Abstract
Aims
To study the correlation between clinicopathological risk factors and the risk for intervention-requiring cancer recurrence in patients with small papillary thyroid cancers (sPTCs).
Materials and methods
Records for 397 patients with sPTC (T1 ≤ 20mm) were obtained from the Scandinavian Quality Register for Thyroid, Parathyroid and Adrenal Surgery (SQRTPA) between 2010 and 2016. Follow-up time was at least 5 years. Data regarding intervention-requiring cancer recurrence were obtained from patient medical records and analysed regarding lymph node (LN) status (N0, N1a and N1b) and recurrence.
Results
Age was significantly lower in the N1a and N1b groups compared to N0 (45 vs. 40.5 vs. 49 years, respectively; p = 0.002). Tumour size was smaller in the N1a group compared to N1b group (9 vs. 11.8 mm; p <0.01). The mean number of metastatic LNs at initial surgery was higher in the N1b compared to N1a group (6.6 vs. 3; p = 0.001), and in the recurrent compared to the non-recurrent group (7 versus 3.9; p <0.01). The recurrence rate was higher in the N1b group than the N1a and N0 groups (25% vs. 2.4% vs. 1.4%, respectively; p = 0.001).
Conclusions
Lymph node stage N1b at diagnosis, and having five or more metastatic nodes, are strong risk factors for cancer recurrence and decreased disease-free survival in sPTC. The management of patients with sPTC should include thorough lymph node mapping for optimal treatment and individual risk stratification.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Thyroid cancer (TC) is the most common cancer of the endocrine glands. Papillary thyroid cancer (PTC) is the most common subtype of TC, with an increasing incidence worldwide [1,2,3]. The rising incidence is partly attributed to established risk factors such as ionizing radiation [1, 2]. Improved diagnostics are also an important contributing factor to the increment. These include ultrasound and fine-needle aspiration cytology, which enable the detection of small papillary thyroid cancers (sPTCs, ≤20mm in size) as well as papillary thyroid microcarcinoma (PTMC, ≤10 mm) [2, 3].
Annual incidence in Sweden per 100,000 people is 8 cases for women and 2.4 cases for men, constituting 550-600 new patients per year [2]. Despite the increasing incidence, the prognosis for sPTC is excellent, with a 10-year survival rate of 90% - 95% [2, 3]. Due to the good prognosis, the general approach is towards less aggressive management of these small tumours [4]. Although most sPTCs are considered low risk cancers, some are considerably more aggressive than others with a high recurrence risk [2, 5,6,7,8].
PTC often metastasizes to locoregional cervical lymph nodes. Although the finding of locoregional metastases at diagnosis seems to have a little effect on long-term patient survival [9], it is associated with an increased risk of future locoregional recurrence [10, 11]. Depending on the definition, locoregional recurrences have been described in up to 1.2% - 28% in patients with PTC [9, 12]. Locoregional recurrences are not immediately life-threatening, but they present as a stressor to both physicians and patients. The primary treatment of PTC in Sweden, according to current national guidelines, is total thyroidectomy complemented by postoperative radioactive iodine (RAI) and thyroxine suppression therapy (TST) [2, 13]. For PTMC, hemithyroidectomy is considered sufficient, and in some cases active surveillance can be used in order to avoid surgery [2, 7, 9, 14]. Several options for treatment of recurrent disease are available, depending on the type of recurrence. These include surgery, RAI ablation, external beam radiation therapy (EBRT) and other systemic therapies [2, 13].
The suggested risk factors for cancer recurrence are tumour size, multifocality, vascular invasion, extrathyroidal extension (ETE), lymph node (LN) and distant metastasis [6, 11, 15,16,17,18]. Further, LN metastasis location, number, size and ratio (involved LN/retrieved LN) and extranodal extension (ENE) at time of diagnosis are also important risk factors for recurrence [19,20,21,22,23,24]. Previously, age was believed to be a strong predictive factor of death from thyroid cancer complications, but is now more generally considered in conjunction with other variables [2, 25]. Although females have a higher incidence of PTC, and being male is associated with a higher prevalence of advanced-stage thyroid cancer, gender in general is not considered as a risk factor for recurrence in patients with PTC [26,27,28]. Molecular biomarkers are not yet widely implemented to help differentiate the relatively small number of aggressive cancers from the larger population of more indolent tumours. The BRAF-V600E mutation carries an increased risk in the intermediate and high risk patient group, but cannot be used as the sole discriminator, as up to 60% of PTCs carry the BRAF-V600E mutation [22, 29]. Telomerase reverse transcriptase (TERT) promoter mutation was found to be an independent risk factor for recurrence and mortality in well differentiated thyroid cancers [30], and, in combination with the BRAF-V600E mutation, TERT promoter mutation is associated with an increased risk of structural disease recurrence [22, 31].
