Abstract
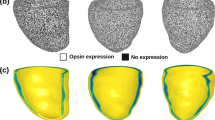
A major challenge in cardiac optogenetics is to have minimally invasive large volume excitation and suppression for effective cardioversion and treatment of tachycardia. It is important to study the effect of light attenuation on the electrical activity of cells in in vivo cardiac optogenetic experiments. In this computational study, we present a detailed analysis of the effect of light attenuation in different channelrhodopsins (ChRs)-expressing human ventricular cardiomyocytes. The study shows that sustained illumination from the myocardium surface used for suppression, simultaneously results in spurious excitation in deeper tissue regions. Tissue depths of suppressed and excited regions have been determined for different opsin expression levels. It is shown that increasing the expression level by 5-fold enhances the depth of suppressed tissue from 2.24 to 3.73 mm with ChR2(H134R) (ChR2 with a single point mutation at position H134), 3.78 to 5.12 mm with GtACR1 (anion-conducting ChR from cryptophyte algae Guillardia theta) and 6.63 to 9.31 mm with ChRmine (a marine opsin gene from Tiarina fusus). Light attenuation also results in desynchrony in action potentials in different tissue regions under pulsed illumination. It is further shown that gradient-opsin expression not only enables suppression up to the same level of tissue depth but also enables synchronized excitation under pulsed illumination. The study is important for the effective treatment of tachycardia and cardiac pacing and for extending the scale of cardiac optogenetics.







Similar content being viewed by others
Data availability
All data are presented in the manuscript and figures.
References
Entcheva E, Kay MW (2021) Cardiac optogenetics: a decade of enlightenment. Nat Rev Cardiol 18:349–367
Williams JC, Entcheva E (2015) Optogenetic versus electrical stimulation of human cardiomyocytes: modeling insights. Biophys J 108:1934–1945
Bruegmann T, Malan D, Hesse M, Beiert T, Fuegemann CJ, Fleischmann BK, Sasse P (2010) Optogenetic control of heart muscle in vitro and in vivo. Nat Methods 7:897–900
Bruegmann T, Boyle PM, Vogt CC, Karathanos TV, Arevalo HJ, Fleischmann BK, Trayanova NA, Sasse P (2016) Optogenetic defibrillation terminates ventricular arrhythmia in mouse hearts and human simulations. J Clin Investing 126:3894–3904
Floria M, Radu S, Gosav EM, Moraru AC, Serban T, Carauleanu A, Costea CF, Ouatu A, Ciocoiu M, Tanase DM (2020) Cardiac optogenetics in atrial fibrillation: current challenges and future opportunities. BioMed Res Int 8814092. https://doi.org/10.1155/2020/8814092
Nyns ECA, Kip A, Bart CI, Plomp JJ, Zeppenfeld K, Schalij MJ, de Vries AAF, Pijnappels DA (2017) Optogenetic termination of ventricular arrhythmias in the whole heart: towards biological cardiac rhythm management. Eur Heart J 38:2132–2136
O’shea C, Holmes AP, Winter J, Correia J, Ou X, Dong R, He S, Kirchhof P, Fabritz L, Rajpoot K, Pavlovic D (2019) Cardiac optogenetics and optical mapping–overcoming spectral congestion in all-optical cardiac electrophysiology. Front Physiol 10:182. https://doi.org/10.3389/fphys.2019.00182
Hussaini S, Venkatesan V, Biasci V, Romero Sepúlveda JM, Quiñonez Uribe RA, Sacconi L, Bub G, Richter C, Krinski V, Parlitz U, Majumder R (2021) Drift and termination of spiral waves in optogenetically modified cardiac tissue at sub-threshold illumination. Elife 10:e59954
