Abstract
Background and aim
Minimally invasive endoscopic techniques are the treatment of choice for Zenker’s diverticulum (ZD). Our objective was to evaluate the results and efficacy of endoscopic and open approaches, to determine whether postoperative C-reactive protein (CRP) serum levels can be used as a marker to exclude the presence of esophageal leakage, and to identify risk factors for development of postoperative leakage and complications.
Materials and methods
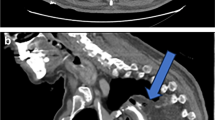
Patients who underwent transcervical myotomy and diverticulotomy (TMD) or endoscopic cricopharyngeal myotomy (ECM) with CO2 laser for ZD in years 2008–2021 at our department were included in this retrospective study.
Results
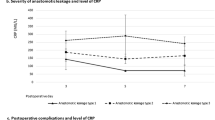
Of the 101 patients enrolled, 83 patients underwent ECM and 18 TMD. The procedure time of the endoscopic technique was significantly shorter compared to that of transcervical method (p < 0.001). The median time to oral intake was 6 days for ECM and 10.5 days in the TMD group (p < 0.001). There was a 13% (n = 11) and 16.7% (n = 3) symptomatic recurrence rate and 3.6% (n = 3) and 16.7% (n = 3) major complications rate for ECM and TMD groups, respectively. The incidence of contrast leak (CL) evaluated by postoperative swallow study was 8.9% (9 from 83 patients in the ECM group only). In patients with CL, a significant increase in CRP levels on postoperative day (POD) 2 and 3 was detected when compared to patients without CL.
Conclusions
Endoscopic diverticulotomy with CO2 laser represents a safe and efficient treatment of ZD. Elevation of postoperative CRP serum levels over 123.8 mg/L on POD2 and 98.8 mg/L on POD3 may indicate presence of an esophageal leakage.


Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are not openly available due to reasons of sensitivity personal data and are available in electronic version (Excel document) from the corresponding author upon reasonable request.
References
Bizzotto A, Iacopini F, Landi R, Costamagna G (2013) Zenker’s diverticulum: exploring treatment options. Acta Otorhinolaryngol Ital 33(4):219–229
Ferreira LE, Simmons DT, Baron TH (2008) Zenker’s diverticula: pathophysiology, clinical presentation, and flexible endoscopic management. Dis Esophagus 21(1):1–8. https://doi.org/10.1111/j.1442-2050.2007.00795.x
Koch M, Mantsopoulos K, Velegrakis S, Iro H, Zenk J (2011) Endoscopic laser-assisted diverticulotomy versus open surgical approach in the treatment of Zenker’s diverticulum. Laryngoscope 121(10):2090–2094. https://doi.org/10.1002/lary.22152
Albers DV, Kondo A, Bernardo WM, Sakai P, Moura RN, Silva GL, Ide E, Tomishige T, de Moura EG (2016) Endoscopic versus surgical approach in the treatment of Zenker’s diverticulum: systematic review and meta-analysis. Endosc Int Open 4(6):E678-686. https://doi.org/10.1055/s-0042-106203
Greene CL, McFadden PM, Oh DS, Chang EJ, Hagen JA (2015) Long-term outcome of the treatment of Zenker’s diverticulum. Ann Thorac Surg 100(3):975–978. https://doi.org/10.1016/j.athoracsur.2015.04.029
Chang CW, Burkey BB, Netterville JL, Courey MS, Garrett CG, Bayles SW (2004) Carbon dioxide laser endoscopic diverticulotomy versus open diverticulectomy for Zenker’s diverticulum. Laryngoscope 114(3):519–527. https://doi.org/10.1097/00005537-200403000-00025
