Abstract
Objective
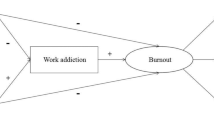
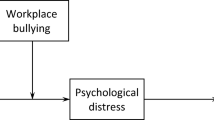
This study aims to test whether health workers experiencing both depression, anxiety and burnout would show severer burnout symptoms, and the potential moderating effect of anxiety and depression on mindfulness improving burnout.
Methods
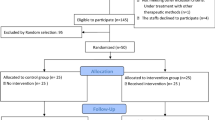
This study was conducted in a comprehensive hospital of China in 2016. A total of 924 healthcare professionals were included in this cross-sectional study with a response rate of 82.0%. Maslach Burnout Inventory, Patient Health Questionnaire‐9, Generalized Anxiety Disorder, Perceived Stress Scale and Short Inventory of Mindfulness Capability were used to measure burnout, depression, anxiety, perceived stress and mindfulness. Univariate analysis, correlation analysis, mediation analysis and moderated mediation analysis were conducted.
Results
Burnout and anxiety group (BA) and burnout and depression group (BD) reported significantly higher burnout scores compared to the burnout-only group (BO) (59.90 ± 15.700, 56.20 ± 13.190, and 49.99 ± 11.955, respectively). Perceived stress was a mediator between mindfulness and occupational burnout, and depression and anxiety significantly moderated the mediation path between mindfulness and occupational burnout (β for stress in moderated mediation models with depression and anxiety respectively: β = 1.8088, p < 0.001, and β = 1.7908, p < 0.001). For participants who experienced a high level of depression, less occupational burnout was reduced as mindfulness increased. Indirect effect of mindfulness reducing occupational burnout was greater among participants who experienced less anxiety.
Conclusions
Depression and anxiety weakened the mindfulness ability on relieving occupational burnout, which could be the potential mechanism of the worsening effect of depression and anxiety.


Similar content being viewed by others
Availability of data and material
Not applicable.
Code availability
Not applicable.
References
Abdulrahman M, Nair SC, Farooq MM, Al Kharmiri A, Al Marzooqi F, Carrick FR (2018) Burnout and depression among medical residents in the United Arab Emirates: a multicenter study. J Fam Med Primary Care 7(2):435
Aparuhov T, Muthen B (2009) Exploratory structural equation modeling: structural equation modeling. Multidiscip J 16(3):397–438
Ballard ED, Ionescu DF, Voort JLV, Niciu MJ, Richards EM, Luckenbaugh DA, Zarate CA Jr (2014) Improvement in suicidal ideation after ketamine infusion: relationship to reductions in depression and anxiety. J Psychiatr Res 58:161–166
Beck AT (1983) Cognitive therapy of depression: new perspectives. In: Clayton PJ, Barett JE (eds) Treatment of depression. Old controversies and new approaches. Raven Press, New York, pp 265–284
Beck AT, Clark DA (1997) An information processing model of anxiety: a automatic and strategic processes. Behav Res Ther 35(1):49–58
Bianchi R, Brisson R (2019) Burnout and depression: causal attributions and construct overlap. J Health Psychol 24(11):1574–1580
Bianchi R, Schonfeld IS (2018) Burnout-depression overlap: nomological network examination and factor-analytic approach. Scand J Psychol 59(5):532–539
Bianchi R, Schonfeld IS, Laurent E (2015) Is burnout separable from depression in cluster analysis? A longitudinal study. Soc Psychiatry Psychiatr Epidemiol 50(6):1005–1011
Bianchi R, Schonfeld IS, Vandel P, Laurent E (2017) On the depressive nature of the “burnout syndrome”: a clarification. Eur Psychiatry 41:109–110
Bianchi R, Laurent E, Schonfeld IS, Verkuilen J, Berna C (2018) Interpretation bias toward ambiguous information in burnout and depression. Personal Individ Differ 135:216–221
Bianchi R, Laurent E, Schonfeld IS, Bietti LM, Mayor E (2020) Memory bias toward emotional information in burnout and depression. J Health Psychol 25:1567–1575
Braun SE, Auerbach SM, Rybarczyk B, Lee B, Call S (2017) Mindfulness, burnout, and effects on performance evaluations in internal medicine residents. Adv Med Educ Pract 8:591
