Abstract
Background
Studies showed the impact of sex and onset site (spinal or bulbar) on disease onset and survival in ALS. However, they mainly result from cross-sectional or survival analysis, and the interaction of sex and onset site on the different proxies of disease trajectory has not been fully investigated.
Methods
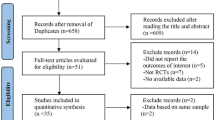
We selected all patients with repeated observations in the PRO-ACT database. We divided them into four groups depending on their sex and onset site. We estimated a multivariate disease progression model, named ALS Course Map, to investigate the combined temporal changes of the four sub-scores of the revised ALS functional rating scale (ALSFRSr), the forced vital capacity (FVC), and the body mass index (BMI). We then compared the progression rate, the estimated age at onset, and the relative progression of the outcomes across each group.
Results
We included 1438 patients from the PRO-ACT database. They were 51% men with spinal onset, 12% men with bulbar onset, 26% women with spinal onset, and 11% women with bulbar onset. We showed a significant influence of both sex and onset site on the ALSFRSr progression. The BMI decreased 8.9 months earlier (95% CI [3.9, 13.8]) in women than men, after correction for the onset site. Among patients with bulbar onset, FVC was impaired 2.6 months earlier (95% CI [0.6, 4.6]) in women.
Conclusion
Using a multivariable disease modelling approach, we showed that sex and onset site are important drivers of the progression of motor function, BMI, and FVC decline.



Similar content being viewed by others
References
Rowland LP, Shneider NA (2001) Amyotrophic lateral sclerosis. N Engl J Med 344(22):1688–1700. https://doi.org/10.1056/NEJM200105313442207
Talbott EO, Malek AM, Lacomis D (2016) The epidemiology of amyotrophic lateral sclerosis. Handb Clin Neurol 138:225–238. https://doi.org/10.1016/B978-0-12-802973-2.00013-6
Swinnen B, Robberecht W (2014) The phenotypic variability of amyotrophic lateral sclerosis. Nat Rev Neurol 10(11):661–670. https://doi.org/10.1038/nrneurol.2014.184
Tysnes OB, Vollset SE, Aarli JA (1991) Epidemiology of amyotrophic lateral sclerosis in Hordaland county, western Norway. Acta Neurol Scand 83(5):280–285. https://doi.org/10.1111/j.1600-0404.1991.tb04701.x
Brown RH, Al-Chalabi A (2017) Amyotrophic lateral sclerosis. N Engl J Med 377(2):162–172. https://doi.org/10.1056/NEJMra1603471
Brooks BR (1996) Natural history of ALS: symptoms, strength, pulmonary function, and disability. Neurology 47(4):S71-81. https://doi.org/10.1212/wnl.47.4_suppl_2.71s
Logroscino G, Traynor BJ, Hardiman O et al (2010) Incidence of amyotrophic lateral sclerosis in Europe. J Neurol Neurosurg Psychiatry 81(4):385–390. https://doi.org/10.1136/jnnp.2009.183525
Chiò A, Moglia C, Canosa A et al (2020) ALS phenotype is influenced by age, sex, and genetics: a population-based study. Neurology 94(8):e802–e810. https://doi.org/10.1212/WNL.0000000000008869
F T, G D, S B, G T. (2020) Genetics and sex in the pathogenesis of amyotrophic lateral sclerosis (ALS): is there a link? Int J Mol Sci 21:10. https://doi.org/10.3390/ijms21103647
Bede P, Elamin M, Byrne S, Hardiman O (2014) Sexual dimorphism in ALS: exploring gender-specific neuroimaging signatures. Amyotroph Lateral Scler Front Degener 15(3–4):235–243. https://doi.org/10.3109/21678421.2013.865749
Farrington DP (1991) Longitudinal research strategies: advantages, problems, and prospects. J Am Acad Child Adolesc Psychiatry 30(3):369–374. https://doi.org/10.1097/00004583-199105000-00003
