Abstract
Purpose
The aim of this study was to identify the frequency of swallowing disorders and the associated factors in older adults living in nursing homes.
Methods
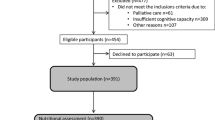
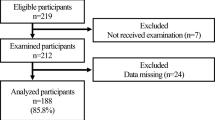
This is a cross-sectional study with a sample of 73 older adults (≥ 60 years; mean age = 80 ± 7.49 years; female = 82.2%) living in five non-profit Brazilian nursing homes. Demographic and clinical data were collected. The frequency of swallowing disorders was determined by the Volume-Viscosity Swallow Test (VVS-T). Covariables with a p-value less than 0.20 according to Pearson's chi-square test or Fisher's exact test were included in the multiple logistic regression analysis model. The level of significance was 5%.
Results
The frequency of swallowing disorders was 63%. The multiple logistic regression model revealed that the chance of an older adult living in a nursing home presenting with swallowing disorders increased by 8% with each 1-year increase in age. Decreases in oral intake level improved the chance of a negative result in the VVS-T by approximately four times, and an individual with a FOIS level below seven was almost 11 times more likely to have a swallowing disorder.
Conclusion
The frequency of swallowing disorders in older adults living in nursing homes is high and is associated with age and oral intake. The management care team should be aware of the early detection of these conditions to prevent complications of oropharyngeal dysphagia.


Similar content being viewed by others
Data availability
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
References
Wakabayashi H, Sashika H, Matsushima M (2015) Head lifting strength is associated with dysphagia and malnutrition in frail older adults. Geriatr Gerontol Int 15(4):410–416. https://doi.org/10.1111/ggi.12283
Groher ME (1997) Dysphagia: diagnosis and management, 3rd edn. Butterworth-Heinemann, Boston
Furkim AM, Duarte ST, Hildebrandt PT, Rodrigues KA. A instituição asilar como fator potencializador da disfagia. Rev. CEFAC. 2010; 12(6): 954–63. Portuguese.
Kua CH, Mak VSL, Huey Lee SW (2019) Health outcomes of deprescribing interventions among older residents in nursing homes: a systematic review and meta-analysis. J Am Med Dir Assoc 20(3):362-372.e11. https://doi.org/10.1016/j.jamda.2018.10.026
Santos BP, Andrade MJC, Silva RO, Menezes EC (2018) Dysphagia in the elderly in long-term care facilities. Rev CEFAC 20(1):123–130. https://doi.org/10.1590/1982-021620182013817
Xavier JS, Gois ACB, Travassos LCP, Pernambuco L (2021) Oropharyngeal dysphagia frequency in older adults living in nursing homes: an integrative review. CoDAS 33(3):e20200153. https://doi.org/10.1590/2317-1782/20202020153
Pernambuco L, Espelt A, Góis ACB, de Lima KC (2017) Voice disorders in older adults living in nursing homes: prevalence and associated factors. J Voice 31(4):510.e15-510.e21. https://doi.org/10.1016/j.jvoice.2016.11.015
Ferrero López MI, García Gollarte JF, Botella Trelis JJ, Juan Vidal O. Detección de disfagia en mayores institucionalizados [Detection of dysphagia in the institutionalised elderly]. Rev Esp Geriatr Gerontol. 2012 Jul-Aug;47(4):143-7. Spanish. DOI: https://doi.org/10.1016/j.regg.2011.09.004
Pfeiffer E (1975) A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 23(70):433–441. https://doi.org/10.1111/j.1532-5415.1975.tb00927.x
Rodrigues RMC (2008) Validation of the European Portuguese version of a multidimensional functional assessment questionnaire for the elderly. Rev Panam Salud Publica 23(2):109–115. https://doi.org/10.1590/S1020-49892008000200006
Magalhães Junior HV, Pernambuco LA, Cavalcanti RVA, Lima KC, Ferreira MAF (2020) Validity evidence of an epidemiological oropharyngeal dysphagia screening questionnaire for older adults. Clinics (Sao Paulo) 75:e1425. https://doi.org/10.6061/clinics/2020/e1425
Magalhães Junior HV, Pernambuco LA, Cavalcanti RVA, Silva RGD, Lima KC, Ferreira MAF. Accuracy of an epidemiological oropharyngeal dysphagia screening for older adults. Gerodontology. 2021. Epub ahead of print. DOI: https://doi.org/10.1111/ger.12613.