Brown KW, Ryan RM (2003) The benefits of being present: mindfulness and its role in psychological well-being. J Pers Soc Psychol 84(4):822–848. https://doi.org/10.1037/0022-3514.84.4.822
Creedy D, Sidebotham M, Gamble J, Pallant J, Fenwick J (2017) Prevalence of burnout, depression, anxiety and stress in Australian midwives: a cross-sectional survey. BMC Pregnancy Childbirth 17(1):13
Creswell JD, Lindsay EK (2014) How does mindfulness training affect health? A mindfulness stress buffering account. Curr Dir Psychol Sci 23(6):401–407
Ding Y, Qu J, Yu X, Wang S (2014) The mediating effects of burnout on the relationship between anxiety symptoms and occupational stress among community healthcare workers in China: a cross-sectional study. PLoS One 9(9):e107130
Du X, Luo W, Shen Y, Wei D, Xie P, Zhang J, Qiu J (2015) Brain structure associated with automatic thoughts predicted depression symptoms in healthy individuals. Psychiatry Res Neuroimaging 232(3):257–263
Duan W, Li J (2016) Distinguishing dispositional and cultivated forms of mindfulness: item-level factor analysis of five-facet mindfulness questionnaire and construction of short inventory of mindfulness capability. Front Psychol 7:1348
Duarte J, Pinto-Gouveia J (2016) Effectiveness of a mindfulness-based intervention on oncology nurses’ burnout and compassion fatigue symptoms: a non-randomized study. Int J Nurs Stud 64:98–107. https://doi.org/10.1016/j.ijnurstu.2016.10.002
Epstein RM, Krasner MS (2013) Physician resilience: what it means, why it matters, and how to promote it. Acad Med 88(3):301–303
Gracia Gozalo RM, Ferrer Tarrés JM, Ayora Ayora A, Alonso Herrero M, Amutio Kareaga A, Ferrer Roca R (2019) Application of a mindfulness program among healthcare professionals in an intensive care unit: effect on burnout, empathy and self-compassion. Med Intensiva 43(4):207–216. https://doi.org/10.1016/j.medin.2018.02.005
Ireland MJ, Clough B, Gill K, Langan F, O’Connor A, Spencer L (2017a) A randomized controlled trial of mindfulness to reduce stress and burnout among intern medical practitioners. Med Teach 39(4):409–414
Joiner TE Jr (2000) Depression’s vicious scree: Self-propagating and erosive processes in depression chronicity. Clin Psychol Sci Pract 7(2):203–218
Kabat-Zinn J, Hanh TN (2009) Full catastrophe living: using the wisdom of your body and mind to face stress, pain, and illness: Delta
Klein A, Taieb O, Xavier S, Baubet T, Reyre A (2020) The benefits of mindfulness-based interventions on burnout among health professionals: a systematic review. Explore (NY) 16(1):35–43. https://doi.org/10.1016/j.explore.2019.09.002
Knani M, Fournier P-S, Biron C (2018) Psychosocial risks, burnout and intention to quit following the introduction of new software at work. Work 60(1):95–104
Koutsimani P, Anthony M, Georganta K (2019) The relationship between burnout, depression and anxiety: a systematic review and meta-analysis. Front Psychol 10:284
Kroenke K, Spitzer RL, Williams JBW (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Leiter MP, Durup J (1994) The discriminant validity of burnout and depression: a confirmatory factor analytic study. Anxiety Stress Coping 7(4):357–373
Leung DY, Lam TH, Chan SS (2010) Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health 10:513. https://doi.org/10.1186/1471-2458-10-513
Lew B, Huen J, Yu P, Yuan L, Wang D-F, Ping F, Jia C-X (2019) Associations between depression, anxiety, stress, hopelessness, subjective well-being, coping styles and suicide in Chinese university students. PLoS One 14(7):e0217372
Li YX, Li YM (2006) Developing the diagnostic ctiterion of job burnout (in Chinese). Psychol Sci 29(1):148
Liang XC, Feng XL (2017) Research progress on job burnout among nurses: a systematic review (in Chinese). Chin Nurs Manag 11:19
Lin P, Wang Y, Yang B, Cao F (2018) Reliability and validity of the Short Inventory of Mindfulness Capability Chinese version applied in multi ethnic college students. Nurs Res 32(24):61–65
