Abstract
Purpose
In daily practice, vitreomacular traction (VMT) is described by the horizontal diameter of its attachment site implying a regular round shape of VMT. We investigated the deviation from this circular area of vitreous traction in patients with VMT.
Methods
A retrospective analysis of optical coherence tomography (OCT) scans was performed. The area of vitreomacular attachment was determined using six radial OCT scans (Ameasured). The assumed circular area of traction was calculated based on measuring the maximal horizontal diameter for comparison (Acircular).
Results
Thirty-seven eyes of 37 patients with pure VMT were included. Patients’ mean age was 72.8 ± 8.2 years. Mean horizontal VMT diameter was 400.8 ± 230.5 μm (median 361 μm; range 44–991 μm). While there was no difference between mean areas of traction for Acircular and Ameasured (P = 0.93), the individual difference (|Acircular − Ameasured|) was 0.042 (± 0.044) mm2 in mean or relative 73.0% (± 135.8%). A difference of ≥ 30% of Ameasured to Acircular was found in 16 eyes (43.2%) and ≥ 100% in 7 eyes (18.9%), respectively.
Conclusion
Vitreous attachment sites possess an irregular non-circular shape in a significant number of eyes with VMT. Consequently, the area of traction appears inaccurately described by its horizontal VMT diameter alone. As the area of traction is important for therapeutic recommendation, our results emphasize the need for a more precise description of the area of traction in eyes with VMT.


Similar content being viewed by others
References
Duker JS, Kaiser PK, Binder S, de Smet MD, Gaudric A, Reichel E, Sadda SR, Sebag J, Spaide RF, Stalmans P (2013) The international vitreomacular traction study group classification of vitreomacular adhesion, traction, and macular hole. Ophthalmology 120:2611–2619. https://doi.org/10.1016/j.ophtha.2013.07.042
Small KW, Shaya FS, La Fontaine M (2015) Post-market experience with ocriplasmin including chronic electrophysiologic changes. Ophthalmic surgery, lasers & imaging retina 46:956–962. https://doi.org/10.3928/23258160-20151008-09
Chatziralli I, Theodossiadis G, Xanthopoulou P, Miligkos M, Sivaprasad S, Theodossiadis P (2016) Ocriplasmin use for vitreomacular traction and macular hole: a meta-analysis and comprehensive review on predictive factors for vitreous release and potential complications. Graefes Arch Clin Exp Ophthalmol 254:1247–1256. https://doi.org/10.1007/s00417-016-3363-5
John VJ, Flynn HW Jr, Smiddy WE, Carver A, Leonard R, Tabandeh H, Boyer DS (2014) Clinical course of vitreomacular adhesion managed by initial observation. Retina (Philadelphia, Pa) 34:442–446. https://doi.org/10.1097/IAE.0b013e3182a15f8b
Dimopoulos S, Bartz-Schmidt KU, Gelisken F, Januschowski K, Ziemssen F (2015) Rate and timing of spontaneous resolution in a vitreomacular traction group: should the role of watchful waiting be re-evaluated as an alternative to ocriplasmin therapy? Br J Ophthalmol 99:350–353. https://doi.org/10.1136/bjophthalmol-2014-304961
Chan CK, Crosson JN, Mein CE, Daher N (2017) Pneumatic vitreolysis for relief of vitreomacular traction. Retina (Philadelphia, Pa) 37:1820–1831. https://doi.org/10.1097/IAE.0000000000001448
Steinle NC, Dhoot DS, Quezada Ruiz C, Castellarin AA, Pieramici DJ, See RF, Couvillion SC, Nasir MA, Avery RL (2017) Treatment of vitreomacular traction with intravitreal perfluoropropane (C3f8) injection. Retina (Philadelphia, Pa) 37:643–650. https://doi.org/10.1097/IAE.0000000000001237
Stalmans P (2016) A retrospective cohort study in patients with tractional diseases of the vitreomacular interface (ReCoVit). Graefes Arch Clin Exp Ophthalmol 254:617–628. https://doi.org/10.1007/s00417-016-3294-1
Theodossiadis GP, Grigoropoulos VG, Theodoropoulou S, Datseris I, Theodossiadis PG (2014) Spontaneous resolution of vitreomacular traction demonstrated by spectral-domain optical coherence tomography. Am J Ophthalmol 157:842–851.e841. https://doi.org/10.1016/j.ajo.2014.01.011
Chatziralli I, Theodossiadis G, Parikakis E, Datseris I, Theodossiadis P (2016) Real-life experience after intravitreal ocriplasmin for vitreomacular traction and macular hole: a spectral-domain optical coherence tomography prospective study. Graefes Arch Clin Exp Ophthalmol 254:223–233. https://doi.org/10.1007/s00417-015-3031-1