Deisseroth K (2015) Optogenetics: 10 years of microbial opsins in neuroscience. Nat Neurosci 18:1213–1225
Pyari G, Bansal H, Roy S (2022) Ultra-low power deep sustained optogenetic excitation of human ventricular cardiomyocytes with red-shifted opsins: a computational study. J Physiol 600:4653–4676
Jia Z, Valiunas V, Lu Z, Bien H, Liu H, Wang HZ, Rosati B, Brink PR, Cohen IS, Entcheva E (2011) Stimulating cardiac muscle by light: cardiac optogenetics by cell delivery. Cir Arrhythm Electrophysiol 4:753–760
Emiliani V, Entcheva E, Hedrich R, Hegemann P, Konrad KR, Lüscher C, Mahn M, Pan ZH, Sims RR, Vierock J, Yizhar O (2022) Optogenetics for light control of biological systems. Nat Rev Methods Primers 2:1–25
Sung YL, Wang TW, Lin TT, Lin SF (2022) Optogenetics in cardiology: methodology and future applications. Int J Arrhythm 23:9
Gruber A, Edri O, Huber I, Arbel G, Gepstein A, Shiti A, Shaheen N, Chorna S, Landesberg M, Gepstein L (2021) Optogenetic modulation of cardiac action potential properties may prevent arrhythmogenesis in short and long QT syndromes. JCI Insight 6:e147470. https://doi.org/10.1172/jci.insight.147470
Entcheva E, Williams JC (2014) Channelrhodopsin2 current during the action potential: “optical AP clamp” and approximation. Sci Rep 4:1–7
Kopton RA, Baillie JS, Rafferty SA, Moss R, Zgierski-Johnston CM, Prykhozhij SV, Stoyek MR, Smith FM, Kohl P, Quinn TA, Schneider-Warme F (2018) Cardiac electrophysiological effects of light-activated chloride channels. Front Physiol 9:1806
Govorunova EG, Sineshchekov OA, Janz R, Liu X, Spudich JL (2015) Natural light-gated anion channels: a family of microbial rhodopsins for advanced optogenetics. Science 349:647–650
Arrenberg AB, Stainier DY, Baier H, Huisken J (2010) Optogenetic control of cardiac function. Science 330:971–974
Govorunova EG, Cunha SR, Sineshchekov OA, Spudich JL (2016) Anion channelrhodopsins for inhibitory cardiac optogenetics. Sci Rep 6:33530
Ferenczi EA, Tan X, Huang CL (2019) Principles of optogenetic methods and their application to cardiac experimental systems. Front Physiol 10:1096
Marshel JH, Kim YS, Machado TA, Quirin S, Benson B, Kadmon J, Raja C, Chibukhchyan A, Ramakrishnan C, Inoue M, Shane JC, McKnight DJ, Yoshizawa S, Kato HE, Ganguli S, Deisseroth K (2019) Cortical layer-specific critical dynamics triggering perception. Science 365:eaaw5202
Karathanos TV, Bayer JD, Wang D, Boyle PM, Trayanova NA (2016) Opsin spectral sensitivity determines the effectiveness of optogenetic termination of ventricular fibrillation in the human heart: a simulation study. J Physiol 594:6879–6891
Al-Juboori SI, Dondzillo A, Stubblefield EA, Felsen G, Lei TC, Klug A (2013) Light scattering properties vary across different regions of the adult mouse brain. PLoS One 8:e67626
Roy S, Tewari R, Thyagarajan K (1991) Accurate empirical relations for characterizing a single-mode matched clad fibre from its far-field pattern. J Opt Commun 12:26–29
Bingen BO, Engels MC, Schalij MJ, Jangsangthong W, Neshati Z, Feola I, Ypey DL, Askar SF, Panfilov AV, Pijnappels DA, de Vries AA (2014) Light-induced termination of spiral wave arrhythmias by optogenetic engineering of atrial cardiomyocytes. Cardiovasc Res 104:194–205
Nussinovitch U, Gepstein L (2015) Optogenetics for in vivo cardiac pacing and resynchronization therapies. Nat Biotechnol 33:750–754
Chien KR (2008) Regenerative medicine and human models of human disease. Nature 453:302–305
