Abstract
Background
Secondary achalasia or pseudoachalasia is a clinical presentation undistinguishable from achalasia in terms of symptoms, manometric, and radiographic findings, but associated with different and identifiable underlying causes.
Methods
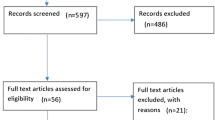
A literature review was conducted on the PubMed database restricting results to the English language. Key terms used were “achalasia-like” with 63 results, “secondary achalasia” with 69 results, and “pseudoachalasia” with 141 results. References of the retrieved papers were also manually reviewed.
Results
Etiology, diagnosis, and treatment were reviewed.
Conclusions
Pseudoachalasia is a rare disease. Most available evidence regarding this condition is based on case reports or small retrospective series. There are different causes but all culminating in outflow obstruction. Clinical presentation and image and functional tests overlap with primary achalasia or are inaccurate, thus the identification of secondary achalasia can be delayed. Inadequate diagnosis leads to futile therapies and could worsen prognosis, especially in neoplastic disease. Routine screening is not justifiable; good clinical judgment still remains the best tool. Therapy should be aimed at etiology. Even though Heller’s myotomy brings the best results in non-malignant cases, good clinical judgment still remains the best tool as well.

Similar content being viewed by others
Data availability
No datasets were generated or analysed during the current study.
References
Lendrum FC (1937) Anatomic features of the cardiac orifice of the stomach with special reference to cardiospasm. Arch Intern Med 59:474–451
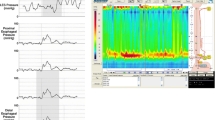
Yadlapati R, Kahrilas PJ, Fox MR et al (2021) Esophageal motility disorders on high-resolution manometry: Chicago classification version 4.0©. Neurogastroenterol Motil. 33(1):e14058. https://doi.org/10.1111/nmo.14058. (Erratum in: Neurogastroenterol Motil. 2022 5;:e14179)
Kahrilas PJ, Boeckxstaens G (2013) The spectrum of achalasia: lessons from studies of pathophysiology and high-resolution manometry. Gastroenterology 145:954–965
Ravi K, Sweetser S, Katzka DA (2016) Pseudoachalasia secondary to bariatric surgery. Dis Esophagus 29(8):992–995
Ogilvie H (1947) The early diagnosis of cancer of the oesophagus and stomach. Br Med J 2(4523):405–407. https://doi.org/10.1136/bmj.2.4523.405
Hejazi RA, Zhang D, McCallum RW (2009) Gastroparesis, pseudoachalasia and impaired intestinal motility as paraneoplastic manifestations of small cell lung cancer. Am J Med Sci 338(1):69–71. https://doi.org/10.1097/MAJ.0b013e31819b93e5
Song CW, Chun HJ, Kim CD, Ryu HS, Hyun JH, Kahrilas PJ (1999) Association of pseudoachalasia with advancing cancer of the gastric cardia. Gastrointest Endosc 50(4):486–491. https://doi.org/10.1016/s0016-5107(99)70070-2
Parkman HP, Cohen S (1993) Malignancy-induced secondary achalasia. Dysphagia. 8(3):292–6 (Corrected and republished in: Dysphagia. 1994 9(2):292-6)
Moonka R, Pellegrini CA (1999) Malignant pseudoachalasia. Surg Endosc 13(3):273–275. https://doi.org/10.1007/s004649900962
Wehrli NE, Levine MS, Rubesin SE, Katzka DA, Laufer I (2007) Secondary achalasia and other esophageal motility disorders after laparoscopic Nissen fundoplication for gastroesophageal reflux disease. AJR Am J Roentgenol 189(6):1464–1468. https://doi.org/10.2214/AJR.07.2582
Casas MA, Schlottmann F, Herbella FAM, Buxhoeveden R, Patti MG (2019) Esophageal achalasia after Roux-en-Y gastric bypass for morbid obesity. Updates Surg 71(4):631–635. https://doi.org/10.1007/s13304-019-00688-3
Abu Ghanimeh M, Qasrawi A, Abughanimeh O, Albadarin S, Clarkston W (2017) Achalasia after bariatric Roux-en-Y gastric bypass surgery reversal. World J Gastroenterol 23(37):6902–6906. https://doi.org/10.3748/wjg.v23.i37.6902
Suris X, Moyà F, Panés J, del Olmo JA, Solé M, Muñoz-Gómez J (1993) Achalasia of the esophagus in secondary amyloidosis. Am J Gastroenterol 88(11):1959–1960