The paradigm shift in management of patients with small PTCs towards less aggressive treatment warrants further understanding of the predictors of cancer recurrence. This would reduce unnecessary treatments for indolent thyroid cancers and improve outcomes in patients with clinically more aggressive cancers.
The aim of this study was to investigate the correlation between demographic factors (age, sex, tumour characteristics such as nodal status, tumour diameter, number of metastasized lymph nodes and multifocality) and the risk for intervention-requiring cancer recurrence in the Swedish sPTC population.
Materials and methods
Cohort selection
This study is a registry-based retrospective observational cohort study based on a validated and prospectively maintained register—the Scandinavian Quality Register for Thyroid, Parathyroid and Adrenal Surgery (SQRTPA) [32]. The SQRTPA register was established in 2004 and is the world’s first quality register for endocrine surgery. The SQRTPA covers almost 100% of thyroid surgeries in Sweden. It is validated against the national patient register and is one of the few registers to have an internal quality audit that randomly checks the operating centres every year [32]. The register does not, however, provide longitudinal, long-term follow-up data regarding local and distant recurrence. Therefore, access to the patients’ surgical, oncological, and pathology records was also obtained for the present study.
Patients from all regions across Sweden who underwent surgery between January 2010 and December 2016 were included, which allowed a minimum follow-up time of 5 years (60 months) based on the latest patient record review (February 2022). The inclusion criteria were a primary diagnosis of sPTC, defined as a tumour ≤20 mm in size, and T1 stage with (N1) or without (N0) cervical lymph node metastases. The N1 group was further divided into N1a and N1b subgroups based on the location of metastases, with N1a classified as metastases in the central cervical lymph nodes (level VI) and N1b classified as metastases to the ipsilateral, bilateral, or contralateral lateral cervical lymph nodes (levels I-V). Patients with Nx lymph node status (where central lymph nodes could not be assessed or fewer than six central lymph nodes could be found) were not included. Patient inclusion was based on the 7th edition of the tumour–node– metastasis (TNM) classification that was current during the study period [33].
Patients were subsequently subdivided into two groups based on whether they received intervention due to cancer recurrence (“recurrence group”) or not (“recurrence-free group”). Intervention-requiring cancer recurrence was defined as any type of clinical or radiological evidence of recurrence at least 3 months after the initial surgery, requiring any type of surgery for local and/or regional lymph node recurrence and/or RAI ablation, EBRT or other systemic treatment. All intervention-requiring recurrences were histologically confirmed by biopsy. Four patients in the cohort (two in the N1a group and two in the N1b group) had elevated thyroglobulin levels but no evidence of structural disease was seen during the follow-ups, and thus no extra treatment beyond the standard postoperative RAI was given. These four patients were included in the recurrence-free group.
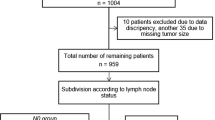
Exclusion criteria were patients that were alive but did not complete a minimum of 5 years (60 months) of follow-up time (n = 15), patients with insufficient medical record information or no access to patient medical records (n = 42). The study cohort was further checked for duplicates and any duplicate records were excluded (n = 72) (Fig. 1). One patient died from PTC before the 5-year minimum follow-up time (after 20 months) but was still included for further analysis. Tumours ≤20 mm formerly classified as T3 have been debated and re-classified in TNM 8th edition [33]. Thus, most of such tumours would be downstaged to T1 tumours according to size. As it was not possible to differentiate this in the register, these patients were excluded in order to have a pure and validated T1 cohort. No T4 tumours ≤20 mm were registered in the SQRTPA during the period. Only patients with M0 (no distant metastasis) status at the time of the diagnosis were included in this study.
