Abstract
Purpose
This multicentric, retrospective study aimed to analyze the short-term safety and effectiveness of the mCLIP Partial Prosthesis.
Methods
Patients underwent tympanoplasty with implantation of a mCLIP Partial Prosthesis. Follow-up examination included ear microscopy and pure-tone audiometry to determine the post-operative pure tone average of the frequencies 0.5, 1, 2 and 3 kHz (PTA4). The post-operative PTA4 air bone gap (ABG) was used to evaluate the audiological outcome. A post-operative minimum and maximum follow-up period was not defined. Thus, the follow-up times of each study center were different, which resulted in different follow-up times for the audiological analysis and for adverse events (AE).
Results
72 (66 adults, 6 children) patients were implanted with the mCLIP Partial Prosthesis. 68 (62 adults, 6 children) patients underwent audiological examination; all 72 patients were examined for adverse events. All patients (N = 68): 72.1% of the patients showed a PTA4 ABG of ≤ 20 dB. Individual post-operative bone conduction (BC) PTA4 thresholds were stable in 67 patients. The mean post-operative follow-up time was 78 ± 46 days. Children (N = 6): 5 out of 6 children showed a PTA4 ABG of ≤ 20 dB. None of the children reported a BC PTA4 deterioration of > 10 dB HL after the implantation. The mean post-operative follow-up time was 101 ± 45 days. Adverse events (all patients, N = 72): 15 (14 adults, 1 child) patients had AEs (27 AEs and 2 Follow-Ups). The mean post-operative follow-up time was 375 days.
Conclusion
Clinical data show satisfactory audiological parameters after implantation of the mCLIP Partial Prosthesis. The prosthesis is safe and effective for implantation in children and adults.
Trial registration number
NCT05565339, 09 September 2022, retrospectively registered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Passive middle ear implants (PMEIs) are used to reconstruct the ossicular chain to improve hearing in patients. PMEIs are designed to replace the ossicles and restore mechanical sound transmission from the tympanic membrane to the oval window. In addition to alloplastic materials, PMEIs include metals (titanium, platinum, gold), plastics (polyamide, polyethylene), Teflon®, and ceramics (hydroxyapatite, oxide ceramic, carbon, calcium phosphate ceramic, glass ceramic) [1]. Titanium is easy to implant, has a low extrusion rate and good tissue compatibility [2], and provides good functional results [3]. Titanium PMEIs have been on the market since 1994 [4], and ossicular chain reconstruction is considered the standard surgical method for hearing restoration.
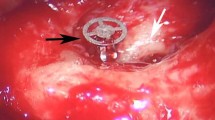
Our study provides results on patients implanted with the new mCLIP Partial Prosthesis (MED-EL, Innsbruck, Austria). The mCLIP Partial Prosthesis is made of titanium and was introduced to the market in August 2020 (Fig. 1).
mCLIP partial prosthesis design
The mCLIP Partial Prosthesis is made of medical titanium, grade 2. The head plate has a diameter of 2.6 mm and a thickness of 0.1 mm. The mCLIP Partial Prosthesis consists of 4 longer coupling structures with a length of 1.6 mm and 4 shorter coupling structures with a length of 1 mm. For the distance between the stapes head and the tympanic membrane, called functional length, is the prosthesis available from 0.75 – 3.5 mm and determines the 10 length versions of the prosthesis: 0.75, 1.0, 1.25, 1.5, 1.75, 2.0, 2.25, 2.5, 3.0, 3.5 mm (Fig. 1).
Material and methods
Ethical considerations
This study was conducted in Germany, Austria and Poland (Kajetany) in agreement with the Declaration of Helsinki 2013 and was approved by the relevant German, Austrian and Polish ethics committee(s) (Wels: 1257/2022, Erlangen: 456_20 Bc, Freiburg: 22–1142-retro, Göttingen: 1/9/20, Hannover: 9456_BO_S_2020, Lünen: 2020_829_b-S, Sankt Pölten; GS1-EK-4/777–2022, Warsaw: Oświadczenie nr. 11/2021r., AKH Wien: 2296/2021, Wiener Gesundheitsverbund, Klinik Landstraße: EK_23_005_XX, Linz: 1257/2022). The study is registered at ClinicalTrials.gov under NCT05565339.