Moglia C, Calvo A, Grassano M et al (2019) Early weight loss in amyotrophic lateral sclerosis: outcome relevance and clinical correlates in a population-based cohort. J Neurol Neurosurg Psychiatry 90(6):666–673. https://doi.org/10.1136/jnnp-2018-319611
Daghlas SA, Govindarajan R, Pooled Resource Open-Access ALS Clinical Trials Consortium (2021) Relative effects of forced vital capacity and ALSFRS-R on survival in ALS. Muscle Nerve 64(3):346–351. https://doi.org/10.1002/mus.27344
Rooney J, Burke T, Vajda A, Heverin M, Hardiman O (2017) What does the ALSFRS-R really measure? A longitudinal and survival analysis of functional dimension subscores in amyotrophic lateral sclerosis. J Neurol Neurosurg Psychiatry 88(5):381–385. https://doi.org/10.1136/jnnp-2016-314661
Schiratti JB, Allassonnière S, Colliot O, Durrleman S (2017) A Bayesian mixed-effects model to learn trajectories of changes from repeated manifold-valued observations
Schiratti JB, Allassonniere S, Colliot O, Durrleman S (2015) Learning spatiotemporal trajectories from manifold-valued longitudinal data
Atassi N, Berry J, Shui A et al (2014) The PRO-ACT database: design, initial analyses, and predictive features. Neurology 83(19):1719–1725. https://doi.org/10.1212/WNL.0000000000000951
Brändli O, Schindler C, Künzli N, Keller R, Perruchoud AP (1996) Lung function in healthy never smoking adults: reference values and lower limits of normal of a Swiss population. Thorax 51(3):277–283. https://doi.org/10.1136/thx.51.3.277
Pedregosa F, Varoquaux G, Gramfort A et al (2023) Scikit-learn: machine learning in python. Mach Learn Python 6:2
Yeo I, Johnson RA (2000) A new family of power transformations to improve normality or symmetry. Biometrika 87(4):954–959. https://doi.org/10.1093/biomet/87.4.954
Box GEP, Cox DR (1964) An analysis of transformations. J R Stat Soc Ser B Methodol 26(2):211–252
Fang T, Al Khleifat A, Stahl DR et al (2017) Comparison of the King’s and MiToS staging systems for ALS. Amyotroph Lateral Scler Front Degener 18(3–4):227–232. https://doi.org/10.1080/21678421.2016.1265565
Thakore NJ, Lapin BR, Kinzy TG, Pioro EP (2018) Deconstructing progression of amyotrophic lateral sclerosis in stages: a Markov modeling approach. Amyotroph Lateral Scler Front Degener 19(7–8):483–494. https://doi.org/10.1080/21678421.2018.1484925
Couronne R, Vidailhet M, Corvol JC, Lehericy S, Durrleman S. Learning disease progression models with longitudinal data and missing values. In: 2019 IEEE 16th International Symposium on Biomedical Imaging (ISBI 2019). IEEE; 2019:1033–1037. doi:https://doi.org/10.1109/ISBI.2019.8759198
Koval I, Bône A, Louis M et al (2021) AD course map charts Alzheimer’s disease progression. Sci Rep 11(1):8020. https://doi.org/10.1038/s41598-021-87434-1
Couronné R (2021) Progression models for Parkinson’s Disease. Published online 194
Tukey JW (1949) Comparing individual means in the analysis of variance. Biometrics 5(2):99–114. https://doi.org/10.2307/3001913
Skipper S, Perktold J (2010) Statsmodels: Econometric and statistical modeling with python. Published online
Bedre R (2020) reneshbedre/bioinfokit: Bioinformatics data analysis and visualization toolkit. Published online
Peter RS, Rosenbohm A, Dupuis L et al (2017) Life course body mass index and risk and prognosis of amyotrophic lateral sclerosis: results from the ALS registry Swabia. Eur J Epidemiol 32(10):901–908. https://doi.org/10.1007/s10654-017-0318-z