Haj Ali SN, Nguyen NQ, Abu Sneineh AT (2021) Pseudoachalasia: a diagnostic challenge. When to consider and how to manage? Scand J Gastroenterol. 56(7):747–752. https://doi.org/10.1080/00365521.2021.1925957
Schizas D, Theochari NA, Katsaros I, Mylonas KS, Triantafyllou T, Michalinos A, Kamberoglou D, Tsekrekos A, Rouvelas I (2020) Pseudoachalasia: a systematic review of the literature. Esophagus 17(3):216–222. https://doi.org/10.1007/s10388-020-00720-1
Campo SM, Zullo A, Scandavini CM, Frezza B, Cerro P, Balducci G (2013) Pseudoachalasia: a peculiar case report and review of the literature. World J Gastrointest Endosc 5(9):450–454. https://doi.org/10.4253/wjge.v5.i9.450
Ponds FA, van Raath MI, Mohamed SMM, Smout AJPM, Bredenoord AJ (2017) Diagnostic features of malignancy-associated pseudoachalasia. Aliment Pharmacol Ther 45(11):1449–1458. https://doi.org/10.1111/apt.14057
Katzka DA, Farrugia G, Arora AS (2012) Achalasia secondary to neoplasia: a disease with a changing differential diagnosis. Dis Esophagus 25:331–336
Fredens K, Tøttrup A, Kristensen IB, Dahl R, Jacobsen NO, Funch-Jensen P, Thommesen P (1989) Severe destruction of esophageal nerves in a patient with achalasia secondary to gastric cancer. A possible role of eosinophil neurotoxic proteins. Dig Dis Sci. 34(2):297–303. https://doi.org/10.1007/BF01536066
Lee HR, Lennon VA, Camilleri M, Prather CM (2001) Paraneoplastic gastrointestinal motor dysfunction: clinical and laboratory characteristics. Am J Gastroenterol 96(2):373–379. https://doi.org/10.1111/j.1572-0241.2001.03454.x
Fabian E, Eherer AJ, Lackner C, Urban C, Smolle-Juettner FM, Krejs GJ (2019) Pseudoachalasia as first manifestation of a malignancy. Dig Dis 37(5):347–354. https://doi.org/10.1159/000495758
Lennon VA, Sas DF, Busk MF, Scheithauer B, Malagelada JR, Camilleri M, Miller LJ (1991) Enteric neuronal autoantibodies in pseudoobstruction with small-cell lung carcinoma. Gastroenterology 100(1):137–142. https://doi.org/10.1016/0016-5085(91)90593-a
Poulin EC, Diamant NE, Kortan P, Seshadri PA, Schlachta CM, Mamazza J (2000) Achalasia developing years after surgery for reflux disease: case reports, laparoscopic treatment, and review of achalasia syndromes following antireflux surgery. J Gastrointest Surg 4(6):626–631. https://doi.org/10.1016/s1091-255x(00)80113-4
Stylopoulos N, Bunker CJ, Rattner DW (2002) Development of achalasia secondary to laparoscopic Nissen fundoplication. J Gastrointest Surg 6:368–378. https://doi.org/10.1016/S1091-255X(02)00019-7
Awad ZT, Selima MA, Filipi CJ (2002) Pseudoachalasia as a late complication of gastric wrap performed for morbid obesity: report of a case. Surg Today 32(10):906–909. https://doi.org/10.1007/s005950200178
Myers JC, Jamieson GG, Wayman J, King DR, Watson DI (2007) Esophageal ileus following laparoscopic fundoplication. Dis Esophagus 20(5):420–427. https://doi.org/10.1111/j.1442-2050.2007.00643.x
Schwameis K, Ayazi S, Zaidi AH, Hoppo T, Jobe BA (2020) Development of pseudoachalasia following magnetic sphincter augmentation (MSA) with restoration of peristalsis after endoscopic dilation. Clin J Gastroenterol 13(5):697–702. https://doi.org/10.1007/s12328-020-01140-5
Arias IE, Radulescu M, Stiegeler R et al (2009) Diagnosis and treatment of megaesophagus after adjustable gastric banding for morbid obesity. Surg Obes Relat Dis 5(2):156–159. https://doi.org/10.1016/j.soard.2008.11.007
Losh JM, Sanchez B, Waxman K (2017) Refractory pseudoachalasia secondary to laparoscopically placed adjustable gastric band successfully treated with Heller myotomy. Surg Obes Relat Dis 13(2):e4–e8. https://doi.org/10.1016/j.soard.2016.10.005
Khan A, Ren-Fielding C, Traube M (2011) Potentially reversible pseudoachalasia after laparoscopic adjustable gastric banding. J Clin Gastroenterol 45(9):775–779
Facchiano E, Scaringi S, Sabate JM et al (2007) Is esophageal dysmotility after laparoscopic adjustable gastric banding reversible? Obes Surg 17(6):832–835
