Abstract
Background
Freezing of gait (FOG) is one of the most disabling gait disorders affecting 80% of patients with Parkinson’s disease (PD). Clinical guidelines recommend a behavioral approach for gait rehabilitation, but there is a wide diversity of behavioral modalities.
Objective
The objective of this network meta-analysis was to compare the effectiveness of different behavioral interventions for FOG management in PD patients.
Methods
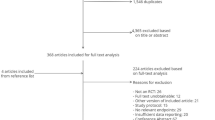
Six databases were searched for randomized controlled trials of behavioral interventions for FOG management among PD patients from 1990 to December 2021. Bayesian network meta-analysis was used to combine both direct and indirect trial evidence on treatment effectiveness, while the surface under the cumulative ranking (SUCRA) score was used to estimate the ranked probability of intervention effectiveness.
Results
Forty-six studies were included in the qualitative synthesis. Among, 36 studies (1454 patients) of 72 interventions or control conditions (12 classes) were included in the network meta-analysis, with a mean intervention period of 10.3 weeks. After adjusting for the moderating effect of baseline FOG severity, obstacle training [SMD −2.1; 95% credible interval (Crl): −3.3, −0.86], gait training with treadmill (SMD −1.2; 95% Crl: −2.0, −0.34), action observation training (SMD −1.0; 95% Crl: −1.9, −0.14), conventional physiotherapy (SMD −0.70; 95% Crl: −1.3, −0.12) and general exercise (SMD −0.64; 95% Crl: −1.2, −0.11) demonstrated significant improvement on immediate FOG severity compared to usual care. The SUCRA rankings suggest that obstacle training, gait training on treadmill and general exercises are most likely to reduce FOG severity.
Conclusion
Obstacle training, gait training on treadmill, general exercises, action observation training and conventional physiotherapy demonstrated immediate real-life benefits on FOG symptoms among patients with mild–moderate PD. With the promising findings, the sustained effects of high complexity motor training combined with attentional/cognitive strategy should be further explored. Future trials with rigorous research designs using both subjective and objective outcome measures, long-term follow-up and cost-effective analysis are warranted to establish effective behavioral strategies for FOG management.





Similar content being viewed by others
Change history
05 April 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00415-022-11076-0
References
Gilat M et al (2018) Freezing of gait: promising avenues for future treatment. Parkinsonism Relat Disord 52:7–16
Mahoney JR et al (2016) The role of prefrontal cortex during postural control in Parkinsonian syndromes a functional near-infrared spectroscopy study. Brain Res 1633:126–138
Gilat M et al (2021) A systematic review on exercise and training-based interventions for freezing of gait in Parkinson’s disease. NPJ Parkinson’s Dis 7(1):81
Nonnekes J et al (2019) Compensation strategies for gait impairments in Parkinson disease: a review. JAMA Neurol 76(6):718–725
Cosentino C et al (2020) Effectiveness of physiotherapy on freezing of gait in Parkinson’s disease: a systematic review and meta-analyses. Mov Disord 35(4):523–536
Mak MK et al (2017) Long-term effects of exercise and physical therapy in people with Parkinson disease. Nat Rev Neurol 13(11):689–703
Kwok JYY, Choi KC, Chan HYL (2016) Effects of mind–body exercises on the physiological and psychosocial well-being of individuals with Parkinson’s disease: a systematic review and meta-analysis. Complement Ther Med 29:121–131
Walton CC et al (2014) Freezing of gait in Parkinson’s disease: current treatments and the potential role for cognitive training. Restor Neurol Neurosci 32(3):411–422
Rouse B, Chaimani A, Li T (2017) Network meta-analysis: an introduction for clinicians. Intern Emerg Med 12(1):103–111
Hutton B et al (2015) The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med 162(11):777–784
Ou R et al (2018) Predictors of freezing of gait in Chinese patients with Parkinson’s disease. Brain Behav 8(3):e00931
Sterne JAC et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898
Brignardello-Petersen R et al (2018) Advances in the GRADE approach to rate the certainty in estimates from a network meta-analysis. J Clin Epidemiol 93:36–44
Giladi N et al (2009) Validation of the freezing of gait questionnaire in patients with Parkinson’s disease. Mov Disord 24(5):655–661
