Abstract
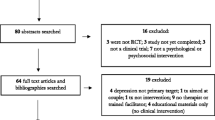
Perinatal (antenatal and postpartum) depression is increasingly becoming a global public health problem. Studies have shown that the presence of depression during the perinatal period impact on a mother’s ability to adequately provide nutritional care for herself and her infants and young children. This may thus negatively influence the nutritional status of these vulnerable children resulting in poor growth, such as stunting which is currently a public health problem in low- and middle-income countries (LMICs). The aim of this systematic review and meta-analysis was to determine the association between maternal postpartum depression and child growth in LMICs. Electronic databases were systematically reviewed by screening abstracts, titles, full text and additional data sources of eligible papers. Articles were eligible for inclusion if based on children aged 0 to 59 months, if reporting maternal postpartum depression as an exposure, if based on observational studies evaluating the relation between maternal postpartum depression and child growth, if reporting at least one physical growth indicator such as stunting as an outcome, and if published after 2000. Article selection was based on the PRISMA guidelines for reporting systematic reviews. Twelve articles were included in the quantitative synthesis (12 for stunting, 8 for underweight and 2 for wasting). Maternal postpartum depression was observed to be associated with an increased risk of child stunting (1.87 (95% CI: 1.52, 2.30; I2 = 41.6%, p = 0.064)) and underweight (1.81 (95% Cl: 1.25, 2.62; I2 = 70.7%, p = 0.001)). These results were confirmed after influence analyses, with publication bias being negligible.
Conclusion: Maternal depression is a risk factor for poor child growth in LMICs. This study contributes to the knowledge on this topic and calls on policymakers to improve on its understanding, screening and treatment to alleviate the potential negative impact on child growth.
What is Known: • Maternal postpartum depression is currently a public health relevance in low- and middle-income countries (LMICs). • Maternal postpartum depression is a risk factor for poor nutritional status in children from LMICs. | |
What is New: • Maternal postpartum depression is associated with an 80 to 90% increased risk of childhood stunting and underweight in LMICs. • The association between risk of childhood stunting and underweight with maternal postpartum depression is slightly influenced by geographical area, rural or urban location, by factors such as study design, study quality and sample size. |


Similar content being viewed by others
Availability of data and material
N/A.
Code availability
N/A.
Abbreviations
- Cl:
-
Confident limit
- HRs:
-
Hazard ratios
- L/HAZ:
-
Length/Height-for-Age Z-score
- LMICs:
-
Low- and middle-income countries
- MeSH:
-
Medical Subject Headings
- NOS:
-
New castle Ottawa Scale
- ORs:
-
Odds ratios
- PECO (ST):
-
Population, Exposure, Comparison, Outcome, Study design, Time
- RR:
-
Relative risk
- RRs:
-
Relative risks
- WAZ:
-
Weight-for-age Z-score
- WHO:
-
World Health Organization
- WLZ:
-
Weight-for-length/height Z-score
References
UNICEF (United Nation Children’s Funds), WHO (World Health Organization), World Bank (2020) NICEF/WHO/The World Bank Group joint child malnutrition estimates: levels and trends in child malnutrition: key findings of the 2020 edition. https://www.who.int/publications/i/item/jme-2020-edition (accessed 26 June 2020)
Shidhaye P, Giri P (2014) Maternal depression: a hidden burden in developing countries, (in eng). Ann Med Health Sci Res 4(4):463–465. https://doi.org/10.4103/2141-9248.139268
Stewart CP, Iannotti L, Dewey KG, Michaelsen KF, Onyango AW (2013) Contextualising complementary feeding in a broader framework for stunting prevention. Matern Child Nutr 9(2):27–45. https://doi.org/10.1111/mcn.12088
Segre SL, Davis NW (2013) Postpartum depression and perinatal mood disorders in the DSM. https://www.postpartum.net (accessed 9 Sept, 2021)
Woody CA, Ferrari AJ, Siskind DJ, Whiteford HA, Harris MG (2017) A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J Affect Disord vol. 219, pp. 86–92, /09/01/2017. https://doi.org/10.1016/j.jad.2017.05.003