Wiesner W, Hauser M, Schöb O, Weber M, Hauser RS (2001) Pseudo-achalasia following laparoscopically placed adjustable gastric banding. Obes Surg 11(4):513–518. https://doi.org/10.1381/096089201321209440
Robert M, Golse N, Espalieu P et al (2012) Achalasia-like disorder after laparoscopic adjustable gastric banding: a reversible side effect? Obes Surg 22(5):704–711
Naef M, Mouton WG, Naef U, van der Weg B, Maddern GJ, Wagner HE (2011) Esophageal dysmotility disorders after laparoscopic gastric banding–an underestimated complication. Ann Surg 253(2):285–290. https://doi.org/10.1097/SLA.0b013e318206843e
Lipka S, Katz S (2013) Reversible pseudoachalasia in a patient with laparoscopic adjustable gastric banding. Gastroenterol Hepatol (N Y) 9(7):469–471
Herbella FAM, Patti MG (2021) The Impact of bariatric procedures on esophageal motility. Foregut 1(3):268–276. https://doi.org/10.1177/26345161211043462
Campos GM, Mazzini GS, Altieri MS, Docimo S Jr, DeMaria EJ, Rogers AM (2021) Clinical Issues Committee of the American Society for metabolic and bariatric surgery. ASMBS position statement on the rationale for performance of upper gastrointestinal endoscopy before and after metabolic and bariatric surgery. Surg Obes Relat Dis. 17(5):837–847. https://doi.org/10.1016/j.soard.2021.03.007
Lemme EMO, Alvariz AC, Pereira GLC (2021) Esophageal functional disorders in the pre-operatory evaluation of bariatric surgery. Arq Gastroenterol. 58(2):190–194. https://doi.org/10.1590/S0004-2803.202100000-34
Jaffin BW, Knoepflmacher P, Greenstein R (1999) High prevalence of asymptomatic esophageal motility disorders among morbidly obese patients. Obes Surg 9(4):390–395. https://doi.org/10.1381/096089299765552990
Chuah SK, Kuo CM, Wu KL, Changchien CS, Hu TH, Wang CC, Chiu YC, Chou YP, Hsu PI, Chiu KW, Kuo CH, Chiou SS, Lee CM (2006) Pseudoachalasia in a patient after truncal vagotomy surgery successfully treated by subsequent pneumatic dilations. World J Gastroenterol. 12(31):5087–90. https://doi.org/10.3748/wjg.v12.i31.5087
Sharp JR (1979) Mechanical and neurogenic factors in postvagotomy dysphagia. J Clin Gastroenterol 1(4):321–324. https://doi.org/10.1097/00004836-197912000-00008
Gelfand MD (1981) Irreversible esophageal motor dysfunction in postvagotomy dysphagia. Am J Gastroenterol 76(4):347–350
Duntemann TJ, Dresner DM (1995) Achalasia-like syndrome presenting after highly selective vagotomy. Dig Dis Sci 40(9):2081–2083. https://doi.org/10.1007/BF02208682
Singhal S, Kirkpatrick DR, Masuda T, Gerhardt J, Mittal SK (2018) Primary and redo antireflux surgery: outcomes and lessons learned. J Gastrointest Surg 22(2):177–186. https://doi.org/10.1007/s11605-017-3480-4
Trus TL, Bax T, Richardson WS, Branum GD, Mauren SJ, Swanstrom LL, Hunter JG (1997) Complications of laparoscopic paraesophageal hernia repair. J Gastrointest Surg. 1(3):221–7; discussion 228. https://doi.org/10.1016/s1091-255x(97)80113-8
Little AG, Correnti FS, Calleja IJ, Montag AG, Chow YC, Ferguson MK, Skinner DB (1986) Effect of incomplete obstruction on feline esophageal function with a clinical correlation. Surgery 100(2):430–436
Schneider JH, Peters JH, Kirkman E, Bremner CG, DeMeester TR (1999) Are the motility abnormalities of achalasia reversible? An experimental outflow obstruction in the feline model. Surgery 125(5):498–503
McKellar SH, Allen MS, Cassivi SD, Nichols FC 3rd, Shen KR, Wigle DA, Deschamps C (2011) Laparoscopic conversion from Nissen to partial fundoplication for refractory dysphagia. Ann Thorac Surg 91(3):932–934. https://doi.org/10.1016/j.athoracsur.2010.07.090
Galey KM, Wilshire CL, Niebisch S, Jones CE, Raymond DP, Litle VR, Watson TJ, Peters JH (2011) Atypical variants of classic achalasia are common and currently under-recognized: a study of prevalence and clinical features. J Am Coll Surg. 213(1):155–61; discussion 162-3. https://doi.org/10.1016/j.jamcollsurg.2011.02.008
