Abstract
To assess the effect of pro- and synbiotics in the eradication therapy of Helicobacter pylori (Hp), as well as their effect on adverse effects and therapy compliance in children, a review was performed. We searched for relevant studies published in the English language in PubMed in the last 5 years. Articles were extracted using subject heading and keywords of interest to the topic. There is low-quality evidence that Lactobacillus casei, Bifidobacterium infantis, and Clostridium butyricum (only one RCT for all three) and Saccharomyces boulardii (more than 1 RCT) increase the eradication rate and decrease the adverse effects. Data with synbiotics report only a trend towards a better eradication. Heterogeneity in study designs and outcomes is a major limitation to propose evidence-based recommendations. A reduced incidence of antibiotic-associated diarrhoea is reported. Therapy compliance has been poorly studied.
Conclusion: Due to study heterogeneity, there is very low evidence that some specific probiotics strains increase the eradication rate of Hp when added to standard eradication therapy in children. Whether this is related to immunological effects of the strain or a decrease of adverse effects is not known. More studies, especially comparative trials, are needed before the addition of pro- or synbiotics to Hp eradication treatment can be recommended in daily routine.
What is Known: • Eradication treatment of Helicobacter pylori in children has a low success rate and induces frequently adverse effects. • The addition of probiotics might improve eradication and decrease adverse effects, but no paediatric guideline does recommend probiotics as part of the eradication treatment. | |
What is New: • There is low-quality evidence that Lactobacillus casei, Bifidobacteria infantis, and Clostridium butyricum (only one randomized controlled trial (RCT) for all three) and Saccharomyces boulardii (more than 1 RCT) increase the eradication rate and decrease the adverse effects. • Data with synbiotics report only a trend towards a better eradication. |
Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
Abbreviations
- AAD:
-
Antibiotic-associated diarrhoea
- B:
-
Bifidobacterium
- C:
-
Clostridium
- CFU:
-
Colony form unit
- CI:
-
Confidence interval
- ESPGHAN :
-
European Society for Paediatric Gastroenterology, Hepatology and Nutrition
- Hp:
-
Helicobacter pylori
- ISAPP:
-
International Scientific Organization for Probiotics and Prebiotics
- L:
-
Lactobacillus
- NASPGHAN :
-
North American Society for Pediatric Gastroenterology, Hepatology and Nutrition
- PPI:
-
Proton pump inhibitor
- RCT:
-
Randomized controlled trial
- RR:
-
Relative risk
- S:
-
Saccharomyces
References
Kotilea K, Bontems P, Touati E (2019) Epidemiology, diagnosis and risk factors of Helicobacter pylori infection. Adv Exp Med Biol 11(49):17–33. https://doi.org/10.1007/5584_2019_357
O’Connor A, O’Morain CA, Ford AC (2017) Population screening and treatment of Helicobacter pylori infection. Nat Rev Gastroenterol Hepatol 14(4):230–240. https://doi.org/10.1038/nrgastro.2016.195
Debowski AW, Walton SM, Chua EG et al (2017) Helicobacter pylori gene silencing in vivo demonstrates urease is essential for chronic infection. PLoS Pathog 13(6):e1006464. https://doi.org/10.1371/journal.ppat.1006464
Yonezawa H, Osaki T, Hojo F, Kamiya S (2019) Effect of Helicobacter pylori biofilm formation on susceptibility to amoxicillin, metronidazole and clarithromycin. Microb Pathog 132:100–108. https://doi.org/10.1016/j.micpath.2019.04.030
Mori M, Suzuki H, Suzuki M, Kai A, Miura S, Ishii H (1997) Catalase and superoxide dismutase secreted from Helicobacter pylori. Helicobacter 2(2):100–105. https://doi.org/10.1111/j.1523-5378.1997.tb00067.x
Qureshi N, Li P, Gu Q (2019) Probiotic therapy in Helicobacter pylori infection: a potential strategy against a serious pathogen? Appl Microbiol Biotechnol 103(4):1573–1588. https://doi.org/10.1007/s00253-018-09580-3
de Jesus Souza M, de Moraes JA, Da Silva VN et al (2019) Helicobacter pylori urease induces pro-inflammatory effects and differentiation of human endothelial cells: Cellular and molecular mechanism. Helicobacter 24(3):e12573. https://doi.org/10.1111/hel.12573