Herba CM, Glover V, Ramchandani PG, Rondon MB (2016) Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. Lancet Psychiatry 3(10):983–992. https://doi.org/10.1016/S2215-0366(16)30148-1
American Psychiatric Association (2020) Depression. https://www.psychiatry.org/patients-families/depression/what-is-depression (accessed 18 Aug, 2021)
Marcus M, Yasamy MT, van Ommeren Mv, Chisholm D, Saxena S (2012) Depression: a global pub health concern
Sontag-Padilla L, Schultz D, Reynolds K, Lovejoy SL, Firth R (2013) Maternal depression: Implications for systems serving mother and child. https://www.rand.org/pubs/research_reports/RR404.html (accessed 06 November, 2020)
Stewart RC et al (2008) Maternal common mental disorder and infant growth–a cross-sectional study from Malawi. Matern Child Nutr 4(3):209–219. https://doi.org/10.1111/j.1740-8709.2008.00147.x
Nguyen PH et al (2014) Maternal mental health is associated with child undernutrition and illness in Bangladesh. Vietnam and Ethiopia, Public Health Nutr 17(6):1318–1327. https://doi.org/10.1017/S1368980013001043
Harpham T, Huttly S, De Silva MJ, Abramsky T (2005) Maternal mental health and child nutritional status in four developing countries. J Epidemiol Community Health 59(12):1060–1064. https://doi.org/10.1136/jech.2005.039180
Girma S, Fikadu T, Abdisa E (2019) Maternal common mental disorder as predictors of stunting among children aged 6–59 months in Western Ethiopia: a case-control study. Int J Pediatr 2019:4716482. https://doi.org/10.1155/2019/4716482
Tomlinson M, Cooper P, Stein A, Swartz L, Molteno C (2006) Post-partum depression and infant growth in a South African peri-urban settlement. Child Care Health Dev 32(1):81–86. https://doi.org/10.1111/j.1365-2214.2006.00598.x
Surkan PJ, Kawachi I, Ryan LM, Berkman LF, Carvalho Vieira LM, Peterson KE (2008) Maternal depressive symptoms, parenting self-efficacy, and child growth. Am J Public Health vol. 98, no. 1, pp. 125–132. https://doi.org/10.2105/AJPH.2006.108332
Rahman A, Iqbal Z, Bunn J, Lovel H, Harrington R (2004) Impact of maternal depression on infant nutritional status and illness: a cohort study. Arch Gen Psychiatry 61(9):946–952. https://doi.org/10.1001/archpsyc.61.9.946
Patel V, DeSouza N, Rodrigues M (2003) Postnatal depression and infant growth and development in low income countries: a cohort study from Goa. India, Arch Dis Child 88(1):34–37. https://doi.org/10.1136/adc.88.1.34
Wemakor A, Mensah KA (2016) Association between maternal depression and child stunting in Northern Ghana: a cross-sectional study. BMC Public Health vol. 16, no. 1, p. 869. Aug 24 2016. https://doi.org/10.1186/s12889-016-3558-z
Wemakor A, Iddrisu H (2018) Maternal depression does not affect complementary feeding indicators or stunting status of young children (6–23 months) in Northern Ghana. BMC Res Notes vol. 11, no. 1, p. 408. Jun 25 2018. https://doi.org/10.1186/s13104-018-3528-x
Ndokera R, MacArthur C (2011) The relationship between maternal depression and adverse infant health outcomes in Zambia: a cross-sectional feasibility study. Child Care Health Dev 37(1):74–81. https://doi.org/10.1111/j.1365-2214.2010.01129.x
Ertel KA, Koenen KC, Rich-Edwards JW, Gillman MW (2010) Maternal depressive symptoms not associated with reduced height in young children in a US prospective cohort study. PLoS One vol. 5, no. 10, p. e13656. 27 October 2010. https://doi.org/10.1371/journal.pone.0013656
Black MM, Baqui AH, Zaman K, El Arifeen S, Black RE (2009) Maternal depressive symptoms and infant growth in rural Bangladesh. Am J Clin Nutr 89(3):951S-957S. https://doi.org/10.3945/ajcn.2008.26692E
Avan B, Richter LM, Ramchandani PG, Norris SA, Stein A (2010) Maternal postnatal depression and children’s growth and behaviour during the early years of life: exploring the interaction between physical and mental health. Arch Dis Child 95(9):690–695. https://doi.org/10.1136/adc.2009.164848
Ashaba S, Rukundo GZ, Beinempaka F, Ntaro M, LeBlanc JC (2015) Maternal depression and malnutrition in children in southwest Uganda: a case control study. BMC Public Health vol. 15, p. 1303. Dec 28 2015. https://doi.org/10.1186/s12889-015-2644-y
Anato A, Baye K, Tafese Z, Stoecker BJ (2020) Maternal depression is associated with child undernutrition: a cross-sectional study in Ethiopia. Matern Child Nutr 16(3):e12934. https://doi.org/10.1111/mcn.12934
Page MJ, The PRISMA et al (2020) statement: an updated guideline for reporting systematic reviews. BMJ 372(n71):2021. https://doi.org/10.1136/bmj.n71