Ethical considerations
This study was approved by the Umeå Regional Ethics Committee, permit number 2021-01664, and was carried out in accordance with the EU’s General Data Protection Regulation (GDPR) rules.
Statistics
Descriptive statistics were used to describe the basic characteristics of the three groups (N0, N1a, N1b) and recurrence vs. recurrence-free groups. One-way ANOVA and Pearson’s Chi-square test for categorical variables were used to assess the relationship between each group with the following potential predictors of recurrence: age, sex, tumour size, total number of metastatic LNs, multifocality, recurrence and primary RAI treatment. The Cox proportional hazard model was chosen for multivariable analysis to check for patient demographics and tumour variables.
A recurrence event was defined as described in the cohort selection section, above. The time to recurrence was quantified in months from day of primary surgery to time of the re-evaluation that confirmed the first PTC recurrence during follow-up. Disease-free survival in each group was estimated using the Kaplan–Meier curve, and the estimates among the groups were compared by the log-rank test. In all statistical analyses, a two-tailed p-value < 0.05 was considered statistically significant.
The statistical analyses and graphs were performed using SPSS version 27 (IBM Corporate, Armonk, NY) and GraphPad Prism version 9 (GraphPad Software, San Diego, CA).
Results
The clinicopathological characteristics of the patients regarding nodal status (N0, N1a, N1b) are presented in Table 1. The median age of the patients in the N1b group was lower than the other groups (40.5 years; p = 0.002). The female/male ratio was higher in all groups (p = 0.003). The mean tumour size was smaller in both the N0 and N1b groups compared to N1a (9.3 mm and 9 mm compared to 11.8 mm, respectively; p = 0.001), and more tumours were T1a (1-10mm in size) in the N1b group (60%) compared with the N1a group (37.9%, p = 0.007). The mean number of metastatic LNs was significantly higher in the N1b group than the N1a group (6.64 and 3 respectively, p = 0.001) and the number of patients having five or more metastatic lymph nodes was significantly higher in the N1b group compared to N1a (41.7% vs. 12.9%, respectively; p = 0.001). Intervention-requiring cancer recurrence occurred more often in the N1b group (25%) compared to N1a (2.4%) and N0 groups (1.4%, p = 0.001). The overall intervention-requiring cancer recurrence rate was 5.3% (n = 21).
The clinicopathological characteristics of the patients regarding intervention-requiring cancer recurrence (recurrence vs. recurrence-free groups) are presented in Table 2. The mean number of metastatic lymph nodes was higher in the intervention-requiring cancer recurrence group compared to the recurrence-free group (7 vs. 3.9; p = 0.006). The number of patients with N1b lymph node status was significantly higher in the intervention-requiring recurrence group compared to the recurrence-free group (71.4% vs. 12%, p = 0.001).
The relationship of disease-free survival (DFS) between the two groups (intervention-requiring cancer recurrence vs. recurrence-free) is described in Fig. 2. The Kaplan–Meier curve and log-rank test for DFS demonstrate a significant difference between the two groups regarding LN status (N0, N1a and N1b, p = 0.001) in Fig. 2a, and between the number of metastatic lymph nodes with five LN as cut-off (p = 0.002) in Fig. 2b.
Using the Cox proportional hazard model for regression analysis to assess factors predictive of DFS, only LN status N1b compared to N1a and N0 (hazard ratio (HR) 19.93; 95% confidence interval (CI), 5.76 - 68.82, p = 0.001), and the number of metastatic LNs (five or more) (HR 3.98; 95% CI 1.58 - 10.03, p = 0.003) predicted decreased DFS as shown in Table 3.