Yuan Y, Zhao YF, Hu Y, Chen LQ (2013) Surgical treatment of Zenker’s diverticulum. Dig Surg 30(3):207–218. https://doi.org/10.1159/000351433
Visser LJ, Hardillo JA, Monserez DA, Wieringa MH, Baatenburg de Jong RJ (2016) Zenker’s diverticulum: Rotterdam experience. Eur Arch Otorhinolaryngol 273(9):2755–2763. https://doi.org/10.1007/s00405-015-3825-0
Akashi M, Furudoi S, Hashikawa K, Sakakibara A, Hasegawa T, Shigeta T, Minamikawa T, Komori T (2015) Postoperative abnormal response of C-reactive protein as an indicator for infectious complications after oral oncologic surgery with primary reconstruction. J Otolaryngol Head Neck Surg 44:13. https://doi.org/10.1186/s40463-015-0066-6
Santonocito C, De Loecker I, Donadello K, Moussa MD, Markowicz S, Gullo A, Vincent JL (2014) C-reactive protein kinetics after major surgery. Anesth Analg 119(3):624–629. https://doi.org/10.1213/ANE.0000000000000263
van Winsen M, McSorley ST, McLeod R, MacDonald A, Forshaw MJ, Shaw M, Puxty K (2021) Postoperative C-reactive protein concentrations to predict infective complications following gastrectomy for cancer. J Surg Oncol 124(7):1060–1069. https://doi.org/10.1002/jso.26613
Dutta S, Fullarton GM, Forshaw MJ, Horgan PG, McMillan DC (2011) Persistent elevation of C-reactive protein following esophagogastric cancer resection as a predictor of postoperative surgical site infectious complications. World J Surg 35(5):1017–1025. https://doi.org/10.1007/s00268-011-1002-1
Messias BA, Botelho RV, Saad SS, Mocchetti ER, Turke KC, Waisberg J (2020) Serum C-reactive protein is a useful marker to exclude anastomotic leakage after colorectal surgery. Sci Rep 10(1):1687. https://doi.org/10.1038/s41598-020-58780-3
Hering S, Wiegand S (2019) Systemic inflammatory response after endoscopic surgery of Zenker’s diverticulum. Acta Otorhinolaryngol Ital 39(4):230–234. https://doi.org/10.14639/0392-100X-1576
Plzak J, Zabrodsky M, Lukes P (2014) Zenker’s diverticulum: carbon dioxide laser endoscopic surgery. Biomed Res Int 2014:516231. https://doi.org/10.1155/2014/516231
Jammer I, Wickboldt N, Sander M, Smith A, Schultz MJ, Pelosi P, Leva B, Rhodes A, Hoeft A, Walder B, Chew MS, Pearse RM, European Society of A, the European Society of Intensive Care M, European Society of A, European Society of Intensive Care M (2015) Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol 32(2):88–105. https://doi.org/10.1097/EJA.0000000000000118
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240(2):205–213. https://doi.org/10.1097/01.sla.0000133083.54934.ae
Wheeler WI (1886) Pharyngocele and dilatation of pharynx, with existing diverticulum at lower portion of pharynx lying posterior to the Œsophagus, cured by pharyngotomy, being the first case of the kind recorded. Dublin J Med Sci 82(5):349–356. https://doi.org/10.1007/BF02970535
Mosher HP (1917) Webs and pouches of the esophagus: their diagnosis and treatment. Surg Gynecol Obstet 25:175–187
Johnson CM, Postma GN (2016) Zenker diverticulum-which surgical approach is superior? JAMA Otolaryngol Head Neck Surg 142(4):401–403. https://doi.org/10.1001/jamaoto.2015.3892
Keck T, Rozsasi A, Grun PM (2010) Surgical treatment of hypopharyngeal diverticulum (Zenker’s diverticulum). Eur Arch Otorhinolaryngol 267(4):587–592. https://doi.org/10.1007/s00405-009-1079-4
Saetti R, Silvestrini M, Peracchia A, Narne S (2006) Endoscopic stapler-assisted Zenker’s diverticulotomy: which is the best operative facility? Head Neck 28(12):1084–1089. https://doi.org/10.1002/hed.20431