Bredenoord AJ, Babaei A, Carlson D, Omari T, Akiyama J, Yadlapati R, Pandolfino JE, Richter J, Fass R (2021) Esophagogastric junction outflow obstruction. Neurogastroenterol Motil 33(9):e14193. https://doi.org/10.1111/nmo.14193
Fontes LH, Herbella FA, Rodriguez TN, Trivino T, Farah JF (2013) Progression of diffuse esophageal spasm to achalasia: incidence and predictive factors. Dis Esophagus 26(5):470–474. https://doi.org/10.1111/j.1442-2050.2012.01377.x
Dejaeger M, Lormans M, Dejaeger E, Fagard K (2020) Case report: an aortic aneurysm as cause of pseudoachalasia. BMC Gastroenterol. 20(1):63. https://doi.org/10.1186/s12876-020-01198-y
Fisichella PM, Raz D, Palazzo F, Niponmick I, Patti MG (2008) Clinical, radiological, and manometric profile in 145 patients with untreated achalasia. World J Surg 32(9):1974–1979. https://doi.org/10.1007/s00268-008-9656-z
Floch NR, Hinder RA, Klingler PJ, Branton SA, Seelig MH, Bammer T, Filipi CJ (1999) Is laparoscopic reoperation for failed antireflux surgery feasible? Arch Surg 134(7):733–737. https://doi.org/10.1001/archsurg.134.7.733
Gergely M, Mello MD, Rengarajan A, Gyawali CP (2021) Duration of symptoms and manometric parameters offer clues to diagnosis of pseudoachalasia. Neurogastroenterol Motil 33(1):e13965. https://doi.org/10.1111/nmo.13965
Sutton RA, Gabbard SL (2017) High-resolution esophageal manometry findings in malignant pseudoachalasia. Dis Esophagus. 30(12):1–3. https://doi.org/10.1093/dote/dox095
Gupta P, Debi U, Sinha SK, Thapa BR, Prasad K (2015) Primary versus secondary achalasia: a diagnostic conundrum. Trop Gastroenterol 36(2):86–95. https://doi.org/10.7869/tg.259
Gupta P, Debi U, Sinha SK, Prasad KK (2015) Primary versus secondary achalasia: new signs on barium esophagogram. Indian J Radiol Imaging 25(3):288–295. https://doi.org/10.4103/0971-3026.161465
Woodfield CA, Levine MS, Rubesin SE, Langlotz CP, Laufer I (2000) Diagnosis of primary versus secondary achalasia: reassessment of clinical and radiographic criteria. AJR Am J Roentgenol 175(3):727–731. https://doi.org/10.2214/ajr.175.3.1750727
Licurse MY, Levine MS, Torigian DA, Barbosa EM Jr (2014) Utility of chest CT for differentiating primary and secondary achalasia. Clin Radiol 69(10):1019–1026. https://doi.org/10.1016/j.crad.2014.05.005
Moonka R, Patti MG, Feo CV, Arcerito M, De Pinto M, Horgan S, Pellegrini CA (1999) Clinical presentation and evaluation of malignant pseudoachalasia. J Gastrointest Surg 3(5):456–461. https://doi.org/10.1016/s1091-255x(99)80097-3
Carter M, Deckmann RC, Smith RC, Burrell MI, Traube M (1997) Differentiation of achalasia from pseudoachalasia by computed tomography. Am J Gastroenterol 92(4):624–628
Tracey JP, Traube M (1994) Difficulties in the diagnosis of pseudoachalasia. Am J Gastroenterol 89(11):2014–2018
Kulinna-Cosentini C, Schima W, Ba-Ssalamah A, Cosentini EP (2014) MRI patterns of Nissen fundoplication: normal appearance and mechanisms of failure. Eur Radiol 24(9):2137–2145. https://doi.org/10.1007/s00330-014-3267-x
Nasa M, Bhansali S, Choudhary NS, Sud R (2018) Uncommon cause of dysphagia: paraneoplastic achalasia. BMJ Case Rep. 2018(7):bcr2017223929. https://doi.org/10.1136/bcr-2017-223929
Ulla JL, Fernandez-Salgado E, Alvarez V, Ibañez A, Soto S, Carpio D, Vazquez-Sanluis J, Ledo L, Vazquez-Astray E (2008) Pseudoachalasia of the cardia secondary to nongastrointestinal neoplasia. Dysphagia 23(2):122–126. https://doi.org/10.1007/s00455-007-9104-5
Branchi F, Tenca A, Bareggi C, Mensi C, Mauro A, Conte D, Penagini R (2016) A case of pseudoachalasia hiding a malignant pleural mesothelioma. Tumori 102(Suppl. 2). https://doi.org/10.5301/tj.5000521
Bonavina L, Bona D, Saino G et al (2007) Pseudoachalasia occurring after laparoscopic Nissen fundoplication and crural mesh repair. Langenbecks Arch Surg 392:653–656
Harbaugh JW, Clayton SB (2020) Pseudoachalasia Following Nissen fundoplication. ACG Case Rep J 7(2):e00318. https://doi.org/10.14309/crj.0000000000000318.
