Abstract
Purpose
To evaluate the incidence, risk factors, and dosages of proton beam therapy associated with cataract development, and long-term visual outcomes after treatment of uveal melanoma.
Methods
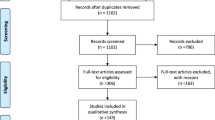
All patients receiving primary proton beam therapy for uveal melanoma between 1998 and 2008 with no signs of cataract before irradiation were included. A minimum follow-up of 12 months was determined. Exclusion criteria included all applied adjuvant therapies such as intravitreal injections, laser photocoagulation, tumor resections, or re-irradiation. For subgroup analysis, we included all patients who underwent brachytherapy between 1998 and 2008 for uveal melanoma, considering the above mentioned inclusion and exclusion criteria.
Results
Two hundred and fifty-eight patients matched our inclusion criteria. Median follow-up was 72.6 months (12.0-167.4 months). Of these 258 patients, 71 patients (66.3 %) presented with cataract after 31.3 months (0.7–142.4 months), of whom 35 (20.4 %) required surgery after 24.2 (0.7–111.1 months) to ensure funduscopic tumor control. Kaplan–Meier estimates calculated a risk for cataract of 74.3 % after 5 years. There was no increase in metastasis or local recurrence in these patients. Patient’s age was the sole independent statistically significant risk factor for cataract development. The probability of cataract occurrence significantly increased with doses to lens exceeding 15–20 CGE. Neither the appearance of cataract nor cataract surgery influenced long-term visual outcome.
Conclusion
Cataract formation is the most frequent complication after irradiation. There is no benefit vis-a-vis brachytherapy with regard to cataract development. Data indicate a dose–effect threshold of 0.5 CGE for cataractogenesis, with significantly increasing risk above a dose of 15 CGE. Furthermore, cataract surgery can be performed without an increased risk for metastasis.

Similar content being viewed by others
References
Collaborative Ocular Melanoma Study Group (2007) Incidence of cataract and outcomes after cataract surgery in the first 5 years after iodine 125 brachytherapy in the Collaborative Ocular Melanoma Study: COMS Report No 27. Ophthalmology 114(7):1363–1371
Ainsbury EA, Bouffler SD, Dörr W et al (2009) Radiation cataractogenesis: a review of recent studies. Radiat Res 172(1):1–9. doi:10.1667/RR1688.1
Kleineidam M, Augsburger JJ, Hernandez C et al (1993) Cataractogenesis after Cobalt-60 eye plaque radiotherapy. Int J Radiat Oncol Biol Phys 26:625–630. doi:10.1016/0360-3016(93)90279-5
Summanen P, Immonen I, Kivela T et al (1996) Radiation related complications after ruthenium plaque radiotherapy of uveal melanoma. Br J Ophthalmol 80(8):732–739. doi:10.1136/bjo.80.8.732
Gündüz K, Shields CL, Shields JA et al (1999) Radiation complications and tumor control after plaque radiotherapy of uveal melanoma with macular involvement. Am J Opthalmol 127(5):579–589. doi:10.1016/S0002-9394(98)00445-0
Shields CL, Cater J, Shields JA et al (2002) Combined plaque radiotherapy and transpupillary thermotherapy for choroidal melanoma: tumor control and treatment complications in 270 consecutive patients. Arch Ophthalmol 120(7):933–940. doi:10.1001/archopht.120.7.933
Gündüz K, Shields CL, Shields JA et al (1999) Plaque radiotherapy of uveal melanoma with predominant ciliary body involvement. Arch Ophthalmol 117(2):170–177. doi:10.1001/archopht.117.2.170
Brovkina AF, Zarubei GD (1986) Ciliochoroidal melanomas treated with a narrow medical proton beam. Arch Ophthalmol 104(3):402–404. doi:10.1001/archopht.1986.01050150102037
Gragoudas ES, Egan KM, Arrigg PG et al (1992) Cataract extraction after proton beam irradiation for malignant melanoma of the eye. Arch Ophthalmol 110(4):475–479. doi:10.1001/archopht.1992.01080160053029
Emami B, Lyman J, Brown A, Coia L, Goitein M, Munzenrider JE, Shank B, Solin LJ, Wesson M (1991) Tolerance of normal tissue to therapeutic irradiation. Int J Radiat Oncol Biol Phys 21(1):109–122. doi:10.1016/0360-3016(91)90171-Y
Puusaari I, Heikkonen J, Kivela T (2004) Effect of radiation dose on ocular complications after iodine brachytherapy for large uveal melanoma: empirical data and simulation of collimating plaques. Invest Ophthalmol Vis Sci 45(10):3425–3434. doi:10.1167/iovs.04-0066
Congdon NG, Taylor HR (2003) Age-related cataract. In: Johnson GJ, Minassian DC, Weale RA, West SK (eds) The epidemiology of eye disease. Arnold, London, pp 105–119
Reichstein D (2015) Current treatments and preventive strategies for radiation retinopathy. Curr Opin Ophthalmol 26(3):157–166. doi:10.1097/ICU.0000000000000141
James ER (2007) The etiology of steroid cataract. J Ocul Pharmacol Ther 23(5):403–420. doi:10.1089/jop.2006.0067
ICRP (1990) Recommendations of the International Commission on Radiological Protection. Publication 60, Annals of the ICRP, Vol. 21. Elsevier, Amsterdam
ICRP (2007) The 2007 Recommendations of the International Commission on Radiological Protection. Publication 103, Annals of the ICRP, Vol. 37. Elsevier, Amsterdam
Chumak VV, Worgul BV, Kundiyev YI et al (2007) Dosimetry for a study of low-dose radiation cataracts among Chernobyl clean-up workers. Radiat Res 167(5):606–614. doi:10.1667/RR0302.1
Worgul BV, Kundiyev YI, Sergiyenko NM et al (2007) Cataracts among Chernobyl clean-up workers: implications regarding permissible eye exposures. Radiat Res 167(2):233–243. doi:10.1667/RR0298.1
Hall P, Granath F, Lundell M et al (1999) Lenticular opacities in individuals exposed to ionizing radiation in infancy. Radiat Res 152(2):190–195. doi:10.2307/3580093
Nakashima E, Neriishi K, Minamoto A (2006) A reanalysis of atomic-bomb cataract data,2000-2002, a threshold analysis. Health Phys 90(2):154–160. doi:10.1097/01.HP.0000175442.03596.63
Seibel I, Cordini D, Rehak M et al (2015) Local recurrence after primary proton beam therapy in uveal melanoma: risk factors, retreatment approaches, and outcome. Am J Ophthalmol 160(4):628–636. doi:10.1016/j.ajo.2015.06.017
Acknowledgments
Statistical analysis was performed by Dr. Ulrich Gauger, medical statistician, Berlin, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research
Conflict of interest
Prof. Dr. A. M. Joussen and PD Dr. M. Rehak report personal fees from Bayer, personal fees from Novartis, and personal fees from Allergan, outside the submitted work. All other authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Seibel, I., Cordini, D., Hager, A. et al. Cataract development in patients treated with proton beam therapy for uveal melanoma. Graefes Arch Clin Exp Ophthalmol 254, 1625–1630 (2016). https://doi.org/10.1007/s00417-016-3356-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3356-4