Izadi I, Dusend V, Takrouni A, Nudds N, Gradkowski K, O’Brien P, Sasse P, Corbett B (2021) Wide area uniform illumination scheme using LED matrix for optogenetic cardiac pacing. Photonics 8:499
Dufour S, De Koninck Y (2015) Optrodes for combined optogenetics and electrophysiology in live animals. Neurophoton 2(3):031205
Cardin JA, Carlén M, Meletis K, Knoblich U, Zhang F, Deisseroth K, Tsai LH, Moore CI (2010) Targeted optogenetic stimulation and recording of neurons in vivo using cell-type-specific expression of channelrhodopsin-2. Nat Protocols 5(2):247–254
Chen R, Gore F, Nguyen QA, Ramakrishnan C, Patel S, Kim SH, Raffiee M, Kim YS, Hsueh B, Krook-Magnusson E, Soltesz I (2021) Deep brain optogenetics without intracranial surgery. Nat Biotechnol 39(2):161–164
Hsueh B, Chen R, Jo Y, Tang D, Raffiee M, Kim YS, Inoue M, Randles S, Ramakrishnan C, Patel S, Kim DK (2023) Cardiogenic control of affective behavioural state. Nature 615:292–299
Bansal H, Pyari G, Roy S (2023) Optogenetic generation of neural firing patterns with temporal shaping of light pulses. Photonics 10(5):571
Abilez OJ, Wong J, Prakash R, Deisseroth K, Zarins CK, Kuhl E (2011) Multiscale computational models for optogenetic control of cardiac function. Biophys J 101:1326–1334
Williams JC, Xu J, Lu Z, Klimas A, Chen X, Ambrosi CM, Cohen IS, Entcheva E (2013) Computational optogenetics: empirically-derived voltage- and light-sensitive channelrhodopsin-2 model. PLoS Comput Biol 9:e1003220
Bansal H, Gupta N, Roy S (2020a) Comparison of low-power, high-frequency and temporally precise optogenetic inhibition of spiking in NpHR, eNpHR3. 0 and Jaws-expressing neurons. Biomed Phys Eng Express 6:045011
Bansal H, Gupta N, Roy S (2020b) Theoretical analysis of low-power bidirectional optogenetic control of high-frequency neural codes with single spike resolution. Neuroscience 449:165–188
Bansal H, Gupta N, Roy S (2021) Theoretical analysis of optogenetic spiking with ChRmine, bReaChES and CsChrimson-expressing neurons for retinal prostheses. J Neural Eng 18:0460b8
Bansal H, Pyari G, Roy S (2022) Co-expressing fast channelrhodopsin with step-function opsin overcomes spike failure due to photocurrent desensitization in optogenetics: a theoretical study. J Neural Eng 19:026032
Saran S, Gupta N, Roy S (2018) Theoretical analysis of low-power fast optogenetic control of firing of Chronos-expressing neurons. Neurophoton 5:025009
Gupta N, Bansal H, Roy S (2019) Theoretical optimization of high-frequency optogenetic spiking of red-shifted very fast-Chrimson-expressing neurons. Neurophoton 6:025002
Bruegmann T, Beiert T, Vogt CC, Schrickel JW, Sasse P (2018) Optogenetic termination of atrial fibrillation in mice. Cardiovasc Res 114:713–723
Ochs AR, Karathanos TV, Trayanova NA, Boyle PM (2021) Optogenetic stimulation using anion channelrhodopsin (GtACR1) facilitates termination of reentrant arrhythmias with low light energy requirements: a computational study. Front Physiol 12:718622
Boyle PM, Williams JC, Ambrosi CM, Entcheva E, Trayanova NA (2013) A comprehensive multiscale framework for simulating optogenetics in the heart. Nat Commun 4:2370
Klimas A, Entcheva E (2014) Toward microendoscopyinspired cardiac optogenetics in vivo: technical overview and perspective. J Biomed Opt 19:080701
Roy S, Singh CP, Reddy KP (2001) Generalized model for all-optical light modulation in bacteriorhodopsin. J Appl Phys 90:3679–3688