Discussion
In this study, a cohort of 397 patients with sPTC (T1) was evaluated regarding intervention-requiring cancer recurrence during a follow-up period of at least 60 months. Basic clinicopathological characteristics regarding both the LN as well as the recurrence status were analysed. The recurrence rates in this study are similar to the ones described in the literature [9]. The overall recurrence rate was 5.3% (n = 21/397) when calculating for intervention-requiring cancer recurrences. The recurrence rate was significantly higher in the N1b group (25%) but mortality is still very low. Only one patient in the whole cohort of 397 died from thyroid cancer. The results support the hypothesis that recurrence rate, rather than mortality rate, is a preferable clinical measure when discussing sPTC. Given the difference regarding intervention-requiring cancer recurrence between N1b and N1a/N0, LN status plays an important role in individual risk stratification, and this emphasizes the need for thorough preoperative LN mapping even in sPTC [8]. Central lymph node metastasis (CLNM) has been shown to be the strongest risk factor for lateral lymph node metastasis. The sensitivity of the preoperative palpation or ultrasound for CLNM detection is low, especially when it comes to microscopic disease. This puts patients with PTC at risk of being under-staged and under-treated [34, 35]. One can argue that routine prophylactic central lymph node dissection is needed in order to obtain more appropriate risk stratification, but this leads to an increased risk for postoperative complications such as hypoparathyroidism and recurrent laryngeal nerve injuries, especially in low volume centres [35]. Furthermore, there are reports that postoperative RAI treatment has a negative impact on overall wellbeing and could possibly induce other malignancies [36]. More studies with large numbers of patients are warranted to find out whether our results imply an overtreatment of some sPTCs (N1a) when it comes to central lymph node surgery and postoperative RAI therapy.
Age is one of the most important prognostic factors for cancer-specific mortality in patients with PTC and it is currently evaluated together with other factors when assessing the risk for recurrences. The 8th edition of the American Joint Committee on Cancer (AJCC), has raised the age cut-off from 45 to 55 years, thus reclassifying many patients <55 years with differentiated PTC and no evident distant metastasis (M0) as stage I [4]. As patients in this study were treated according to the 7th edition of AJCC with an age cut-off of 45, this classification was kept. The median age in the N1b group (and N1 group in total) was lower than that of the N0 group (Table 1). However, the median age did not differ significantly between the groups when comparing recurrence and tended to be slightly lower in the intervention-requiring cancer recurrence group (Table 2). In both groups the median age was above the cut-off of 45 years.
The female/male ratio was significantly higher in all groups regarding LN status (Table 1), but no difference was observed when comparing recurrence status (Table 2) or DFS. Whether male sex is a predictive risk factor for recurrence has been controversial, but our results are in line with the latest data showing that female sex is a risk factor for PTC in general, but is not considered as a risk factor for recurrence in PTC or impact on the DFS [26, 28].
Tumour size ≥20mm, especially in combination with other risk factors such as BRAF and/or TERT mutations or ETE, is an established risk factor for LN metastasis and recurrence [22]. Well-differentiated PTMCs without worrisome features are considered as extremely low risk tumours and can be treated with lobectomy only, without the need for prophylactic LN dissection or RAI treatment. However, some of these tumours do recur with a rate ranging between 1% - 5% depending on multifocality. One study showed that 50% - 60% of patients with PTMCs have micrometastases that can be indolent and subclinical for several years [37]. Interestingly, we found that mean tumour size was significantly smaller in the N1b group compared to the N1a group. However, there were no significant differences in the recurrence groups or effect on the DFS, indicating that size alone cannot be considered a robust predictor for recurrence in sPTC.
Multifocality is considered a prognostic marker and risk factor for PTC recurrence, especially if more than two foci are present [22, 38, 39]. In our results, multifocality was not a risk factor for recurrence or decreased DFS.
These results show that LN status at presentation (N0, N1a or N1b) and clinical N1 status at diagnosis is correlated with risk for recurrence, a finding that is in line with previous publications [9, 22]. The number of metastatic lymph nodes is usually weighed together with the size of the metastasis and presence of ENE. According to the 2015 American Thyroid Association (ATA) guidelines, five or more metastatic LNs are considered as a risk factor for recurrence in patients with PTC [10, 19, 22, 23, 38]. In our cohort, analysis of the recurrence groups confirmed this (Tables 2 and 3, Fig. 2b). Regarding LN status as a separate risk factor, most of the patients in the N1a and N1b groups had fewer than five metastatic LNs (Table 1). However, when analysing the recurrence groups regarding LN status and number of metastatic LN nodes, our study results show that 60% (9/15) of the patients in the N1b group in the recurrence group had five or more metastatic LNs. In some cases of low-risk PTCs with tumour size up to 4 cm and without signs of LN metastasis or ETE, the latest ATA guidelines recommend hemithyroidectomy without the need of completion hemithyroidectomy or post operative RAI as sufficient treatment [38]. According to our results, this recommendation (and the active surveillance approach for PTMC) should be carefully considered as tumour size alone should not be used singularly for the preoperative surgical decision, rather in combination with other factors such as thorough preoperative LN status mapping and cytology with molecular analysis.