Study design
This multicenter, retrospective follow-up study included 72 patients (72 ears), in which each patient served as his or her own control. All 72 patients were assessed for adverse events (AE); 4 of the 72 patients were excluded from the audiological analysis because of missing audiological data. For the analysis, patients implanted with the mCLIP Partial Prosthesis (regardless of implanted prosthesis length) until end of December 2022 were included.
Audiometric methods
Follow-up time
Patients were evaluated pre- and post-operatively (1 pre- and 1 post-operative audiological measurement). A post-operative minimum and maximum follow-up period was not specified. Therefore, follow-up times varied among study centers, resulting in different follow-up times for audiologic analysis and AE analysis. The mean post-operative follow-up time of all patients was calculated. Post-operative PTA was calculated as a four-frequency mean of 0.5, 1, 2, and 3 kHz (PTA4).
PTA4 ABG
Babighian et al. defined a post-operative PTA4 ABG of ≤ 20 dB as successful rehabilitation [1]. The minimum success rates found in the scientific literature for a titanium partial ossicular replacement prosthesis was reported by Quesnel et al. – 53.8% of the patients achieved a PTA4 ABG of ≤ 20 dB post-operatively [2]. Based on [1] and [2] a post-operative PTA4 ABG of ≤ 20 dB by ≥ 53.8% of the patients was considered a successful outcome four our study.
BC PTA4
The individual differences (Δ) between bone conduction (BC) post-operative and pre-operative PTA4 were calculated to determine safety of the procedure.
Adverse events (AE)
All surgical-, procedure- and device-related AEs in the operated ear that occurred intra- and post-operatively were collected.
General information
PTA4 ABG and adverse events were analysed descriptively. BC PTA4 was calculated inferentially. Graphs were created with GraphPad Prism 7 (GraphPad Software, Inc.).
Results
Demographics
All patients (N = 72)
The 72 patients (36 female, 36 male), including 6 children, were treated in four German (Erlangen, Freiburg, Göttingen, Hannover,) and one Austrian (Wels) clinic. The mean age was 45.5 ± 18.8 years (range: 9–81 years) at the time of implantation. 34 (47.2%) patients were implanted in the left ear and 38 (52.8%) in the right ear. 47 (65.3%) patients suffered from mixed hearing loss (MHL) and 25 (34.7%) from conductive hearing loss (CHL). The current etiologies that required implantation of the mCLIP Partial Prosthesis are listed in Table 1. In 39 (54.2%) cases it was not reported whether tympanoplasty sizers were used, in 25 (34.7%) cases no tympanoplasty sizer was used, in 8 (11.1%) cases tympanoplasty sizers were used (6 × MED-EL, 2 × brand was not reported).
Children (N = 6):
The 6 children (3 female, 3 male) had a mean age of 12.7 ± 2.4 years (range: 9–16 years) at the time of implantation. 4 out of 6 children were implanted in the left ear and 2 in the right ear. 3 children suffered from MHL and 3 from CHL. In 2 cases it was not reported whether a tympanoplasty sizer was used, in further 2 cases no tympanoplasty sizer was used, and in other 2 cases a MED-EL tympanoplasty sizer was used.
Audiometric results:
PTA4 ABG, all patients (N = 68):
The mean post-operative follow-up time was 78 ± 46 days (range: 3–302 days; median: 79 days). 49 (72.1%) of the 68 patients had a PTA4 ABG of ≤ 20 dB with a mean of 10.4 ± 4.4 dB (range: -0.3–19.8 dB; median: 11.0 dB) (95% CI (± e), min: 60.2%, max: 83.9%). Another 19 (27.9%) had a PTA4 ABG of > 20 dB, with a mean of 31.3 ± 7.5 dB (range: 21.3–50.5 dB; median: 29.5 dB) (Table 2). The mean post-operative PTA4 ABG of all 68 patients was 16.3 ± 10.9 dB. The first endpoint, improvement in post-operative PTA4 ABG of ≤ 20 dB by ≥ 53.8% of the patients was achieved. Figure 2 shows the PTA4 ABG results for all patients, as well as the pre- and post-operative AC and BC thresholds at the individual frequencies.