Roy S, Kikukawa T, Sharma P, Kamo N (2006) All-optical switching in pharaonis phoborhodopsin protein molecules. IEEE Trans Nanobiosci 5:178–187
Roy S, Yadav C (2014) All-optical sub-ps switching and parallel logic gates with bacteriorhodopsin (BR) protein and BR-gold nanoparticles. Laser Phys Lett 11:12590
Engelhard C, Chizhov I, Siebert F, Engelhard M (2018) Microbial halorhodopsins: light-driven chloride pumps. Chem Rev 118:10629–10645
Evans BD, Jarvis S, Schultz SR, Nikolic K (2016) PyRhO: a multiscale optogenetics simulation platform. Front Neuroinform 10:8
ten Tusscher KH, Noble D, Noble PJ, Panfilov AV (2014) A model for human ventricular tissue. Am J Physiol Heart Circ Physiol 286:H1573–H1589
ten Tusscher KH, Panfilov AV (2006) Alternans and spiral breakup in a human ventricular tissue model. Am J Physiol Heart Circ Physiol 291:1088–1100
Foutz TJ, Arlow RL, McIntyre CC (2012) Theoretical principles underlying optical stimulation of a channelrhodopsin-2 positive pyramidal neuron. J Neurophysiol 107:3235–3245
Swartling J, Pålsson S, Platonov P, Olsson SB, Andersson-Engels S (2003) Changes in tissue optical properties due to radio-frequency ablation of myocardium. Med Bio Eng Comput 41:403–409. https://doi.org/10.1007/BF02348082
Aravanis AM, Wang LP, Zhang F, Meltzer LA, Mogri MZ, Schneider MB, Deisseroth K (2007) An optical neural interface: in vivo control of rodent motor cortex with integrated fiberoptic and optogenetic technolog. J Neural Eng 4:S143–S156
Kubelka P, Munk F (1931) Ein Beitrag zur Optik der Farbanstriche. Zeitschrift für Technische Physik 12:593–601
Vo-Dinh T (2003) Biomedical photonics handbook. CRC Press. https://doi.org/10.1201/9780203008997
Nyns ECA, Jin T, Fontes MS, van den Heuvel T, Portero V, Ramsey C, Bart CI, Zeppenfeld K, Schalij MJ, van Brakel TJ, Ramkisoensing AA (2014) Optical ventricular cardioversion by local optogenetic targeting and LED implantation in a cardiomyopathic rat model. Cardiovasc Res 118:2293–2303
Yu J, Chen K, Lucero RV, Ambrosi CM, Entcheva E (2015) Cardiac optogenetics: enhancement by all-trans-retinal. Sci Rep 5:1–2
Alex A, Li A, Tanzi RE, Zhou C (2015) Optogenetic pacing in Drosophila melanogaster. Sci Adv 1:e1500639
Govorunova EG, Gou Y, Sineshchekov OA, Li H, Lu X, Wang Y, Brown LS, St-Pierre F, Xue M, Spudich JL (2022) Kalium channelrhodopsins are natural light-gated potassium channels that mediate optogenetic inhibition. Nat Neurosci 25:967–974
Vierock J, Peter E, Grimm C, Rozenberg A, Chen IW, Tillert L, Castro Scalise AG, Casini M, Augustin S, Tanese D, Forget BC, Peyronnet R, Schneider-Warme F, Emiliani V, Hegemann P (2022) WiChR, a highly potassium selective channelrhodopsin for low-light one- and two-photon inhibition of excitable cells. Sci Adv 8:eadd7729. https://doi.org/10.1126/sciadv.add7729
Ausra J, Madrid M, Yin RT, Hanna J, Arnott S, Brennan JA, Peralta R, Clausen D, Bakall JA, Efimov IR, Gutruf P (2022) Wireless, fully implantable cardiac stimulation and recording with on-device computation for closed-loop pacing and defibrillation. Sci Adv 8:eabq7469
Biasci V, Santini L, Marchal GA, Hussaini S, Ferrantini C, Coppini R, Loew LM, Luther S, Campione M, Poggesi C, Pavone FS, Cerbai E, Bub G, Sacconi L (2022) Optogenetic manipulation of cardiac electrical dynamics using sub-threshold illumination: dissecting the role of cardiac alternans in terminating rapid rhythms. Basic Res Cardiol 117:25
