Abstract
Purpose
The aim of this retrospective study was to evaluate a revised classification system for predicting the difficulty of laparoscopic partial liver resection.
Methods
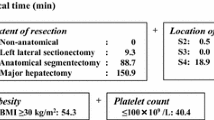
Patients who had undergone initial laparoscopic partial liver resection for a solitary lesion from January 2012 to February 2021were classified into two groups according to the type of procedure performed, “scooping-out” versus “cutting.” The participants were then further divided into “small” and “large” subgroups according to the tumor’s depth and diameter. Finally, they were categorized into two groups, namely “standard” and “advanced.” Operative outcomes were compared between the two groups and the proposed revised system for classifying difficulty of laparoscopic partial liver resection compared with the existing scoring system.
Results
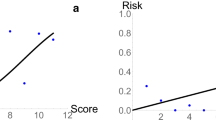
Of the 65 procedures assessed, 40 were categorized as standard and 25 as advanced. Tumor size (P < 0.001), operation time (P < 0.001), volume of intraoperative blood loss (P = 0.001), rate of the Pringle maneuver (P = 0.044), and resected liver weight (P < 0.001) were significantly greater in the advanced than in the standard group. Differences in operation time and intraoperative blood loss were not identified by the existing difficulty scoring system.
Conclusion
The proposed revised classification is useful for predicting the difficulty of laparoscopic partial liver resection.



Similar content being viewed by others
Data availability
The dataset analyzed for the current study is available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
Kawaguchi Y, Hasegawa K, Wakabayashi G et al (2016) Survey results on daily practice in open and laparoscopic liver resections from 27 centers participating in the second International Consensus Conference. J Hepatobiliary Pancreat Sci 23:283–288
Hibi T, Cherqui D, Geller DA, Itano O, Kitagawa Y, Wakabayashi G (2016) Expanding indications and regional diversity in laparoscopic liver resection unveiled by the International Survey on Technical Aspects of Laparoscopic Liver Resection (INSTALL) study. Surg Endosc 30:2975–2983
Wong-Lun-Hing EM, van Dam RM, van Breukelen GJ et al (2017) Randomized clinical trial of open versus laparoscopic left lateral hepatic sectionectomy within an enhanced recovery after surgery programme (ORANGE II study). Br J Surg 104:525–535
Fretland ÅA, Dagenborg VJ, Bjørnelv GMW et al (2018) Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg 267:199–207
Wakabayashi G, Cherqui D, Geller DA et al (2015) Recommendations for laparoscopic liver resection: a report from the second international consensus conference held in Morioka. Ann Surg 261:619–629
Ban D, Tanabe M, Ito H et al (2014) A novel difficulty scoring system for laparoscopic liver resection. J Hepatobiliary Pancreat Sci 21:745–753
Halls MC, Berardi G, Cipriani F et al (2018) Development and validation of a difficulty score to predict intraoperative complications during laparoscopic liver resection. Br J Surg 105:1182–1191
Tanaka S, Kubo S, Kanazawa A et al (2017) Validation of a difficulty scoring system for laparoscopic liver resection: a multicenter analysis by the Endoscopic Liver Surgery Study Group in Japan. J Am Coll Surg 225:249-258.e1
Koch M, Garden OJ, Padbury R et al (2011) Bile leakage after hepatobiliary and pancreatic surgery: a definition and grading of severity by the International Study Group of Liver Surgery. Surgery 149:680–688
Guro H, Cho JY, Han HS et al (2018) Laparoscopic liver resection of hepatocellular carcinoma located in segments 7 or 8. Surg Endosc 32:872–878
Lee W, Han HS, Yoon YS, Cho JY, Choi Y, Shin HK (2014) Role of intercostal trocars on laparoscopic liver resection for tumors in segments 7 and 8. J Hepatobiliary Pancreat Sci 21:E65-68
Lafaro K, Grandhi MS, Herman JM, Pawlik TM (2016) The importance of surgical margins in primary malignancies of the liver. J Surg Oncol 113:296–303
Pawlik TM, Scoggins CR, Zorzi D et al (2005) Effect of surgical margin status on survival and site of recurrence after hepatic resection for colorectal metastases. Ann Surg 241:715–722
Montalti R, Tomassini F, Laurent S et al (2015) Impact of surgical margins on overall and recurrence-free survival in parenchymal-sparing laparoscopic liver resections of colorectal metastases. Surg Endosc 29:2736–2747
Mise Y, Hasegawa K, Shindoh J et al (2015) The feasibility of third or more repeat hepatectomy for recurrent hepatocellular carcinoma. Ann Surg 262:347–357
Kobayashi Y, Shindoh J, Igata Y, Okubo S, Hashimoto M (2020) A novel scoring system for evaluating the difficulty of lysis of adhesion and surgical risk at repeat hepatectomy. J Hepatobiliary Pancreat Sci 27:191–199
Acknowledgements
We thank Dr. Trish Reynolds, MBBS, FRACP, from Edanz (http://jp.edanz.com/ac), for editing the English text of a draft of this manuscript.
Funding
This study was supported by JSPS KAKENHI (Grant Number 21K15515).
Author information
Authors and Affiliations
Contributions
Study conception and design: Onda S. Acquisition of data: Onda S, Furukawa K, Haruki K, Shirai Y, Hamura R, Yasuda J, Shiozaki H, Gocho T, Shiba H. Analysis and interpretation of data: Furukawa K, Haruki K, Shirai Y. Drafting of manuscript: Onda S. Critical revision of manuscript: Ikegami T.
Corresponding author
Ethics declarations
Ethics approval
The study met the ethical standards of the World Medical Association Declaration of Helsinki and its protocol was approved by the Ethics Committee of the Jikei University School of Medicine (27-177[8062]).
Conflict of interest
The authors declare no competing interests.
Consent
Written informed consent was obtained from each patient for their surgical procedures.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Onda, S., Furukawa, K., Haruki, K. et al. Proposal for a revised system for classifying difficulty of laparoscopic partial liver resection. Langenbecks Arch Surg 406, 1533–1541 (2021). https://doi.org/10.1007/s00423-021-02253-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-021-02253-2