Post-operative AC and BC thresholds with the PTA4 ABG (N = 68). Left figure: circles = mean BC thresholds per frequency. Squares = mean AC thresholds per frequency; hatched area = ABG as difference between the results of AC and BC thresholds; mean post-operative BC PTA4 at 0.5/1/2/3 kHz = 14.8 ± 11.3/12.0 ± 14.3/23.4 ± 18.0/25.5 ± 18.4 dB HL. Mean post-operative AC PTA4 at 0.5/1/2/3 kHz = 33.4 ± 17.3/31.9 ± 18.7/32.6 ± 21.7/42.9 ± 21.9 dB HL. Right figure: PTA4 ABG as box plot: horizontal line = median; + = mean; circles = distribution of individual values; whiskers = maximum and minimum. PTA4 ABG: mean = 16.3 ± 10.9 dB; median = 13.0 dB
PTA4 ABG, children (< 18 years of age, N = 6):
The mean post-operative follow-up time was 101 ± 45 days (range: 57–179 days; median: 91 days). 5 out of 6 children had a PTA4 ABG of ≤ 20 dB (95% CI (± e), min: 36.4%, max: 100%). Patient 23 had a PTA4 ABG of 25.0 dB. The mean post-operative PTA4 ABG was 13.4 ± 6.4 dB.
BC PTA4 thresholds, all patients (N = 68):
-
The individual Δ BC PTA4thresholds were stable in 67 (98.5%) patients and within the fluctuation range of ± 5 dB HL. Patient 11 had a BC PTA4 deterioration of 16.3 dB HL after implantation (Table 2, Fig. 3).
-
Mean BC PTA4 thresholds (sum of all 68 patients): The mean pre-operative BC PTA4threshold was 21.4 ± 13.8 dB HL (range: – 3.8–64.3 dB HL) and the mean post-operative BC PTA4 threshold was 18.9 ± 13.9 dB HL (range: 1.3–65.3 dB HL) (Fig. 3).
Individual differences between pre- and post-operative BC thresholds with the BC PTA4 (N = 68). Pre-operative outcomes were compared with post-operative outcomes. + = mean; horizontal lines = median; circles = distribution of individual values; whiskers = maximum and minimum. BC PTA4 pre-/post-operative: mean = 21.4 ± 13.8/18.9 ± 13.9 dB HL
BC PTA4 thresholds, children (N = 6):
-
Individual BC PTA4 thresholds: None of the children had a BC PTA4 deterioration of > 10 dB HL after the implantation.
-
Mean BC PTA4 thresholds (sum of all 6 children): The mean pre-operative BC PTA4 threshold was 11.5 ± 5.9 dB HL (range: 7.0–22.0 dB HL) and the mean post-operative BC PTA4 threshold was 10.5 ± 5.5 dB HL (range: 5.0–19.0 dB HL).
Adverse events (AEs)
All patients (N = 72)
The mean post-operative follow-up time of the 72 patients was 368 ± 177 days (range: 0–666 days; median: 375 days). 15 (20.8%) of the 72 patients had AEs (27 AEs and 2 follow-ups).
One (1.4%) underage patient showed recurrent cholesteatoma; a revision surgery was performed and the mCLIP Partial Prosthesis was replaced with a total ossicular replacement prosthesis (patient 23). Another patient (1.4%) showed a prosthesis extrusion in combination with hearing reduction (patient 24) and was treated with a hearing aid. One patient (1.4%) suffered from a fungal infection in the mastoid cavity and the headplate of the prosthesis started to migrate (patient 31) (Table 3). Due to the retrospective design of the study, there was no further information available regarding the current status of the adverse events.
Children (N = 6)
The mean post-operative follow-up time of the 6 children was 549 ± 46 days (range: 478–606 days; median: 555 days). 1 (patient 23) out of 6 children had an AE, which is described above.