Kuhne J, Vierock J, Tennigkeit SA, Dreier MA, Wietek J, Petersen D, Gavriljuk K, El-Mashtoly SF, Hegemann P, Gerwert K (2019) Unifying photocycle model for light adaptation and temporal evolution of cation conductance in channelrhodopsin-2. Proc Natl Acad Sci USA 116:9380–9389
Sahel JA, Boulanger-Scemama E, Pagot C, Arleo A, Galluppi F, Martel JN, Esposti SD, Delaux A, de Saint Aubert JB, de Montleau C, Gutman E (2021) Partial recovery of visual function in a blind patient after optogenetic therapy. Nat Med 27:1223–1229
Vogt CC, Bruegmann T, Malan D, Ottersbach A, Roell W, Fleischmann BK, Sasse P (2015) Systemic gene transfer enables optogenetic pacing of mouse hearts. Cardiovasc Res 106:338–343
Acknowledgements
The authors are grateful to Rev. Prof. Prem Saran Satsangi for his kind inspiration and encouragement. The authors gratefully acknowledge the University Grants Commission, India, for the Special Assistance Programme Grant No. (F.530/14/DRS-III/2015(SAP-I)) and Department of Science and Technology, India, for the award of Junior Research Fellowship to G. P., the INSPIRE Fellowship (DST/INSPIRE/03/2017/003087) to H. B. and research projects CRG/2021/005139 and MTR/2021/000742 to S. R.
Funding
This work was supported by the University Grants Commission, India (F.530/14/DRS-III/2015(SAP-I)) and the Department of Science and Technology, India (CRG/2021/005139 and MTR/2021/000742 to S. R. and DST/INSPIRE/03/2017/003087 to H. B.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the special issue on Next generation optogenetics in Pflügers Archiv—European Journal of Physiology
This article is published as part of the Special Issue on Next-generation Optogenetics.
Appendix
Appendix
Appendix A Four-state model of opsin photocurrent
On illumination, the opsin molecule switches from the closed ground state-C1 to open state-O1. From O1, the molecule either decays back to C1 or transits to the second open state-O2, which is less conductive in comparison to O1 but has a longer lifetime. The reversible transition between O1 and O2 can be both light and thermal induced. The molecule in O2 state can also transit to second closed-state C2. From C2, the molecule thermally relaxes to the ground state C1 or can be photo-excited back to O2. The transition from C2 to C1, also called the recovery process of ChRs, is the slowest process in the photocycle [38,39,40,41, 50]. Recent experimental results have shown that ChRmine exhibits the fastest recovery kinetics [21].
If C1, O1, O2, and C2 denote the instantaneous fraction of opsin molecules in each of the four states and follow the constraint C1 + O1 + O2 + C2 = 1, the time-dependent transitions among these states can be defined by the following set of rate equations,
The transitions C1 → O1, C2 → O2, O1 → C1, O2 → C2, O1 → O2, O2 → O1, and C2 → C1,respectively, are governed by the rate constants Ga1, Ga2, Gd1, Gd2, Gf, Gb, and Gr, respectively. Among these rate constants, the light-dependent rate constants vary as \({G}_{a1}\left(\phi \right)=\upvarepsilon {k}_1{\phi}^p/\left({\phi}^p+{\phi}_m^p\right)\), Ga2(ϕ) \(=\upvarepsilon {k}_2{\phi}^p/\left({\phi}^p+{\upphi}_m^p\right)\), Gf(ϕ) \(={G}_{f0}+\upvarepsilon {k}_f{\phi}^q/\left({\phi}^q+{\phi}_m^q\right)\) and Gb(ϕ) \(={G}_{b0}+{\upvarepsilon k}_b{\phi}^q/\left({\phi}^q+{\phi}_m^q\right)\), where ɛ is a wavelength-dependent parameter. Since there are two open states, fϕ(ϕ, t) = O1 + γO2 where γ = gO2/gO1. gO1 and gO2 are the conductances of states O1 and O2, respectively.