Codenotti M, Iuliano L, Fogliato G, Querques G, Bandello F (2014) A novel spectral-domain optical coherence tomography model to estimate changes in vitreomacular traction syndrome. Graefes Arch Clin Exp Ophthalmol 252:1729–1735. https://doi.org/10.1007/s00417-014-2645-z
Paul C, Heun C, Muller HH, Fauser S, Kaymak H, Kazerounian S, Sekundo W, Mennel S, Meyer CH, Schmitz-Valckenberg S, Koss MJ, Feltgen N, Bertelmann T (2016) Impact of vitreoretinal interface architecture on successful vitreomacular traction resolution in eyes scheduled for intravitreal ocriplasmin therapy. Retina (Philadelphia, Pa) DOI https://doi.org/10.1097/iae.0000000000001371
Odrobina D, Michalewska Z, Michalewski J, Dziegielewski K, Nawrocki J (2011) Long-term evaluation of vitreomacular traction disorder in spectral-domain optical coherence tomography. Retina (Philadelphia, Pa) 31:324–331
Paul C, Heun C, Muller HH, Hoerauf H, Feltgen N, Wachtlin J, Kaymak H, Mennel S, Koss MJ, Fauser S, Maier MM, Schumann RG, Mueller S, Chang P, Schmitz-Valckenberg S, Kazerounian S, Szurman P, Lommatzsch A, Bertelmann T (2017) Calculating the individual probability of successful ocriplasmin treatment in eyes with VMT syndrome: a multivariable prediction model from the EXPORT study. The Br J Ophthalmol DOI https://doi.org/10.1136/bjophthalmol-2017-310874
Haller JA, Stalmans P, Benz MS, Gandorfer A, Pakola SJ, Girach A, Kampik A, Jaffe GJ, Toth CA, Group M-TS (2015) Efficacy of intravitreal ocriplasmin for treatment of vitreomacular adhesion: subgroup analyses from two randomized trials. Ophthalmology 122:117–122. https://doi.org/10.1016/j.ophtha.2014.07.045
Cereda MG, Preziosa C, D'Agostino I, Cozzi M, Bottoni F, Pellegrini M, Giani A, Staurenghi G (2017) OCRIPLASMIN FOR VITREOMACULAR TRACTION: LOOKING OUTSIDE THE MACULA: a wide-field optical coherence tomography study. Retina (Philadelphia, Pa) DOI https://doi.org/10.1097/IAE.0000000000001785
Saxena S, Manisha, Meyer CH, Akduman L (2014) Three-dimensional spectral domain optical coherence tomography in vitreomacular traction. BMJ Case Rep 2014 DOI https://doi.org/10.1136/bcr-2013-202065
Aaker GD, Gracia L, Myung JS, Borcherding V, Banfelder JR, D'Amico DJ, Kiss S (2011) Three-dimensional reconstruction and analysis of vitreomacular traction: quantification of cyst volume and vitreoretinal interface area. Arch Ophthalmol (Chicago, Ill : 1960) 129:809–811. https://doi.org/10.1001/archophthalmol.2011.123
Koizumi H, Spaide RF, Fisher YL, Freund KB, Klancnik JM Jr, Yannuzzi LA (2008) Three-dimensional evaluation of vitreomacular traction and epiretinal membrane using spectral-domain optical coherence tomography. Am J Ophthalmol 145:509–517. https://doi.org/10.1016/j.ajo.2007.10.014
Steel DH, Parkes C, Papastavrou VT, Avery PJ, El-Ghrably IA, Habib MS, Sandinha MT, Smith J, Stannard KP, Vaideanu-Collins D, Hillier RJ (2016) Predicting macular hole closure with ocriplasmin based on spectral domain optical coherence tomography. Eye (London, England) 30:740–745. https://doi.org/10.1038/eye.2016.42
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee (ethics committee of the medical department, Philipps-University Marburg, Germany) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Supplementary Figure 1
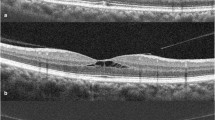
Exemplary measurement of Ameasured. The vertical OCT scan is selected (A) and the upper border of the vitreomacular attachment marked (green line, B, right side). This marked is transferred to the en face projection (blue x, B, left side). This stepped is repeated for all scans (C). Finally, the border marks in the en face projection (blue x, D) are used to measure the enclosed area of traction (yellow cirle, D). (JPG 2833 kb)
Rights and permissions
About this article
Cite this article
Paul, C., Krug, P., Müller, H.H. et al. Comparison of the horizontal diameter to a modeled area of traction in eyes with vitreomacular traction: is the diameter close enough to the truth?. Graefes Arch Clin Exp Ophthalmol 256, 1817–1822 (2018). https://doi.org/10.1007/s00417-018-4055-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-018-4055-0