Discussion
History of the clip mechanism development
Hüttenbrink et al. reported in 2004, of developing a new design of prothesis, with the company Heinz Kurz GmbH, Dusslingen, Germany; this clip prosthesis consisted of elastically flexible feet, which gripped the stapes head and allowed a stable anchoring on the stapes [3]. In 2009, Hüttenbrink et al. combined the clip and the angular mechanism techniques and developed with the company Heinz Kurz GmbH, Dusslingen, Germany the new titanium angular clip prosthesis [4]. In 2011, Beutner et al. modified a common clip prosthesis type Dresden with a ball joint between the prosthesis plate and shaft [5]. The clip design of the mCLIP Partial Prosthesis is based on that of the titanium angular clip prothesis [4]. Hüttenbrink et al. reported that more contact points between the prosthesis and stapes result in a more beneficial anchoring of the prosthesis. Four (longer) of the seven clip prosthesis legs encompass the stapes head and come together between the crura; two (shorter) of the legs stabilize the prosthesis from the rear and one (shorter) leg from the front [3].
PTA4 ABG
Clinical data of our study show satisfactory audiological parameters after the implantation of the mCLIP Partial Prosthesis with a mean PTA4 ABG of 16.3 ± 10.9 dB (N = 68) and stable BC PTA4 thresholds in 67 of the 68 patients.
During a similar trial, Gostian et al. conducted a retrospective study with 47 patients (47 ears) implanted with the Clip Partial Prosthesis Dresden Type (Heinz Kurz GmbH, Dusslingen, Germany), showing a mean post-operative PTA4 ABG of 20.9 ± 10.4 dB at the early follow-up at 21.1 days (range: 23.1–25.5 days). The clip design allows for stable placement and removal of the partial prosthesis without necrosis or other damage to the stapes head [7]. Our mean PTA4 ABG results (N = 68, 16.3 ± 10.9 dB) with the mCLIP Partial Prosthesis are comparable to the short-term results of Gostian et al. (20.9 ± 10.4 dB). Zaoui et al. conducted a prospective study with 52 patients implanted with a Dresden type clip partial prosthesis (Kurz, Germany). The patients were followed for 4 weeks. The mean post-operative PTA4 ABG was 22.4 ± 3.1 dB [8]. The mean PTA4 ABG of our (16.3 ± 10.9 dB) study was favourable to the results of Zaoui et al. (22.4 ± 3.1 dB) [8]. Neudert et al. reported of 29 patients implanted with a titanium clip prosthesis. The mean post-operative PTA4 ABG was 18.8 ± 1.6 dB. 66% of the patients had a post-operative PTA4 ABG of ≤ 20 dB [9]. Our mean PTA4 ABG results and the percentage of the mCLIP Partial Prosthesis patients which reached a PTA4 ABG of ≤ 20 dB is in accordance with results of Neudert et al.[9]. Omar et al. conducted a systematic review with a meta-analysis of 11 papers, which included 202 children, aged ≤ 18 years, implanted with a partial ossicular replacement prosthesis. 62.5% of the children had a post-operative ABG of ≤ 20 dB. The mean post-operative ABG ranged from 13.0 ± 6.1 to 23.8 ± 12.9 dB [10]. In our study 5 out of 6 children reached a post-operative ABG of ≤ 20 dB, with a mean range from 6.3–25.0 dB. Only 1 child had a PTA4 ABG of > 20 dB (patient 23, 25.0 dB). Our results are in accordance with the results of Omar et al. [10]. In sum, our audiological results are in accordance with [7,8,9,10,11].
BC PTA4
Birk et al. evaluated the CLIP Partial FlexiBAL prosthesis (Heinz Kurz GmbH, Dusslingen, Germany) in 60 patients (62 ears). The first follow-up was in mean 19 days after the surgery. The mean BC PTA4 threshold was 20.2 dB HL pre-operatively and 18.1 dB HL post-operatively. The post-operative BC was stable in all 62 ears [12]. In our study the mean BC PTA4 threshold was for all patients (N = 68) 21.4 ± 13.8 dB HL pre-operatively and 18.9 ± 13.9 dB HL post-operatively, which is in accordance with the results of Birk et al. [12].