Li JY, Sun XH, Cai ZY et al (2022) Correlation of weight and body composition with disease progression rate in patients with amyotrophic lateral sclerosis. Sci Rep 12(1):13292. https://doi.org/10.1038/s41598-022-16229-9
Nakamura R, Kurihara M, Ogawa N et al (2022) Investigation of the prognostic predictive value of serum lipid profiles in amyotrophic lateral sclerosis: roles of sex and hypermetabolism. Sci Rep 12(1):1826. https://doi.org/10.1038/s41598-022-05714-w
Dupuis L, Pradat PF, Ludolph AC, Loeffler JP (2011) Energy metabolism in amyotrophic lateral sclerosis. Lancet Neurol 10(1):75–82. https://doi.org/10.1016/S1474-4422(10)70224-6
Nelson AT, Trotti D (2022) Altered bioenergetics and metabolic homeostasis in amyotrophic lateral sclerosis. Neurother J Am Soc Exp Neurother 19(4):1102–1118. https://doi.org/10.1007/s13311-022-01262-3
Vandoorne T, De Bock K, Van Den Bosch L (2018) Energy metabolism in ALS: an underappreciated opportunity? Acta Neuropathol (Berl) 135(4):489–509. https://doi.org/10.1007/s00401-018-1835-x
Guillot SJ, Bolborea M, Dupuis L (2021) Dysregulation of energy homeostasis in amyotrophic lateral sclerosis. Curr Opin Neurol 34(5):773–780. https://doi.org/10.1097/WCO.0000000000000982
Blaak E (2001) Gender differences in fat metabolism. Curr Opin Clin Nutr Metab Care 4(6):499–502. https://doi.org/10.1097/00075197-200111000-00006
Toth MJ, Tchernof A, Sites CK, Poehlman ET (2000) Effect of menopausal status on body composition and abdominal fat distribution. Int J Obes Relat Metab Disord J Int Assoc Study Obes 24(2):226–231. https://doi.org/10.1038/sj.ijo.0801118
Lee I, Kazamel M, McPherson T et al (2021) Fat mass loss correlates with faster disease progression in amyotrophic lateral sclerosis patients: exploring the utility of dual-energy x-ray absorptiometry in a prospective study. PLoS ONE 16(5):e0251087. https://doi.org/10.1371/journal.pone.0251087
Morelot-Panzini C, Bruneteau G, Gonzalez-Bermejo J (2019) NIV in amyotrophic lateral sclerosis: the ‘when’ and ‘how’ of the matter. Respirology 24(6):521–530. https://doi.org/10.1111/resp.13525
Bede P, Murad A, Lope J, Hardiman O, Chang KM (2022) Clusters of anatomical disease-burden patterns in ALS: a data-driven approach confirms radiological subtypes. J Neurol 269(8):4404–4413. https://doi.org/10.1007/s00415-022-11081-3
Trojsi F, Di Nardo F, Caiazzo G et al (2021) Between-sex variability of resting state functional brain networks in amyotrophic lateral sclerosis (ALS). J Neural Transm Vienna Austria 128(12):1881–1897. https://doi.org/10.1007/s00702-021-02413-0
Lissek S, Hausmann M, Knossalla F et al (2007) Sex differences in cortical and subcortical recruitment during simple and complex motor control: An fMRI study. Neuroimage 37(3):912–926. https://doi.org/10.1016/j.neuroimage.2007.05.037
Lay K, Li G (2019) Do microglial sex differences contribute to sex differences in neurodegenerative diseases? Trends Mol Med 25(9):741–749. https://doi.org/10.1016/j.molmed.2019.05.001
Raymond J, Mehta P, Larson T, Pioro EP, Horton DK (2021) Reproductive history and age of onset for women diagnosed with amyotrophic lateral sclerosis: data from the national ALS registry: 2010–2018. Neuroepidemiology 55(5):416–424. https://doi.org/10.1159/000516344
Sumien N, Cunningham JT, Davis DL et al (2021) Neurodegenerative disease: roles for sex, hormones, and oxidative stress. Endocrinology 162(11):185. https://doi.org/10.1210/endocr/bqab185