Murer K, Soyka MB, Broglie MA, Huber GF, Stoeckli SJ (2015) Zenker’s diverticulum: outcome of endoscopic surgery is dependent on the intraoperative exposure. Eur Arch Otorhinolaryngol 272(1):167–173. https://doi.org/10.1007/s00405-014-2959-9
Courson AM, Landry AM, Lott DG, Hinni ML (2013) Open staple diverticulectomy for a large recurrent Zenker’s diverticulum: still a valid procedure. Ann Otol Rhinol Laryngol 122(12):729–733. https://doi.org/10.1177/000348941312201201
Feeley MA, Righi PD, Weisberger EC, Hamaker RC, Spahn TJ, Radpour S, Wynne MK (1999) Zenker’s diverticulum: analysis of surgical complications from diverticulectomy and cricopharyngeal myotomy. Laryngoscope 109(6):858–861. https://doi.org/10.1097/00005537-199906000-00003
Shah RN, Slaughter KA, Fedore LW, Huang BY, Deal AM, Buckmire RA (2016) Does residual wall size or technique matter in the treatment of Zenker’s diverticulum? Laryngoscope 126(11):2475–2479. https://doi.org/10.1002/lary.25975
Barton MD, Detwiller KY, Palmer AD, Schindler JS (2016) The safety and efficacy of endoscopic Zenker’s diverticulotomy: a cohort study. Laryngoscope 126(12):2705–2710. https://doi.org/10.1002/lary.26046
Berger MH, Weiland D, Tierney WS, Bryson PC, Weissbrod PA, Shah PV, Shah RN, Buckmire RA, Verma SP (2021) Surgical management of recurrent Zenker’s diverticulum: a multi-institutional cohort study. Am J Otolaryngol 42(1):102755. https://doi.org/10.1016/j.amjoto.2020.102755
Adam SI, Paskhover B, Sasaki CT (2012) Laser versus stapler: outcomes in endoscopic repair of Zenker diverticulum. Laryngoscope 122(9):1961–1966. https://doi.org/10.1002/lary.23398
Witterick IJ, Gullane PJ, Yeung E (1995) Outcome analysis of Zenker’s diverticulectomy and cricopharyngeal myotomy. Head Neck 17(5):382–388. https://doi.org/10.1002/hed.2880170504
Ong CC, Elton PG, Mitchell D (1999) Pharyngeal pouch endoscopic stapling–are post-operative barium swallow radiographs of any value? J Laryngol Otol 113(3):233–236. https://doi.org/10.1017/s0022215100143646
Berzofsky CE, Holiday RA, Pitman MJ (2012) Variability of postoperative esophagrams after endoscopic cricopharyngeal myotomy: technique dependence. Ann Otol Rhinol Laryngol 121(3):145–150. https://doi.org/10.1177/000348941212100301
Rizzetto C, Zaninotto G, Costantini M, Bottin R, Finotti E, Zanatta L, Guirroli E, Ceolin M, Nicoletti L, Ruol A, Ancona E (2008) Zenker’s diverticula: feasibility of a tailored approach based on diverticulum size. J Gastrointest Surg 12(12):2057–2064. https://doi.org/10.1007/s11605-008-0684-7 (discussion 2064–2055)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This article does not contain any animal studies conducted by the authors. The study was conducted in accordance with the guidelines of the Helsinki Declaration and its subsequent amendments. Retrospective study does not require approval by an ethical committee in our country.
Informed consent
Informed consent was not needed; it is a retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kana, M., Kalfert, D., Lukes, P. et al. C-reactive protein as an early marker of postoperative leakage in patients after endoscopic laser assisted Zenker’s diverticulotomy. Eur Arch Otorhinolaryngol 280, 2007–2016 (2023). https://doi.org/10.1007/s00405-022-07764-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07764-2