The strengths of this study are the accurate and reliable patient data based on thorough revision of medical and pathological reports in addition to the validated SQRTPA register data, as well as the follow-up time of at least 60 months (5 years) for all patients and up to 145 months (12 years) for some. The limitations of the study are the lack of molecular analyses of the tumours such as BRAF or TERT mutations, as these analyses were not routinely performed during the study period and not included in the Swedish national guidelines. Information on the size of the metastasized LNs or the ENE was not obtained, as this was lacking in many patients’ medical records. ETE of the tumour is an established risk factor for recurrence. However, as tumours ≤ 20mm with minimal ETE were classified as T3 during the study period, these could not be identified in the register and were therefore not included in the study.
Conclusions
According to the present results, lateral lymph node metastasis (N1b) at the time of diagnosis and five or more metastatic LNs are the strongest predictors for cancer recurrence in patients with sPTC. Other factors cannot predict recurrence on their own, and should be used in combination with molecular testing to add strength to appropriate individual risk stratification. Small PTC should be considered as a heterogenous disease in which both treatment and follow-up should be individualized and tailored for each patient based on the clinicopathological features of the tumour and the presence of lymph node metastasis.
Abbreviations
- TC:
-
Thyroid cancer
- PTC:
-
Papillary thyroid cancer
- sPTC:
-
Small papillary thyroid cancer
- PTMC:
-
Papillary thyroid microcarcinoma
- RAI:
-
Radioactive iodine
- TST:
-
Thyroxin suppression therapy
- EBRT:
-
External beam radiation therapy
- ETE:
-
Extra thyroidal extension
- ENE:
-
Extra nodal extension
- LN:
-
Lymph node
- SQRTPA:
-
Scandinavian Quality Register for Thyroid, Parathyroid and Adrenal Surgery
- DFS:
-
Disease-free survival
- CLNM:
-
Central lymph node metastasis
- AJCC:
-
American Joint Committee on Cancer
References
Nikiforov YE (2010) Is ionizing radiation responsible for the increasing incidence of thyroid cancer? Cancer 116(7):1626–1628
RCC. Thyroid cancer, Swedish national guidelines 2022 2021 [updated 2021-09-07; cited 2022. https://www.cancercentrum.se/samverkan/cancerdiagnoser/skoldkortel/vardprogram/gallande-vardprogram/.
Vaccarella S, Franceschi S, Bray F, Wild CP, Plummer M, Dal Maso L (2016) Worldwide Thyroid-Cancer Epidemic? The Increasing Impact of Overdiagnosis. N Engl J Med 375(7):614–617
Tuttle RM, Haugen B, Perrier ND (2017) Updated American Joint Committee on Cancer/Tumor-Node-Metastasis Staging System for Differentiated and Anaplastic Thyroid Cancer (Eighth Edition): What Changed and Why? Thyroid 27(6):751–756
Pellegriti G, Scollo C, Lumera G, Regalbuto C, Vigneri R, Belfiore A (2004) Clinical behavior and outcome of papillary thyroid cancers smaller than 1.5 cm in diameter: study of 299 cases. J Clin Endocrinol Metab 89(8):3713–3720
Marques P, Leite V, Bugalho MJ (2014) Retrospective Analysis of 255 Papillary Thyroid Carcinomas </=2 cm: Clinicohistological Features and Prognostic Factors. Eur Thyroid J 3(4):258–263
Freni F, Galletti B, Galletti F, Dionigi G (2018) Improved outcomes for papillary thyroid microcarcinoma care: active surveillance and case volume. Ther Adv Endocrinol Metab 9(7):185–186
Bayadsi H, Bergman M, Sund M, Hennings J (2020) Invasiveness and Metastatic Aggressiveness in Small Differentiated Thyroid Cancers: Demography of Small Papillary Thyroid Carcinomas in the Swedish Population. World J Surg 44(2):461–468