Giladi N et al (2000) Construction of freezing of gait questionnaire for patients with Parkinsonism. Parkinsonism Relat Disord 6(3):165–170
Nieuwboer A et al (2009) Reliability of the new freezing of gait questionnaire: agreement between patients with Parkinson’s disease and their carers. Gait Posture 30(4):459–463
Higgins JPT et al (2019) Cochrane handbook for systematic reviews of interventions, 2nd edn. Wiley, Chichester
Capecci M et al (2019) Clinical effects of robot-assisted gait training and treadmill training for Parkinson’s disease. A randomized controlled trial. Ann Phys Rehabil Med 62(5):303–312
Medijainen K et al (2019) Versatile guideline-based physiotherapy intervention in groups to improve gait speed in Parkinson’s disease patients. NeuroRehabilitation 44(4):579–586
Paul SS et al (2014) Leg muscle power is enhanced by training in people with Parkinson’s disease: a randomized controlled trial. Clin Rehabil 28(3):275–288
Franchini AJ et al (2012) Accounting for correlation in network meta-analysis with multi-arm trials. Res Synth Methods 3(2):142–160
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558
Dias S et al (2018) Network meta-analysis for decision-making, 1st edn. Wiley, Newark
King LA et al (2020) Cognitively challenging agility boot camp program for freezing of gait in Parkinson disease. Neurorehabil Neural Repair 34(5):417–427
Mezzarobba S et al (2018) Action observation plus sonification. A novel therapeutic protocol for Parkinson’s patient with freezing of gait. Front Neurol 8:723–723
Canning CG et al (2015) Exercise for falls prevention in Parkinson disease: a randomized controlled trial. Neurology 84(3):304–312
Volpe D et al (2013) A comparison of Irish set dancing and exercises for people with Parkinson’s disease: a phase II feasibility study. BMC Geriatr 13:1–6
Bekkers EMJ et al (2020) Do patients with Parkinson’s disease with freezing of gait respond differently than those without to treadmill training augmented by virtual reality? Neurorehabil Neural Repair 34(5):440–449
King LA et al (2015) Effects of group, individual, and home exercise in persons with Parkinson disease: a randomized clinical trial. J Neurol Phys Ther 39(4):204–212
Clerici I et al (2019) Land plus aquatic therapy versus land-based rehabilitation alone for the treatment of freezing of gait in Parkinson disease: a randomized controlled trial. Phys Ther 99(5):591–600
Bultitude JH et al (2021) Two weeks of twice-daily prism adaptation treatment does not improve posture or gait in Parkinson’s disease: a double-blind randomized controlled trial. Trials 22(1):846
Schlenstedt C et al (2018) Moderate frequency resistance and balance training do not improve freezing of gait in Parkinson’s disease: a pilot study. Front Neurol 9:1084–1084
Rocha P et al (2018) Dance therapy for Parkinson’s disease: a randomised feasibility trial. Int J Ther Rehabil 25(2):64–72
Duncan RP, Earhart GM (2012) Randomized controlled trial of community-based dancing to modify disease progression in Parkinson disease. Neurorehabil Neural Repair 26(2):132–143
Duncan RP, Earhart GM (2014) Are the effects of community-based dance on Parkinson disease severity, balance, and functional mobility reduced with time? A 2-year prospective pilot study. J Altern Complement Med 20(10):757–763
Keus S et al (2014) European physiotherapy guideline for Parkinson’s disease. KNGF/ParkinsonNet, Nijmegen
Cheng FY et al (2017) Effects of curved-walking training on curved-walking performance and freezing of gait in individuals with Parkinson’s disease: a randomized controlled trial. Parkinsonism Relat Disord 43:20–26
Frazzitta G et al (2009) Rehabilitation treatment of gait in patients with Parkinson’s disease with freezing: a comparison between two physical therapy protocols using visual and auditory cues with or without treadmill training. Mov Disord 24(8):1139–1143
Ginis P et al (2016) Feasibility and effects of home-based smartphone-delivered automated feedback training for gait in people with Parkinson’s disease: A pilot randomized controlled trial. Parkinsonism Relat Disord 22:28–34
Nieuwboer A et al (2007) Cueing training in the home improves gait-related mobility in Parkinson’s disease: the RESCUE trial. J Neurol Neurosurg Psychiatry 78(2):134–140
Pelosin E et al (2010) Action observation improves freezing of gait in patients with Parkinson’s disease. Neurorehabil Neural Repair 24(8):746–752
Romenets RS et al (2015) Tango for treatment of motor and non-motor manifestations in Parkinson’s disease: a randomized control study. Complement Ther Med. 23(2):175–184