Rofes L, Arreola V, Mukherjee R, Clavé P (2014) Sensitivity and specificity of the eating assessment tool and the volume-viscosity swallow test for clinical evaluation of oropharyngeal dysphagia. Neurogastroenterol Motil 26(9):1256–1265. https://doi.org/10.1111/nmo.12382
Rofes L, Arreola V, Clavé P (2012) The volume-viscosity swallow test for clinical screening of dysphagia and aspiration. Nestle Nutr Inst Workshop Ser 72:33–42. https://doi.org/10.1159/000339979
Furkim AM, Sacco ABF (2008) Eficácia da fonoterapia em disfagia neurogênica usando a escala funcional de ingestão por via oral (FOIS) como marcador. Rev CEFAC 10(4):503–512. https://doi.org/10.1590/S1516-18462008000400010
Crary MA, Mann GD, Groher ME (2005) Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 86(8):1516–1520. https://doi.org/10.1016/j.apmr.2004.11.049
Rosa VPPR, Cappellari FCBD, Urbanetto JS (2019) Analysis of risk factors for falls in institutionalized elderly. Rev bras geriatr gerontol 22(1):e180138. https://doi.org/10.1590/1981-22562019022.180138
Scherrer Jr G, Okuno MFP, Oliveira LM, Barbosa DA, Alonso AC, Fram DS et al. Quality of life of institutionalized elderly with and without signs of depression. Rev Bras Enferm. 2019; 72 (Suppl 2): 127–33. https://doi.org/10.1590/0034-7167-2018-0316
Damo CC, Doring M, Alves ALS, Portella MR (2018) Malnutrition risk and associated factors in institutionalized elderly. Rev Bras Geriatr Gerontol 21(6):735–742. https://doi.org/10.1590/1981-22562018021.180152
Silva E, Farias IP, Montenegro LA, de Araújo EG, Raymundo ML, Brito AC, de Lucena EH et al (2021) Impact of oral health on nutritional status, self-perception of oral health and quality of life of institutionalized elderly. J Clin Exp Dent 13(2):e172–e178. https://doi.org/10.4317/jced.57340
Inouye K, Pedrazzani ES. Educational status, social economic status and evaluation of some dimensions of octogenarians' quality of life. Rev Lat Am Enfermagem. 2007;15 Spec No:742–7. https://doi.org/10.1590/s0104-11692007000700005.
Clarke P, Colantonio A. Wheelchair use among community-dwelling older adults: Prevalence and risk factors in a national sample. Can J Aging. 2005 Summer;24(2):191–8. https://doi.org/10.1353/cja.2005.0059.
Oliveira BS, Delgado SE, Brescovici SM (2014) Changes in chewing and swallowing functions in the feeding process of institutionalized elderly. Rev Bras Geriatr Gerontol 17(3):575–587. https://doi.org/10.1590/1809-9823.2014.13065
Santelle O, Lefrève AMC, Cervato AM. Institutionalized food and its social representations among residents of long-term care facilities for the elderly in São Paulo. Cad. Public Health, Rio de Janeiro. 2007; 23(12):3061–65. Portuguese. https://doi.org/10.1590/S0102-311X2007001200029
Presse N, Ferland G (2010) Risk factors contributing to insufficient water intake in elderly living in nursing homes and long-term care units: a review of the literature. Can J Dietetic Practice Res 71(4):94–99. https://doi.org/10.3148/71.4.2010.206
Santoro PP, Furia CL, Forte AP, Lemos EM, Garcia RI, Tavares RA et al (2011) Otolaryngology and speech therapy evaluation in the assessment of oropharyngeal dysphagia: a combined protocol proposal. Braz J Otorhinolaryngol 77(2):201–213. https://doi.org/10.1590/s1808-86942011000200010
Kendall K (2007) Presbyphonia: a review. Curr Opin Otolaryngol Head Neck Surg 15(3):137–140. https://doi.org/10.1097/MOO.0b013e328166794f
Suominen M, Muurinen S, Routasalo P, Soini H, Suur-Uski I, Peiponen A, Finne-Soveri H, Pitkala KH (2005) Malnutrition and associated factors among aged residents in all nursing homes in Helsinki. Eur J Clin Nutr 59(4):578–583. https://doi.org/10.1038/sj.ejcn.1602111
Fernández-Getino Sallés C. Prevalencia de disfagia orofaríngea en ancianos institucionalizados y su relación con síndromes geriátricos. Rev Logop Fon Audiol. 2018;38(2):69–76. https://doi.org/10.1016/j.rlfa.2017.09.001.
Logemann JA, Curro FA, Pauloski B, Gensler G (2013) Aging effects on oropharyngeal swallow and the role of dental care in oropharyngeal dysphagia. Oral Dis 19(8):733–737. https://doi.org/10.1111/odi.12104
Matsuo K, Palmer JB (2008) Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am 19(4):691–707. https://doi.org/10.1016/j.pmr.2008.06.001
Kertscher B, Speyer R, Fong E, Georgiou AM, Smith M (2015) Prevalence of oropharyngeal dysphagia in the Netherlands: a telephone survey. Dysphagia 30(2):114–120. https://doi.org/10.1007/s00455-014-9584-z
Wakabayashi H, Matsushima M (2016) Dysphagia assessed by the 10-item eating assessment tool is associated with nutritional status and activities of daily living in elderly individuals requiring long-term care. J Nutr Health Aging 20(1):22–27. https://doi.org/10.1007/s12603-016-0671-8
Izaola O, Gómez Hoyos E, López JJ, Ortola A, Torres B, Primo D, Castro Á, De Luis Román DA (2018) The 10-item eating assessment tool is associated with nutritional status, mortality and hospital stay in elderly individuals requiring hospitalization with acute diseases. Nutr Hosp 35(4):827–832. https://doi.org/10.20960/nh.1698
Acknowledgements
The authors acknowledge the support given by the board of directors and workers of the five non-profit nursing homes included in this study. We also thank the support of all the undergraduate students who contributed to the acquisition of data.
Funding
This study was supported in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brazil (CAPES) [Funding Agency] under Grant Finance Code 001.
Author information
Authors and Affiliations
Contributions
JSX, ACBG and LP contributed to the study conception and design. Acquisition of data, and the first draft of the manuscript were performed by JSX and ACBG. LMALF performed the statistical analysis. All authors contributed to the interpretation of data, critical revision, and the final draft of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Disclosure
No ethical approval was necessary.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Xavier, J.S., Gois, A.C.B., Costa Lima, K. et al. Swallowing disorders and associated factors in older adults living in nursing homes. Eur Arch Otorhinolaryngol 279, 3733–3740 (2022). https://doi.org/10.1007/s00405-022-07355-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-022-07355-1