Gostian et al. reported for the early- and late follow-up that BC thresholds had no significant differences and that the mean changes in BC PTA4 thresholds were < 10 dB HL at all frequencies [7]. Kahue et al. reported that no patient experienced a BC PTA4 shift of > 15 dB HL for the short- and long-term follow-up [11]. Birk et al. [12], Gostian et al. [7], and Kahue et al. [11] included children, but they did not report separately for children. There is no consensus on comparison of post-operative sensorineural hearing loss (SNHL) [7, 11, 12]. However, when comparing the results of our study to Gostian et al. (mean changes in BC PTA4 thresholds were < 10 dB HL at all frequencies), and Kahue et al. (no patient experienced a BC PTA4 shift of > 15 dB HL), there is only one (1.5%) patient (patient 11, adult) with a BC PTA4 deterioration of ≥ 10 dB HL (16.3 dB HL).
Adverse events
Three of the 72 patients (27 AEs + 2 Follow-Ups) showed 3 adverse events, which should be discussed. One patient (1.4%) showed a recurrent cholesteatoma, which resulted in the replacement of the mCLIP Partial Prosthesis with a total ossicular replacement prosthesis; this revision surgery was not device related (patient 23). One (1.4%) patient had an extrusion in combination with a hearing reduction. A hearing device was recommended or was already used after the recommendation (patient 24). One patient (1.4%) suffered from an infection, and the prosthesis started to migrate (patient 31).
Yu et al. evaluated the effectiveness and the stability of the partial ossicular replacement prosthesis using a meta-analysis. The post-operative follow-up time was < 3 years for short-term and ≥ 3 years for long-term. 3.3% of the patients had an extrusion at the short-term follow-up. 6.7% of the patients had an extrusion at the long-term follow-up. No information on the revision surgeries was given [13].
Omar et al. reported that 3% of the children had an extrusion of the prosthesis. The mean post-operative follow-up time ranged from 12–72 months [10].
In our mean follow-up period of 368 ± 177 days, it is not significant to draw a valid conclusion about the rates of revision surgeries, extrusions, and migrations. However, if our revision rate (1.4%) and our extrusion rate (1.4%) is compared to the rates of Yue et al. [13] and Omar et al. [10], they are in accordance. The rates of revision surgeries, extrusions, and migrations increase with the length of the post-operative follow-up time, which was demonstrated by the long-term safety of Yu et al. [13].
The type of partial ossicular replacement prosthesis determines the stability of the connection between the tympanic membrane and the stapes. The availability of the malleus handle, the mucosal status of the middle ear and the status of the stapes footplate, all have an important impact on the post-operative hearing results [14].
Further detrimental influences on post-operative hearing include mucosal fibrosis, drainage, revision ear surgeries and the type of surgical technique used [15]. An intra-operative and post-operative assessment of the quality of the tympanoplasty surgical technique is limited [16], and surgical interventions cannot solve every problem in the middle ear. In most cases, the mucosal function of the middle ear and the eustachian tube cannot be reconstructed completely, which results in insufficient ventilation and thus insufficient vibration of the restored middle ear [17]. In general, ossicular reconstruction depends on several anatomical factors such as aeration of the middle ear, inflammatory status of the middle ear, remnants of the ossicles, condition of the tympanic membrane (e.g., size, defect, thickness of the tympanic membrane graft), status of mucosa, experience of the surgeon and follow-up period [18], that’s why surgery results are often difficult to compare.
Conclusion
In this short-term study, 72.1% of patients achieved a post-operative PTA4 ABG of ≤ 20 dB. Only one patient had a BC PTA4 decrease of > 10 dB HL (16.3 dB HL). The rates of performed and suggested revision surgeries, the rates of extrusions and migrations was in each case one (1.4%) patient. The follow-up time is too short to draw a final conclusion about these rates. A long-term follow-up study should be performed regarding adverse events. In summary, the mCLIP Partial Prosthesis is safe and effective for all patients (adults and children).