Ellingson TL, Kozarek RA, Gelfand MD, Botoman AV, Patterson DJ (1995) Iatrogenic achalasia. A case series J Clin Gastroenterol 20(2):96–99. https://doi.org/10.1097/00004836-199503000-00004
Gockel I, Eckardt VF, Schmitt T, Junginger T (2005) Pseudoachalasia: a case series and analysis of the literature. Scand J Gastroenterol 40(4):378–385. https://doi.org/10.1080/00365520510012118
Ramos AC, Murakami A, Lanzarini EG, Neto MG, Galvão M (2009) Achalasia and laparoscopic gastric bypass. Surg Obes Relat Dis 5(1):132–134. https://doi.org/10.1016/j.soard.2008.05.004
Torghabeh MH, Afaneh C, Saif T, Dakin GF (2015) Achalasia 5 years following Roux-en-y gastric bypass. J Minim Access Surg 11(3):203–204. https://doi.org/10.4103/0972-9941.159854
Kolb JM, Jonas D, Funari MP, Hammad H, Menard-Katcher P, Wagh MS (2020) Efficacy and safety of peroral endoscopic myotomy after prior sleeve gastrectomy and gastric bypass surgery. World J Gastrointest Endosc. 12(12):532–541. https://doi.org/10.4253/wjge.v12.i12.532
Aiolfi A, Foschi D, Zappa MA, Dell’Era A, Bareggi E, Rausa E, Micheletto G, Bona D (2021) Laparoscopic Heller myotomy and Dor fundoplication for the treatment of esophageal achalasia after sleeve gastrectomy-a video vignette. Obes Surg 31(3):1392–1394. https://doi.org/10.1007/s11695-020-05114-x
Dufour JF, Fawaz KA, Libby ED (1997) Botulinum toxin injection for secondary achalasia with esophageal varices. Gastrointest Endosc 45(2):191–193. https://doi.org/10.1016/s0016-5107(97)70248-7
Fishman VM, Parkman HP, Schiano TD, Hills C, Dabezies MA, Cohen S, Fisher RS, Miller LS (1996) Symptomatic improvement in achalasia after botulinum toxin injection of the lower esophageal sphincter. Am J Gastroenterol 91(9):1724–1730
Woods CA, Foutch PG, Waring JP, Sanowski RA (1989) Pancreatic pseudocyst as a cause for secondary achalasia. Gastroenterology 96(1):235–239. https://doi.org/10.1016/0016-5085(89)90786-5
Sousa RG, Figueiredo PC, Pinto-Marques P, Meira T, Novais LA, Vieira AI, Luz C, Borralho P, Freitas J (2013) An unusual cause of pseudoachalasia: the Alport syndrome-diffuse leiomyomatosis association. Eur J Gastroenterol Hepatol 25(11):1352–1357. https://doi.org/10.1097/MEG.0b013e328361dd17
Author information
Authors and Affiliations
Contributions
LYKZ: acquisition of data, analysis and interpretation of data, drafting the article, and final approval of the version to be published. FAMH: conception and design, acquisition of data, analysis and interpretation of data, drafting the article, and final approval of the version to be published. VV: conception and design, review for intellectual content, and final approval of the version to be published. MGP: conception and design, review for intellectual content, and final approval of the version to be published.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zanini, L.Y.K., Herbella, F.A.M., Velanovich, V. et al. Modern insights into the pathophysiology and treatment of pseudoachalasia. Langenbecks Arch Surg 409, 65 (2024). https://doi.org/10.1007/s00423-024-03259-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-024-03259-2