors in preschool children for predicting asthma during the preschool age and the early school age: a systematic review and meta-analysis. Curr Allergy Asthma Rep 17:85. https://doi.org/10.1007/s11882-017-0753-7
Andersson M, Hedman L, Sundberg S et al (2011) Remission of childhood asthma in adolescence – a longitudinal study. Eur Respir J 38:p317
To T, Gershon A, Wang C et al (2007) Persistence and remission in childhood asthma: a population-based asthma birth cohort study. Arch Pediatr Adolesc Med 161:1197–1204. https://doi.org/10.1001/archpedi.161.12.1197
Becker A, Watson W, Ferguson A et al (2004) The Canadian asthma primary prevention study: Outcomes at 2 years of age. J Allergy Clin Immunol 113:650–656. https://doi.org/10.1016/j.jaci.2004.01.754
Wen H-J, Chiang T-L, Lin S-J, Guo YL (2015) Predicting risk for childhood asthma by pre-pregnancy, perinatal, and postnatal factors. Pediatr Allergy Immunol 26:272–279. https://doi.org/10.1111/pai.12374
Britt RD Jr, Faksh A, Vogel E et al (2013) Perinatal factors in neonatal and pediatric lung diseases. Expert Rev Respir Med 7:515–531. https://doi.org/10.1586/17476348.2013.838020
Caudri D, Wijga AA, Schipper CM et al (2009) Predicting the long-term prognosis of children with symptoms suggestive of asthma at preschool age. J Allergy Clin Immunol 124:903-910.e7. https://doi.org/10.1016/j.jaci.2009.06.045
Rönmark E, Jönsson E, Platts-Mills T, Lundbäck B (2001) Incidence and remission of asthma in schoolchildren: Report from the obstructive lung disease in northern Sweden studies. Pediatrics 107:e37–e37. https://doi.org/10.1542/peds.107.3.e37
Acknowledgements
We would like to thank Kittisakdi Choomalee, biostatistician, Department of epidemiology and the Office of International Affairs, Faculty of Medicine, Prince of Songkla University for their English editing services.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation was performed by Kanokpan Ruangnapa, Pharsai Prasertsan, and Kantara Saelim. Data collection, analysis, and first draft of manuscript were performed by Kantisa Sirianansopa. Utcharee Intusoma and Wanaporn Anuntaseree commented on previous version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This research was approved by Human Research Ethic Committee (REC. 65-059-1-1), Faculty of Medicine, Prince of Songkla University, Thailand. The study was performed in accordance with the ethical standards as laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to participate
The requirement for informed consents was waived because of the retrospective nature of the data.
Consent for publication
This paper did not include identifiable data or images.
Competing interests
The authors declare no competing interests.
Additional information
Communicated by Tobias Tenenbaum
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sirianansopa, K., Ruangnapa, K., Prasertsan, P. et al. Probability of successful inhaled corticosteroids cessation in preschool wheezers: a predictive score. Eur J Pediatr 182, 237–244 (2023). https://doi.org/10.1007/s00431-022-04679-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04679-2