Bernardini G, Figura N, Ponzetto A, Marzocchi B, Santucci A (2017) Application of proteomics to the study of Helicobacter pylori and implications for the clinic. Expert Rev Proteomics 14(6):477–490. https://doi.org/10.1080/14789450.2017.1331739
Malfertheiner P, Megraud F, O’Morain C et al (2017) Management of Helicobacter pylori infection-the Maastricht V/Florence consensus report. Gut 66(1):6–30. https://doi.org/10.1136/gutjnl-2016-312288
Jones NL, Koletzko S, Goodman K et al (2017) Joint ESPGHAN/NASPGHAN Guidelines for the management of Helicobacter pylori in children and adolescents (Update 2016). J Pediatr Gastroenterol Nutr 64(6):991–1003. https://doi.org/10.1097/MPG.0000000000001594
Dang Y, Reinhardt JD, Zhou X, Zhang G (2014) The effect of probiotics supplementation on Helicobacter pylori eradication rates and side effects during eradication therapy: a meta-analysis. PLoS One 9(11):e111030. https://doi.org/10.1371/journal.pone.0111030
Thung I, Aramin H, Vavinskaya V et al (2016) Review article: the global emergence of Helicobacter pylori antibiotic resistance. Aliment Pharmacol Ther 43(4):514–533. https://doi.org/10.1111/apt.13497
Hill C, Guarner F, Reid G et al (2014) Expert consensus document. The International Scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol 11(8):506–514. https://doi.org/10.1038/NRGASTRO.2014.66
Swanson KS, Gibson GR, Hutkins R et al (2020) The International Scientific Association for Probiotics and Prebiotics (ISAPP) consensus statement on the definition and scope of synbiotics. Nat Rev Gastroenterol Hepatol 17(11):687–701. https://doi.org/10.1038/s41575-020-0344-2
Rodes L, Khan A, Paul A et al (2013) Effect of probiotics Lactobacillus and Bifidobacterium on gut-derived lipopolysaccharides and inflammatory cytokines: an in vitro study using a human colonic microbiota model. J Microbiol Biotechnol 23(4):518–526. https://doi.org/10.4014/jmb.1205.05018
Malfertheiner P, Megraud F, O’Morain C et al (2007) Current concepts in the management of Helicobacter pylori infection: The maastricht III consensus report. Gut 56(6):772–781. https://doi.org/10.1136/gut.2006.101634
Feng JR, Wang F, Qiu X et al (2017) Efficacy and safety of probiotic-supplemented triple therapy for eradication of Helicobacter pylori in children: a systematic review and network meta-analysis. Eur J Clin Pharmacol 73(10):1199–1208. https://doi.org/10.1007/s00228-017-2291-6
Wen J, Peng P, Chen P et al (2017) Probiotics in 14-day triple therapy for Asian pediatric patients with Helicobacter pylori infection: a network meta-analysis. Oncotarget 8(56):96409–96418. https://doi.org/10.18632/oncotarget.21633
Szajewska H, Kołodziej M (2015) Systematic review with meta-analysis: Saccharomyces boulardii in the prevention of antibiotic-associated diarrhoea. Aliment Pharmacol Ther 42(7):793–801. https://doi.org/10.1111/apt.13344
Fang HR, Zhang GQ, Cheng JY, Li ZY (2019) Efficacy of Lactobacillus-supplemented triple therapy for Helicobacter pylori infection in children: a meta-analysis of randomized controlled trials. Eur J Pediatr 178(1):7–16. https://doi.org/10.1007/s00431-018-3282-z
Zhou BG, Chen LX, Li B, Wan LY, Ai YW (2019) Saccharomyces boulardii as an adjuvant therapy for Helicobacter pylori eradication: a systematic review and meta-analysis with trial sequential analysis. Helicobacter 24(5):e12651. https://doi.org/10.1111/hel.12651
Pourmasoumi M, Najafgholizadeh A, Hadi A, Mansour-Ghanaei F, Joukar F (2019) The effect of synbiotics in improving Helicobacter pylori eradication: a systematic review and meta-analysis. Complement Ther Med 43:36–43. https://doi.org/10.1016/J.CTIM.2019.01.005
Şirvan BN, Usta MK, Kızılkan NU, Urgancı N (2017) Are synbiotics added to the standard therapy to eradicate Helicobacter pylori in children beneficial? A randomized controlled study. Euroasian J hepato-gastroenterology 7(1):17–22. https://doi.org/10.5005/JP-JOURNALS-10018-1205
Ustundag GH, Altuntas H, Soysal YD, Kokturk F (2017) The effects of synbiotic “Bifidobacterium lactis B94 plus Inulin” addition on standard triple therapy of Helicobacter pylori eradication in children. Can J Gastroenterol Hepatol 2017:8130596. https://doi.org/10.1155/2017/8130596