Tremblay MS et al (2017) Sedentary Behavior Research Network (SBRN)—terminology consensus project process and outcome. Int J Behav Nutr Phys Act 14(1):75
Yang YR et al (2019) Cognitive and motor dual task gait training exerted specific training effects on dual task gait performance in individuals with Parkinson’s disease: a randomized controlled pilot study. PLoS ONE 14(6):e0218180
Zhu Z et al (2018) Aquatic obstacle training improves freezing of gait in Parkinson’s disease patients: a randomized controlled trial. Clin Rehabil 32(1):29–36
Carroll LM et al (2017) Aquatic exercise therapy for people with Parkinson disease: a randomized controlled trial. Arch Phys Med Rehabil 98(4):631–638
Fietzek UM et al (2014) Randomized cross-over trial to investigate the efficacy of a two-week physiotherapy programme with repetitive exercises of cueing to reduce the severity of freezing of gait in patients with Parkinson’s disease. Clin Rehabil 28(9):902–911
Hackney ME et al (2007) Effects of tango on functional mobility in Parkinson’s disease: a preliminary study. J Neurol Phys Ther 31(4):173–179
Hackney ME, Earhart GM (2009) Effects of dance on movement control in Parkinson’s disease: a comparison of Argentine Tango and American Ballroom. J Rehabil Med 41(6):475–481
Harro CC et al (2014) The effects of speed-dependent treadmill training and rhythmic auditory-cued overground walking on balance function, fall incidence, and quality of life in individuals with idiopathic Parkinson’s disease: a randomized controlled trial. NeuroRehabilitation 34(3):541–556
Martin T et al (2015) A randomized controlled feasibility trial of a specific cueing program for falls management in persons with Parkinson disease and freezing of gait. J Neurol Phys Ther 39(3):179–184
Pelosin E et al (2018) Effect of group-based rehabilitation combining action observation with physiotherapy on freezing of gait in Parkinson’s disease. Neural Plast 2018:1–7
Santos L et al (2017) Effects of supervised slackline training on postural instability, freezing of gait, and falls efficacy in people with Parkinson’s disease. Disabil Rehabil 39(16):1573–1580
Schlick C et al (2015) Visual cues combined with treadmill training to improve gait performance in Parkinson’s disease: a pilot randomized controlled trial. Clin Rehabil 30(5):463–471
Wroblewska A et al (2019) The therapeutic effect of nordic walking on freezing of gait in Parkinson’s disease: a pilot study. Parkinsons Dis 2019:3846279
Xiao CM, Zhuang YC (2016) Effect of health Baduanjin Qigong for mild to moderate Parkinson’s disease. Geriatr Gerontol Int 16(8):911–919
Hubble RP et al (2019) Trunk exercises improve balance in Parkinson disease: a phase II randomized controlled trial. J Neurol Phys Ther 43(2):96–105
Ghielen I et al (2017) Body awareness training in the treatment of wearing-off related anxiety in patients with Parkinson’s disease: results from a pilot randomized controlled trial. J Psychosom Res 103:1–8
Carpinella I et al (2017) Wearable sensor-based biofeedback training for balance and gait in Parkinson disease: a pilot randomized controlled trial. Arch Phys Med Rehabil 98(4):622–630
Song J et al (2018) Home-based step training using videogame technology in people with Parkinson’s disease: a single-blinded randomised controlled trial. Clin Rehabil 32(3):299–311
Silva-Batista C et al (2020) A randomized, controlled trial of exercise for Parkinsonian individuals with freezing of gait. Mov Disord 35(9):1607–1617
Radder DLM et al (2020) Physiotherapy in Parkinson’s disease: a meta-analysis of present treatment modalities. Neurorehabil Neural Repair 34(10):871–880
Frenkel-Toledo S et al (2005) Treadmill walking as an external pacemaker to improve gait rhythm and stability in Parkinson’s disease. Mov Disord 20(9):1109–1114
Santos L et al (2017) Effects of progressive resistance exercise in akinetic-rigid Parkinson’s disease patients: a randomized controlled trial. Eur J Phys Rehabil Med 53(5):651–663
Kalyani HH et al (2020) Dance improves symptoms, functional mobility and fine manual dexterity in people with Parkinson disease: a quasi-experimental controlled efficacy study. Eur J Phys Rehabil Med 56(5):563–574
Cassimatis C et al (2016) The effectiveness of external sensory cues in improving functional performance in individuals with Parkinson’s disease: a systematic review with meta-analysis. Int J Rehabil Res 39(3):211–218
Allen NE et al (2010) The effects of an exercise program on fall risk factors in people with Parkinson’s disease: a randomized controlled trial. Mov Disord 25(9):1217–1225