Tufano RP, Clayman G, Heller KS, Inabnet WB, Kebebew E, Shaha A et al (2015) Management of recurrent/persistent nodal disease in patients with differentiated thyroid cancer: a critical review of the risks and benefits of surgical intervention versus active surveillance. Thyroid 25(1):15–27
Kim SY, Kim BW, Pyo JY, Hong SW, Chang HS, Park CS (2018) Macrometastasis in Papillary Thyroid Cancer Patients is Associated with Higher Recurrence in Lateral Neck Nodes. World J Surg 42(1):123–129
Ito Y, Tomoda C, Uruno T, Takamura Y, Miya A, Kobayashi K et al (2005) Ultrasonographically and anatomopathologically detectable node metastases in the lateral compartment as indicators of worse relapse-free survival in patients with papillary thyroid carcinoma. World J Surg 29(7):917–920
Grogan RH, Kaplan SP, Cao H, Weiss RE, Degroot LJ, Simon CA et al (2013) A study of recurrence and death from papillary thyroid cancer with 27 years of median follow-up. Surgery 154(6):1436–1446
Cabanillas ME, McFadden DG, Durante C (2016) Thyroid cancer. Lancet 388(10061):2783–2795
Haser GC, Tuttle RM, Su HK, Alon EE, Bergman D, Bernet V et al (2016) Active Surveillance for Papillary Thyroid Microcarcinoma: New Challenges and Opportunities for the Health Care System. Endocr Pract 22(5):602–611
Wu MH, Shen WT, Gosnell J, Duh QY (2015) Prognostic significance of extranodal extension of regional lymph node metastasis in papillary thyroid cancer. Head Neck 37(9):1336–1343
Lundgren CI, Hall P, Dickman PW, Zedenius J (2006) Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer 106(3):524–531
Zhang X, Zhang L, Xue S, Wang P, Chen G (2019) Predictive factors of lateral lymph node metastasis in solitary papillary thyroid microcarcinoma without gross extrathyroidal extension. Asian J Surg 42(4):563–570
Deng Y, Zhu G, Ouyang W, Pan L, Feng H, Wu J et al (2019) Size of the Largest Metastatic Focus to the Lymph Node Is Associated with Incomplete Response of Pn1 Papillary Thyroid Carcinoma. Endocr Pract 25(9):887–898
Jeon MJ, Yoon JH, Han JM, Yim JH, Hong SJ, Song DE et al (2013) The prognostic value of the metastatic lymph node ratio and maximal metastatic tumor size in pathological N1a papillary thyroid carcinoma. Eur J Endocrinol 168(2):219–225
Clain JB, Scherl S, Dos Reis L, Turk A, Wenig BM, Mehra S et al (2014) Extrathyroidal extension predicts extranodal extension in patients with positive lymph nodes: an important association that may affect clinical management. Thyroid 24(6):951–957
Kim WW, Lee J, Jung JH, Park HY, Jeong JY, Park J-Y et al (2020) Predictive Risk Factors for Recurrence or Metastasis in Papillary Thyroid Cancer. Int J Thyroidol 13(2):111–117
Tarasova VD, Tuttle RM (2017) Current Management of Low Risk Differentiated Thyroid Cancer and Papillary Microcarcinoma. Clin Oncol (R Coll Radiol) 29(5):290–297
Randolph GW, Duh QY, Heller KS, LiVolsi VA, Mandel SJ, Steward DL et al (2012) The prognostic significance of nodal metastases from papillary thyroid carcinoma can be stratified based on the size and number of metastatic lymph nodes, as well as the presence of extranodal extension. Thyroid 22(11):1144–1152
Lindfors H, Ihre Lundgren C, Zedenius J, Juhlin CC, Shabo I (2021) The Clinical Significance of Lymph Node Ratio and Ki-67 Expression in Papillary Thyroid Cancer. World J Surg 45(7):2155–2164
Ito Y, Kudo T, Kobayashi K, Miya A, Ichihara K, Miyauchi A (2012) Prognostic factors for recurrence of papillary thyroid carcinoma in the lymph nodes, lung, and bone: analysis of 5,768 patients with average 10-year follow-up. World J Surg 36(6):1274–1278
Pellegriti G, Frasca F, Regalbuto C, Squatrito S, Vigneri R (2013) Worldwide increasing incidence of thyroid cancer: update on epidemiology and risk factors. J Cancer Epidemiol 2013:965212
Kim WW, Lee J, Jung JH, Park HY, Jeong JY, Park JY, Tufano RP (2020) Predictive Risk Factors for Recurrence or Metastasis in Papillary Thyroid Cancer. International Journal of. Thyroidology 13(2):111–117