Morgan RL, Whaley P, Thayer KA, Schünemann HJ (2018) Identifying the PECO: A framework for formulating good questions to explore the association of environmental and other exposures with health outcomes, (in eng). Environ Int 121(Pt 1):1027–1031. https://doi.org/10.1016/j.envint.2018.07.015
Wells GA et al (2009) The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed 12 December 2020)
Modesti PA et al Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One vol. 11, no. 1. January 25, 2016. https://doi.org/10.1371/journal.pone.0147601
Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50(4):1088–1101
Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test, (in eng). BMJ vol. 315, no. 7109, pp. 629–634. https://doi.org/10.1136/bmj.315.7109.629
Adhikari RP, Williamson R, Sparling TM, Ferguson E, Cunningham K (2020) Parental depression and nutrition: findings from a cross-sectional household survey in Nepal. Public Health Nutr 23(16):2983–2993. https://doi.org/10.1017/S1368980020000968
Ndokera R, MacArthur C (2010) The relationship between maternal depression and adverse infant health outcomes in Zambia: a cross-sectional feasibility study. Child Care Health Dev 37(1):74–81. https://doi.org/10.1111/j.1365-2214.2010.01129.x
Nguyen PH, Friedman J, Kak M, Menon P, Alderman H (2018) Maternal depressive symptoms are negatively associated with child growth and development: evidence from rural India, (in eng). Matern Child Nutr 14(4):e12621. https://doi.org/10.1111/mcn.12621
Saeed Q, Shah N, Inam S, Shafique K (2017) Maternal depressive symptoms and child nutritional status: a cross-sectional study in socially disadvantaged Pakistani community, (in eng). J Child Health Care 21(3):331–342. https://doi.org/10.1177/1367493517721063
Reeves RV, Krause E (2019) The effects of maternal depression on early childhood development and implications for economic mobility. https://www.brookings.edu/wp-content/uploads/2019/01/ES_20190131_Reeves_Maternal_Depression2.pdf (accessed 13 Apr, 2020)
Elliott I (2016) Poverty and mental health: a review to inform the Joseph Rowntree Foundation’s Anti-Poverty Strateg. https://www.mentalhealth.org.uk/sites/default/files/Poverty%20and%20Mental%20Health.pdf (accessed 04 January, 2021)
Isaacs JB (2012) Starting school at a disadvantage: the school readiness of poor children. The Social Genome Project. https://www.brookings.edu/wp-content/uploads/2016/06/0319_school_disadvantage_isaacs.pdf (accessed 04 January, 2021)
Stewart RC (2007) Maternal depression and infant growth–a review of recent evidence. Matern Child Nutr 3(2):94–107. https://doi.org/10.1111/j.1740-8709.2007.00088.x
Center on the Developing Child at Harvard University (2009) Maternal depression can undermine the development of young children: working paper No. 8. https://46y5eh11fhgw3ve3ytpwxt9r-wpengine.netdna-ssl.com/wp-content/uploads/2009/05/Maternal-Depression-Can-Undermine-Development.pdf (accessed 05 January, 2021)
Author information
Authors and Affiliations
Contributions
Hannah Asare conceived the work, performed the paper selection and risk of bias assessment and wrote the first version of the manuscript. Hannah Asare with the help of Cristian Ricci performed the qualitative synthesis and statistical analyses. Alice Rosi defined the detailed literature search strategy and performed the search strings. Alice Rosi, Francesca Scazzina, Mieke Faber, Marius Smuts and Cristian Ricci revised the manuscript. Mieke Faber, Marius Smuts and Cristian Ricci supervised the research team. All the authors actively contributed to the writing of the manuscript and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The ethics committee of the North-West University (NWU-00282–21-A1) approved this study.
Competing interests
The authors declare no competing interests.
Consent to participate
N/A.
Consent for publication
N/A.
Additional information
Communicated by Gregorio Paolo Milani
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Asare, H., Rosi, A., Scazzina, F. et al. Maternal postpartum depression in relation to child undernutrition in low- and middle-income countries: a systematic review and meta-analysis. Eur J Pediatr 181, 979–989 (2022). https://doi.org/10.1007/s00431-021-04289-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-021-04289-4