Sedaghati P et al (2018) Effects of Alexander-based corrective techniques on forward flexed posture, risk of fall, and fear of falling in idiopathic Parkinson′s disease. Arch Neurosci 5(2):e61274
Agosta F et al (2016) Brain plasticity in Parkinson’s disease with freezing of gait induced by action observation training. J Neurol 264(1):88–101
Kwok JYY et al (2019) Effects of mindfulness yoga vs stretching and resistance training exercises on anxiety and depression for people with Parkinson disease: a randomized clinical trial. JAMA Neurol 76(7):755–763
Pohl P et al (2020) Group-based music intervention in Parkinson’s disease—findings from a mixed-methods study. Clin Rehabil 34(4):533–544
Bega D et al (2016) Yoga versus resistance training in Parkinson’s disease: a 12-week pilot feasibility study. Mov Disord 30:S69–S70
Kwok JYY, Lee JJ, Choi EPH, Chau PH, Auyeung M (2022) Stay mindfully active during the coronavirus pandemic: a feasibility study of mHealth-delivered mindfulness yoga program for people with Parkinson’s disease. BMC Complement Med and Ther 22(1). https://doi.org/10.1186/s12906-022-03519-y
Van Puymbroeck M et al (2018) Functional Improvements in Parkinson’s disease following a randomized trial of yoga. Evid Complement Altern Med eCAM 2018:8516351
Cugusi L et al (2017) Nordic walking for the management of people with Parkinson disease: a systematic review. PM&R 9(11):1157–1166
Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: updated guidelines for reporting parallel group randomized trials. Ann Intern Med 152(11):726–732
Acknowledgments
The authors would like to extend our sincere gratitude and appreciation to our research assistants, Ms. Charis Ann Lai and Ms. Yuki Shum, for their dedicated assistance and contribution to this research paper. We would also like to thank the reviewers at the Journal of Neurology for their critical comments and valuable feedback that has much improved the paper.
Funding
This project was supported by the Seed Funding for Basic Research, The University of Hong Kong (201910159193).
Author information
Authors and Affiliations
Contributions
Dr. Kwok had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. JK: conceptualization (lead); data curation (lead); methodology (lead); writing—original draft preparation (lead); writing—review and editing (lead); funding acquisition (lead); project administration (lead). RS: conceptualization (eqal); data curation (equal); formal analysis (lead); methodology (equal); writing—original draft preparation (equal); writing—review and editing (equal); project administration (equal). LC: data curation (lead); methodology (equal); writing—original draft preparation (equal); writing—review and editing (equal). LL: data curation (equal). DF: conceptualization (eqal); methodology (equal); writing—review and editing (equal); project administration (equal); supervision (lead). EC: Writing—review and editing (supporting). KL: writing—review and editing (supporting). JJL: writing—review and editing (supporting). MA: conceptualization (supporting); methodology (supporting). BB: writing—review and editing (supporting); supervision (supporting).
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that this work was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. Kwok, Fong, Choi, Lok and Lee have received funding support as principal investigators of the Seed Funding for Basic Research, the University of Hong Kong, Research Grants Councils and the Food and Health Bureau from Hong Kong, respectively. Bloem has a consultancy role with respect to Michael J Fox Foundation, and is the secretary-elect of the International Parkinson and Movement Disorder Society. The views expressed are those of the author(s) and not necessarily those of funding/professional bodies and non-governmental organization.
Additional information
The original online version of this article was revised: Modifications have been made in the Affiliation, text, reference section and supplementary material. Full information regarding the corrections made can be found in the erratum/correction for this article.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kwok, J.Y.Y., Smith, R., Chan, L.M.L. et al. Managing freezing of gait in Parkinson’s disease: a systematic review and network meta-analysis. J Neurol 269, 3310–3324 (2022). https://doi.org/10.1007/s00415-022-11031-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-022-11031-z