Appendix B Ionic currents through natural ion channels and pumps in human ventricular cardiomyocytes
The ionic currents namely, INa, Ito, IKr, ICaL, and IKs can be expressed as \({I}_f=\kern0.5em {g}_f{m}_1^p{m}_2^q{m}_3^r{m}_4^s\left(V-{E}_f\right)\), where gf and Ef denote the maximal conductance and reversal potential of each ion channel, and m1, m2, m3, and m4 are different gating variables (with exponent p, q, r, and s, respectively) (Tables 2 and 3). Other ionic currents are expressed as follows:
where the Nernst equation has been used to model the variable reversal potential for each ion channel that includes ENa, EK, ECa, and EKs as,
where [Na+]i, [Ca2+]i, and [K+]i are intracellular ion-concentrations, which have been initially considered [Na+]i = 7.67 mM, [Ca2+]i = 0.00007 mM and [K+]i = 138.3 mM and z = 1 for Na+and K+, z = 2 for Ca2+ [51, 52].
The rate of change of in [Na+]i, [Ca2+]i and [K+]i can be expressed as,
where Caitotal is total cytoplasmic Ca2+ concentration, CaSRtotal is total sarcoplasmic reticulum Ca2+ concentration, CaSStotal is total diadic subspace Ca2+ concentration, Cai is free cytoplasmic Ca2+ concentration, CaSR is free sarcoplasmic reticulum Ca2+ concentration, Cass is free diadic subspace Ca2+ concentration, Irel is calcium-induced calcium release current, Iup is sarcoplasmic reticulum Ca2+ pump current, Ileak is sarcoplasmic reticulum Ca2+ leak current, Ixfer is diffusive Ca2+ current between diadic Ca2+ subspace and bulk cytoplasm, and O and \(\overline{R}\) are proportion of open and closed Irel channels, respectively [51, 52]. Each gating function x (m1, m2, m3, and m4) obeys the first-order kinetics as \(\dot{x}=\left({x}_{\infty }-x\right)/{\tau}_x\). The voltage-dependent functions (x∞and τx) and values of parameters are given in Tables 2 and 3, respectively [51, 52].
Appendix C Geometrical spreading, Gaussian distribution, absorption, and scattering of light under fiber optic illumination
Light emitted from the optical fiber spreads as a cone of light with a divergence half angle (θdiv) which depends on the NA and the refractive index of the tissue (ntissue) as follows,
The radius of the light cone (R) at tissue depth z from the optical fiber with radius R0 spreads as,
For myocardium, ntisssue = 1.4. Here, R0 is considered to be 0.2 mm, and NA is considered within the range 0.1–0.4, as used in most of the optogenetics experiments [53, 54].
If I is the irradiance at a distance z from the optical fiber, the radiant power (P) at each point in space, when independently considering geometrical effects, is defined as,
Therefore, the transmittance due to geometrical spreading is defined as follows,
The Gaussian distribution of light G(r, z) emitted by an optical fiber can be approximated as,
The Kubelka-Munk general theory of light propagation in diffuse scattering media has been used to capture the effect of scattering and absorption [55, 56]. The transmittance of light through the myocardium tissue is given by,
where a = 1 + K/S, \(b=\sqrt{a^2}-1\). This study assumes that the myocardium tissue is optically homogeneous and illuminated normally from its surface with monochromatic light. The absorption and scattering coefficients are wavelength dependent.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Pyari, G., Bansal, H. & Roy, S. Optogenetically mediated large volume suppression and synchronized excitation of human ventricular cardiomyocytes. Pflugers Arch - Eur J Physiol 475, 1479–1503 (2023). https://doi.org/10.1007/s00424-023-02831-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00424-023-02831-x