Abstract
Purpose
To report on the safety and efficacy of Nd: YAG laser goniopuncture (LGP) for postsurgical intraocular pressure increase after deep sclerectomy (DS) in a consecutive cohort of open-angle glaucoma patients.
Methods
This case series included 56 eyes from 49 consecutive patients who underwent LGP between November 2008 and March 2015. Prior to LGP, patients had undergone DS augmented with mitomycin C and injectable cross-linked hyaluronic acid implant between October 2008 and May 2014. Demographic variables, type of glaucoma, prior phacoemulsification, intraocular pressure (IOP), best-corrected visual acuity, execution of post-LGP maneuvres, and post-LGP complications were analyzed. The success rate of the procedure was analyzed using the Kaplan–Meier survival curve. Univariate and multivariate analyses were performed using the Cox proportional hazard regression model in order to highlight variables associated with a failure to achieve surgical success.
Results
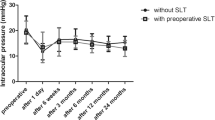
Mean IOP was 23.0 mmHg prior to LGP, and 12.5, 11.8, and 10.5 mmHg at 6, 12, and 24 months after LGP respectively. Post-laser IOP was significantly lower than pre-laser IOP at every time point. For an IOP ≤ 15 mmHg, success rates were 85 % at 6 months, 76 % at 1 year, and 62 % at 2 years. Thirty-eight eyes underwent prophylactic iridotomy and iridoplasty prior to LGP. Iris prolapse into the trabeculo-descemetic window following LGP occurred in 6/18 eyes (33.3 %) of the non-pretreated and in 1/38 eyes (2.6 %) of the pretreated group. One case of choroidal detachment and one delayed suprachoroidal hemorrhage occurred after LGP execution in two non-pretreated eyes.
Conclusions
LGP is a relatively safe and effective complementary adjunct to deep sclerectomy that makes it possible to further lower IOP and avoid additional filtering surgery. Prophylactic iridotomy and localized iridoplasty may permit the frequency of post-LGP complications to be reduced.


Similar content being viewed by others
References
El Sayyad F, Helal M, El-Kholify M, Khalil M, El-Maghraby A (2000) Nonpenetrating deep sclerectomy versus trabeculectomy in bilateral primary open-angle glaucoma. Ophthalmology 107:1671–1674
Carassa RG, Bettin P, Fiori M, Brancato R (2003) Viscocanalostomy versus trabeculectomy in white adults affected by open-angle glaucoma: a 2-year randomized, controlled trial. Ophthalmology 110:882–887
Eldaly MA, Bunce C, Elsheikha OZ, Wormald R (2014) Non-penetrating filtration surgery versus trabeculectomy for open-angle glaucoma. Cochrane Database Syst Rev 2, CD007059
Roy S, Mermoud A (2012) Deep sclerectomy. Dev Ophthalmol 50:29–36
Kozobolis VP, Christodoulakis EV, Tzanakis N, Zacharopoulos I, Pallikaris IG (2002) Primary deep sclerectomy versus primary deep sclerectomy with the use of mitomycin C in primary open-angle glaucoma. J Glaucoma 11:287–293
Neudorfer M, Sadetzki S, Anisimova S, Geyer O (2004) Nonpenetrating deep sclerectomy with the use of adjunctive mitomycin C. Ophthalmic Surg Lasers Imaging 35:6–12
Bettin P, Di Matteo F, Rabiolo A, Fiori M, Ciampi C, Bandello F (2015) Deep sclerectomy with mitomycin C and injectable cross-linked hyaluronic acid implant: long-term results. J Glaucoma [Epub ahead of print]
Koukkoulli A, Musa F, Anand N (2015) Long-term outcomes of needle revision of failing deep sclerectomy blebs. Graefes Arch Clin Exp Ophthalmol 253:99–106
Bettin P (2012) Postoperative management of penetrating and nonpenetrating external filtering procedures. Dev Ophthalmol 50:48–63
Mermoud A, Karlen ME, Schnyder CC et al (1999) Nd:Yag goniopuncture after deep sclerectomy with collagen implant. Ophthalmic Surg Lasers 30:120–125
Tam DY, Barnebey HS, Ahmed II (2013) Nd: YAG laser goniopuncture: indications and procedure. J Glaucoma 22:620–625
Vuori ML (2003) Complications of neodymium:YAG laser goniopuncture after deep sclerectomy. Acta Ophthalmol Scand 81:573–576
Anand N, Pilling R (2010) Nd:YAG laser goniopuncture after deep sclerectomy: outcomes. Acta Ophthalmol 88:110–115
Mendrinos E, Mermoud A, Shaarawy T (2008) Nonpenetrating glaucoma surgery. Surv Ophthalmol 53:592–630
Rabiolo A, Bettin P, Fiori M, Ciampi C, Di Matteo F, Bandello F (2015) Delayed suprachoroidal hemorrhage following Nd:YAG laser goniopuncture: a case report. Eur J Ophthalmol 25:e40–e41
Kim CY, Hong YJ, Seong GJ, Koh HJ, Kim SS (2002) Iris synechia after laser goniopuncture in a patient having deep sclerectomy with a collagen implant. J Cataract Refract Surg 28:900–902
Anand N, Atherley C (2005) Deep sclerectomy augmented with mitomycin C. Eye (Lond) 19:442–450
Anand N, Kumar A, Gupta A (2011) Primary phakic deep sclerectomy augmented with mitomycin C: long-term outcomes. J Glaucoma 20:21–27
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
For this type of study, formal consent is not required.
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge, or beliefs) in the subject matter or materials discussed in this manuscript.
Rights and permissions
About this article
Cite this article
Di Matteo, F., Bettin, P., Fiori, M. et al. Nd:Yag laser goniopuncture for deep sclerectomy: efficacy and outcomes. Graefes Arch Clin Exp Ophthalmol 254, 535–539 (2016). https://doi.org/10.1007/s00417-016-3271-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-016-3271-8