References
Babighian G, Albu S (2011) Stabilising total ossicular replacement prosthesis for ossiculoplasty with an absent malleus in canal wall down tympanomastoidectomy - a randomised controlled study. Clin Otolaryngol 36:543–549. https://doi.org/10.1111/j.1749-4486.2011.02406.x
Quesnel S, Teissier N, Viala P et al (2010) Long term results of ossiculoplasties with partial and total titanium Vario Kurz prostheses in children. Int J Pediatr Otorhinolaryngol 74:1226–1229. https://doi.org/10.1016/j.ijporl.2010.07.015
Hüttenbrink KB, Zahnert T, Wüstenberg EG et al (2004) Titanium clip prosthesis Otol Neurotol 25:436–442. https://doi.org/10.1097/00129492-200407000-00006
Huttenbrink KB, Luers JC, Beutner D (2009) Titanium angular clip: a new prosthesis for reconstruction of the long process of the incus. Otol Neurotol 30:1186–1190. https://doi.org/10.1097/MAO.0b013e3181b287f2
Beutner D, Luers JC, Bornitz M et al (2011) Titanium clip ball joint: a partial ossicular reconstruction prosthesis. Otol Neurotol 32:646–649. https://doi.org/10.1097/MAO.0b013e318213867a
Beleites T, Neudert M, Beutner D et al (2011) Experience with vibroplasty couplers at the stapes head and footplate. Otol Neurotol 32:1468–1472. https://doi.org/10.1097/MAO.0b013e3182380621
Gostian AO, Kouame JM, Bremke M et al (2016) Long term results of the titanium clip prosthesis. Eur Arch Otorhinolaryngol 273:4257–4266. https://doi.org/10.1007/s00405-016-4174-3
Zaoui K, Kromeier J, Neudert Met al. (2014) Clinical investigation of flat panel CT following middle ear reconstruction: a study of 107 patients Eur Radiol 24:587–94. https://doi.org/10.1007/s00330-013-3068-7
Neudert M, Zahnert T, Lasurashvili N et al (2009) Partial ossicular reconstruction: comparison of three different prostheses in clinical and experimental studies. Otol Neurotol 30:332–338. https://doi.org/10.1097/MAO.0b013e31819679dd
Omar M, McCoy JL, Kitsko DJ et al (2023) PORP vs. TORP in children: A systematic review and meta-analysis Am J Otolaryngol 44:103658. https://doi.org/10.1016/j.amjoto.2022.103658
Kahue CN, O’Connnell BP, Dedmon MM et al (2018) Short and Long-Term Outcomes of Titanium Clip Ossiculoplasty. Otol Neurotol 39:e453–e460. https://doi.org/10.1097/mao.0000000000001795
Birk S, Brase C, Hornung J (2014) Experience with the use of a partial ossicular replacement prosthesis with a ball-and-socket joint between the plate and the shaft. Otol Neurotol 35:1248–1250. https://doi.org/10.1097/mao.0000000000000383
Yu H, He Y, Ni Yet al. (2013) PORP vs. TORP: a meta-analysis Eur Arch Otorhinolaryngol 270:3005–17. https://doi.org/10.1007/s00405-013-2388-1
De Vos C, Gersdorff M, Gérard JM (2007) Prognostic factors in ossiculoplasty Otol Neurotol 28:61–67. https://doi.org/10.1097/01.mao.0000231598.33585.8f
Dornhoffer JL, Gardner E (2001) Prognostic factors in ossiculoplasty: a statistical staging system. Otol Neurotol 22:299–304. https://doi.org/10.1097/00129492-200105000-00005
Neudert M, Zahnert T (2017) Tympanoplasty - news and new perspectives GMS Curr Top Otorhinolaryngol Head Neck Surg 16:Doc07. https://doi.org/10.3205/cto000146
Zahnert T (2005) Reconstructive methods in hearing disorders - surgical methods GMS Curr Top Otorhinolaryngol Head Neck Surg 4:Doc02.
Lüers JC, Beutner D, Hüttenbrink KB (2010) [Reconstruction of the ossicular chain--current strategies] Laryngorhinootologie 89:172–81; quiz 82–3. https://doi.org/10.1055/s-0030-1248308
Funding
Open access funding provided by Johannes Kepler University Linz. This study was funded by MED-EL Medical Electronics, Innsbruck, Austria. Aylin Zengin and Noelani Peet (both MED-EL) edited a version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rasse, T., Niederwanger, L., Hornung, J. et al. Short-term safety and effectiveness of the mCLIP partial prosthesis. Eur Arch Otorhinolaryngol 281, 2353–2363 (2024). https://doi.org/10.1007/s00405-023-08359-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08359-1