Park J, Kim K, Lim DJ, Bae JS, Kim JS (2021) Male sex is not an independent risk factor for recurrence of differentiated thyroid cancer: a propensity score-matching study. Sci Rep 11(1):14908
Xing M, Alzahrani AS, Carson KA, Shong YK, Kim TY, Viola D et al (2015) Association between BRAF V600E mutation and recurrence of papillary thyroid cancer. J Clin Oncol 33(1):42–50
Melo M, da Rocha AG, Vinagre J, Batista R, Peixoto J, Tavares C et al (2014) TERT promoter mutations are a major indicator of poor outcome in differentiated thyroid carcinomas. J Clin Endocrinol Metab 99(5):E754–E765
Xing M, Liu R, Liu X, Murugan AK, Zhu G, Zeiger MA et al (2014) BRAF V600E and TERT promoter mutations cooperatively identify the most aggressive papillary thyroid cancer with highest recurrence. J Clin Oncol 32(25):2718–2726
SQRTPA. Scandinavian Quality Register for Thyroid, Parathyriod and Adrenal Surgery - Yearly report 2018 2018 [updated 28 September 2018; cited 2021. https://sqrtpa.se/sites/default/files/sqrtpa/annual_reports/arsrapport_2018_final.pdf.
Nam SH, Bae MR, Roh JL, Gong G, Cho KJ, Choi SH et al (2018) A comparison of the 7th and 8th editions of the AJCC staging system in terms of predicting recurrence and survival in patients with papillary thyroid carcinoma. Oral Oncol 87:158–164
Nylen C, Eriksson FB, Yang A, Aniss A, Turchini J, Learoyd D et al (2021) Prophylactic central lymph node dissection informs the decision of radioactive iodine ablation in papillary thyroid cancer. Am J Surg 221(5):886–892
Moreno MA, Edeiken-Monroe BS, Siegel ER, Sherman SI, Clayman GL (2012) In papillary thyroid cancer, preoperative central neck ultrasound detects only macroscopic surgical disease, but negative findings predict excellent long-term regional control and survival. Thyroid 22(4):347–355
Pasqual E, Schonfeld S, Morton LM, Villoing D, Lee C, Berrington de Gonzalez A et al (2022) Association Between Radioactive Iodine Treatment for Pediatric and Young Adulthood Differentiated Thyroid Cancer and Risk of Second Primary Malignancies. J Clin Oncol 40(13):1439–1449
Wada N, Duh QY, Sugino K, Iwasaki H, Kameyama K, Mimura T et al (2003) Lymph node metastasis from 259 papillary thyroid microcarcinomas: frequency, pattern of occurrence and recurrence, and optimal strategy for neck dissection. Ann Surg 237(3):399–407
Haugen BR, Alexander EK, Bible KC, Doherty GM, Mandel SJ, Nikiforov YE et al (2016) 2015 American Thyroid Association Management Guidelines for Adult Patients with Thyroid Nodules and Differentiated Thyroid Cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26(1):1–133
Kim H, Kwon H, Moon BI (2021) Association of Multifocality With Prognosis of Papillary Thyroid Carcinoma: A Systematic Review and Meta-analysis. JAMA Otolaryngol Head Neck Surg 147(10):847–854
Funding
Open access funding provided by Umea University. This study was funded by the Unit of Research Education and Development, Region Jämtland Härjedalen County, Sweden (Grant number: JLL-940567) and Jämtland County Cancer and Care Fund, Sweden (Grant number: 748). Open access funding provided by Umeå University, Sweden.
Author information
Authors and Affiliations
Contributions
H. Bayadsi, C. Nylén, J. Angelsten, M. Sund and J. Hennings contributed to the study conception and design. Material preparation, data collection and analyses were performed by H. Bayadsi, C. Nylén, M. Sandström and J. Angelsten. The first draft of the manuscript was written by H. Bayadsi, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bayadsi, H., Nylén, C., Sandström, M. et al. Risk factors for recurrent disease in small papillary thyroid cancers – a Swedish register-based study. Langenbecks Arch Surg 408, 162 (2023). https://doi.org/10.1007/s00423-023-02905-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02905-5