Szymański H, Młynarz P, Qasem B et al (2020) Post hoc analysis of fecal samples from responders and non-responders to Lactobacillus reuteri DSM 17938 intervention. Acta Biochim Pol 67(3):393–399. https://doi.org/10.18388/ABP.2020_5344
Paparo L, Tripodi L, Bruno C et al (2020) Protective action of Bacillus clausii probiotic strains in an in vitro model of Rotavirus infection. Sci Rep 10(1):12636. https://doi.org/10.1038/S41598-020-69533-7
Mourey F, Sureja V, Kheni D et al (2020) A Multicenter, randomized, double-blind, placebo-controlled trial of Saccharomyces boulardii in infants and children with acute diarrhea. Pediatr Infect Dis J 39(11):E347–E351. https://doi.org/10.1097/INF.0000000000002849
Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, McQuay HJ (1996) Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials 17:1–1
Rücker G, Schwarzer G (2015) Ranking treatments in frequentist network meta-analysis works without resampling methods. BMC Med Res Methodol 15:58. https://doi.org/10.1186/S12874-015-0060-8
Mack DR, Michail S, Wei S et al (1999) Probiotics inhibit enteropathogenic E. coli adherence in vitro by inducing intestinal mucin gene expression. Am J Physiol 276(4):G941–G950. https://doi.org/10.1152/ajpgi.1999.276.4.G941
Del Piano M, Anderloni A, Balzarini M et al (2012) The innovative potential of Lactobacillus rhamnosus LR06, Lactobacillus pentosus LPS01, Lactobacillus plantarum LP01, and Lactobacillus delbrueckii Subsp. delbrueckii LDD01 to restore the “gastric barrier effect” in patients chronically treated with PPI: a pilot study. J Clin Gastroenterol 46(Suppl):S18-26. https://doi.org/10.1097/MCG.0b013e318267b55d
Wang K-Y, Li S-N, Liu C-S et al (2004) Effects of Ingesting Lactobacillus-and Bifidobacterium-Containing yogurt in subjects with colonized Helicobacter pylori. Am J Clin Nutr 80(3):737–741. https://doi.org/10.1093/ajcn/80.3.737
Haller D, Holt L, Parlesak A et al (2004) Differential effect of immune cells on non-pathogenic Gram-negative bacteria-induced nuclear factor-kappaB activation and pro-inflammatory gene expression in intestinal epithelial cells. Immunology 112(2):310–320. https://doi.org/10.1111/J.1365-2567.2004.01874.X
Sykora J, Valeckova K, Amlerova J et al (2005) Effects of a specially designed fermented milk product containing probiotic Lactobacillus casei DN-114 001 and the eradication of H. pylori in children: a prospective randomized double-blind study. J Clin Gastroenterol 39(8):692–698. https://doi.org/10.1097/01.mcg.0000173855.77191.44.
Pewińska EM, Płaneta-Małecka I, Bąk-Romaniszyn L, MałeckaPanas E (2006) Probiotics in the treatment of Helicobacter pylori infection in children. Gastroenterol Polska 13(4):315–319
Szajewska H, Albrecht P, Topczewska-Cabanek A (2009) Randomized, double-blind, placebo-controlled trial: effect of Lactobacillus GG supplementation on Helicobacter pylori eradication rates and side effects during treatment in children. J Pediatr Gastroenterol Nutr 48(4):431–436
Hurduc V, Plesca D, Dragomir D, Sajin M, Vandenplas Y (2009) A randomized, open trial evaluating the effect of Saccharomyces boulardii on the eradication rate of Helicobacter pylori infection in children. Acta Pædiatrica 98(1):127–131. https://doi.org/10.1111/J.1651-2227.2008.00977.X
Zhao HM, Ou-Yang HJ, Duan BP et al (2014) Clinical effect of triple therapy combined with Saccharomyces boulardii in the treatment of Helicobacter pylori infection in children. Zhongguo Dang Dai Er Ke Za Zhi 16(3):230–233. https://doi.org/10.7499/j.issn.1008-8830.2014.03.002
Bin Z, Ya-Zheng X, Zhao-Hui D, Bo C, Li-Rong J, Vandenplas Y (2015) The efficacy of Saccharomyces boulardii CNCM I-745 in addition to standard Helicobacter pylori eradication treatment in children. Pediatr Gastroenterol Hepatol Nutr 18(1):17–22. https://doi.org/10.5223/PGHN.2015.18.1.17
Gotteland M, Poliak L, Cruchet S, Brunser O (2005) Effect of regular ingestion of Saccharomyces boulardii plus inulin or Lactobacillus acidophilus LB in children colonized by Helicobacter pylori. Acta Paediatr 94(12):1747–1751. https://doi.org/10.1111/J.1651-2227.2005.TB01848