Martin E, Cazenave W, Allain AE, Cattaert D, Branchereau P (2020) Implication of 5-HT in the dysregulation of chloride homeostasis in prenatal spinal motoneurons from the G93A mouse model of amyotrophic lateral sclerosis. Int J Mol Sci 21(3):1107. https://doi.org/10.3390/ijms21031107
Lulé DE, Müller HP, Finsel J et al (2020) Deficits in verbal fluency in presymptomatic C9orf72 mutation gene carriers—a developmental disorder. J Neurol Neurosurg Psychiatry 91(11):1195–1200. https://doi.org/10.1136/jnnp-2020-323671
Bertrand A, Wen J, Rinaldi D et al (2018) Early cognitive, structural, and microstructural changes in presymptomatic C9orf72 carriers younger than 40 years. JAMA Neurol 75(2):236–245. https://doi.org/10.1001/jamaneurol.2017.4266
Stephens MC, Brandt V, Botas J (2022) The developmental roots of neurodegeneration. Neuron 110(1):1–3. https://doi.org/10.1016/j.neuron.2021.12.004
Locascio JJ, Atri A (2011) An overview of longitudinal data analysis methods for neurological research. Dement Geriatr Cogn Disord Extra 1(1):330–357. https://doi.org/10.1159/000330228
Gordon PH, Cheng B, Salachas F et al (2010) Progression in ALS is not linear but is curvilinear. J Neurol 257(10):1713–1717. https://doi.org/10.1007/s00415-010-5609-1
Vasta R, D’Ovidio F, Canosa A et al (2020) Plateaus in amyotrophic lateral sclerosis progression: results from a population-based cohort. Eur J Neurol 27(8):1397–1404. https://doi.org/10.1111/ene.14287
Borghero G, Sechi MM, Vasta R et al (2023) Spatial clustering of amyotrophic lateral sclerosis in Sardinia, Italy: the contribution of age, sex, and genetic factors. Muscle Nerve. https://doi.org/10.1002/mus.27939
Trojsi F, Sagnelli A, Vanacore N et al (2012) Clinical features and lifestyle of patients with amyotrophic lateral sclerosis in Campania: brief overview of an Italian database. Ann Ist Super Sanita 48(3):287–291. https://doi.org/10.4415/ANN_12_03_09
Westeneng HJ, van Veenhuijzen K, van der Spek RA et al (2021) Associations between lifestyle and amyotrophic lateral sclerosis stratified by C9orf72 genotype: a longitudinal, population-based, case-control study. Lancet Neurol 20(5):373–384. https://doi.org/10.1016/S1474-4422(21)00042-9
Acknowledgements
We warmly thank Igor Koval for the review of the data processing and all the team members of ARAMIS for their input and advice.
Funding
This paper is funded in part by grant number 826421 (TVB-Cloud) from the H2020 program, and ANR-10-IAIHU-06 (IHU ICM), ANR-19-P3IA-0001 (PRAIRIE 3IA Institute), and ANR-19-JPW2-000 (E-DADS) from ANR.
Author information
Authors and Affiliations
Contributions
JO contributed to drafting/revision of the manuscript for content, including medical writing for content; study concept or design; and analysis or interpretation of data. P-FP performed drafting/revision of the manuscript for content, including medical writing for content; STdM contributed to drafting/revision of the manuscript for content, including medical writing for content; study concept or design; and analysis or interpretation of data. SD contributed to drafting/revision of the manuscript for content, including medical writing for content; study concept or design; and analysis or interpretation of data.
Corresponding author
Ethics declarations
Conflicts of interest
The authors report no relevant disclosures.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ortholand, J., Pradat, PF., Tezenas du Montcel, S. et al. Interaction of sex and onset site on the disease trajectory of amyotrophic lateral sclerosis. J Neurol 270, 5903–5912 (2023). https://doi.org/10.1007/s00415-023-11932-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-023-11932-7