Luken M, Sammons A (2016) Systematic review of mindfulness practice for reducing job burnout. Am J Occup Ther 70(2):7002250020p7002250021–7002250020p7002250010
Mahmoud JS, Staten RT, Lennie TA, Hall LA (2015) The relationships of coping, negative thinking, life satisfaction, social support, and selected demographics with anxiety of young adult college students. J Child Adolesc Psychiatr Nurs 28(2):97–108
Marchand A, Durand P, Juster R-P, Lupien SJ (2014) Workers’ psychological distress, depression, and burnout symptoms: associations with diurnal cortisol profiles. Scand J Work Environ Health 40(3):305–314
Maslach C, Jackson SE, Leiter MP (1996) Maslach burnout inventory manual, 3rd edn. Consulting Psychologists Press, Palo Alto
Maslach C (1998) A multidimensional theory of burnout. Theor Organ Stress 68:85
Maslach C, Jackson SE (1981) The measurement of experienced burnout. J Organ Behav 2(2):99–113
Maslach C, Jackson SE, Leiter MP, Schaufeli WB, Schwab RL (2016) Maslach Burnout Inventory™ (MBI). http://www.mindgarden.com/117-maslach-burnout-inventory. Accessed 20 June 2019
Mikalauskas A, Benetis R, Širvinskas E, Andrejaitienė J, Kinduris Š, Macas A, Padaiga Ž (2018) Burnout among anesthetists and intensive care physicians. Open Med 13(1):105–112
Mosing MA, Butkovic A, Ullen F (2018) Can flow experiences be protective of work-related depressive symptoms and burnout? A genetically informative approach. J Affect Disord 226:6–11
Murali K, Banerjee S (2018) Burnout in oncologists is a serious issue: what can we do about it? Cancer Treat Rev 68:55–61
Okwaraji F, En A (2014) Burnout and psychological distress among nurses in a Nigerian tertiary health institution. Afr Health Sci 14(1):237–245
Ortega-Campos E, Albendín-García L, Gómez-Urquiza JL, Monsalve-Reyes C, de la Fuente-Solana EI (2019) A multicentre study of psychological variables and the prevalence of burnout among primary health care nurses. Int J Environ Res Public Health 16(18):3242
Paloş R, Vîşcu L (2014) Anxiety, automatic negative thoughts, and unconditional self-acceptance in rheumatoid arthritis: a preliminary study. ISRN Rheumatol 2014:317259
Sibeoni J, Bellon-Champel L, Mousty A, Manolios E, Verneuil L, Revah-Levy A (2019) Physicians’ perspectives about burnout: a systematic review and metasynthesis. J Gen Intern Med 34(8):1578–1590
Spitzer RL, Kroenke K, Williams JB, Lowe B (2006) A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med 166(10):1092–1097. https://doi.org/10.1001/archinte.166.10.1092
Tang Y-Y, Hölzel BK, Posner MI (2015) The neuroscience of mindfulness meditation. Nat Rev Neurosci 16(4):213–225
van der Riet P, Levett-Jones T, Aquino-Russell C (2018) The effectiveness of mindfulness meditation for nurses and nursing students: an integrated literature review. Nurse Educ Today 65:201–211. https://doi.org/10.1016/j.nedt.2018.03.018
Vasconcelos EM, Martino MMF (2018) Predictors of burnout syndrome in intensive care nurses. Rev Gaucha Enferm 38(4):e65354. https://doi.org/10.1590/1983-1447.2017.04.65354
Vella E, McIver S (2019) Reducing stress and burnout in the public-sector work environment: a mindfulness meditation pilot study. Health Promot J Aust 30(2):219–227
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by FL, YW, MZ and BY. The first draft of the manuscript was written by YS and all authors commented on previous versions of the manuscript. Project administration and supervision were performed by FC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of School of Nursing, Shandong University (Date: Sep-9-2016 /No. 2016-R-023).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sun, Y., Liu, F., Wang, Y. et al. Mindfulness improves health worker’s occupational burnout: the moderating effects of anxiety and depression. Int Arch Occup Environ Health 94, 1297–1305 (2021). https://doi.org/10.1007/s00420-021-01685-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00420-021-01685-z