Levy EI, Hoang DM, Vandenplas Y (2020) The effects of proton pump inhibitors on the microbiome in young children. Acta Paediatr 109(8):1531–1538. https://doi.org/10.1111/APA.15213
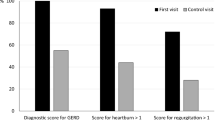
Belei O, Olariu L, Dobrescu A, Marcovici T, Marginean O (2018) Is it useful to administer probiotics together with proton pump inhibitors in children with gastroesophageal reflux? J Neurogastroenterol Motil 24(1):51–57. https://doi.org/10.5056/JNM17059
Cárdenas PA, Garcés D, Prado-Vivar B et al (2020) Effect of Saccharomyces boulardii CNCM I-745 as complementary treatment of Helicobacter pylori infection on gut microbiome. Eur J Clin Microbiol Infect Dis 39(7):1365–1372. https://doi.org/10.1007/s10096-020-03854-3
Depoorter L, Vandenplas Y (2021) Probiotics in pediatrics. A review and practical guide. Nutrients 13(7):2176. https://doi.org/10.3390/NU13072176
Homan M, Orel R (2015) Are probiotics useful in Helicobacter pylori eradication? World J Gastroenterol 21(37):10644–10653. https://doi.org/10.3748/wjg.v21.i37.10644
Song H, Zhou L, Liu D, Ge L, Li Y (2019) Probiotic effect on Helicobacter pylori attachment and inhibition of inflammation in human gastric epithelial cells. Exp Ther Med 18(3):1551–1562. https://doi.org/10.3892/etm.2019.7742
Johnston BC, Ma SSY, Goldenberg JZ et al (2012) Probiotics for the prevention of Clostridium difficile-associated diarrhea: a systematic review and meta-analysis. Ann Intern Med 157(12):878–888. https://doi.org/10.7326/0003-4819-157-12-201212180-00563
Rodgers BM, Kirley KM, Mounsey AM (2013) Pair it with probiotics. J Fam Pract 62(3):148–150. www.jfponline.com. Accessed 10 Jan 2021
Reid G (2005) The importance of guidelines in the development and application of probiotics. Curr Pharm Des 11(1):11–16. https://doi.org/10.2174/1381612053382395
Ji J, Yang H (2020) Using probiotics as supplementation for Helicobacter pylori antibiotic therapy. Int J Mol Sci 21(3):1136. https://doi.org/10.3390/ijms21031136
Goderska K, Agudo Pena S, Alarcon T (2018) Helicobacter pylori treatment: antibiotics or probiotics. Appl Microbiol Biotechnol 102(1):1–7. https://doi.org/10.1007/s00253-017-8535-7
Lesbros-Pantoflickova D, Corthésy-Theulaz I, Blum AL (2007) Helicobacter pylori and probiotics. In: Journal of Nutrition. Vol 137. American Institute of Nutrition 137(3 Suppl 2):812S-818S. https://doi.org/10.1093/jn/137.3.812s
Saxelin M, Tynkkynen S, Mattila-Sandholm T, De Vos WM (2005) Probiotic and other functional microbes: from markets to mechanisms. Curr Opin Biotechnol 16(2):204–211. https://doi.org/10.1016/j.copbio.2005.02.003
Author information
Authors and Affiliations
Contributions
S. Daelemans and V. Deseck did the literature search and wrote the first draft. E.I. Levy and Y. Vandenplas critically reviewed and revised the manuscript for important intellectual content. Y. Vandenplas conceptualized the study. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Communicated by Peter de Winter
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Sari Daelemans and Virginie Deseck share first authorship.
Contents summary
Some pro- and synbiotics improve the eradication of Helicobacter pylori but comparative trials are needed to allow evidence-based recommendations.
Key notes
• Antibiotic resistance of Helicobacter pylori increases worldwide.
• Pro- and synbiotics can increase the eradication rate of standard therapy and decrease adverse effects. There is low-quality evidence that Lactobacillus casei, Bifidobacterium infantis, and Clostridium butyricum (only one RCT for all three) and Saccharomyces boulardii (more than 1 RCT) increase the eradication rate. It is unclear which probiotic is the most effective.
• There is insufficient information on the effect of pro- and synbiotics on therapy compliance.
• Cost-effectiveness of eradication therapy may improve when probiotics are added to the eradication treatment.
Rights and permissions
About this article
Cite this article
Daelemans, S., Deseck, V., Levy, E.I. et al. Are pro- and/or synbiotics beneficial in Helicobacter pylori eradication therapy in children? A narrative review. Eur J Pediatr 181, 3225–3234 (2022). https://doi.org/10.1007/s00431-022-04523-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-022-04523-7