Abstract
Purpose
In this experimental study, the effect of dose-dense systemic application of propolis on oral mucosity, histological changes in papilla, and inflammatory and hypoxic markers in rats exposed to radiation was investigated.
Methods
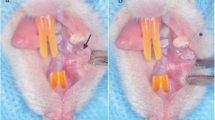
Seven rats were in the control and 30 rats in the experimental group. Three experimental groups were formed. In Group 1 RT (15 Gy) was delivered only to the head and neck region. In Group 2, RT (15 Gy) and systemic administration of 100 mg/kg/ml propolis, in Group 3, RT (15 Gy) and systemic administration of 200 mg/kg/ml propolis were applied. Oral mucositis index (OMI) was scored in control and experimental groups. Proinflammatory markers [interleukin-6 (IL-6), myeloperoxidase (MPO), tumor-necrosis factor-α (TNF-α)] hypoxia markers [glucose transporter-1 (GLUT-1), hypoxia-inducible factor 1α (HIF-1α)] were studied histomorphologically.
Results
The significantly highest OMI score was observed in the G1. OMI score was statistically significantly decreased in experimental groups receiving systemic propolis, especially in G3. Proinflammatory markers increased significantly only in the experimental RT group, G1. Serum levels of MPO and TNF-α significantly decreased in the dose-dense systemic propolis arm. The highest levels of hypoxia markers (HIF-1α and GLUT-1) were detected in the RT group, then in G2, G3, and control groups in order of decreasing frequency. However, the difference between the groups did not reach the level of statistical significance.
Conclusion
Systemic propolis can be reduced acute mucositis with its anti-inflammatory effect without developing resistance to RT (tumor protection). However, greater number of clinical studies should be designed to arrive at definitive conclusions.





Similar content being viewed by others
References
Vissink A, Jansma J, Spijkervet FK, Burlage FR, Coppes RP (2003) Oral sequelae of head and neck radiotherapy. Crit Rev Oral Biol Med 14:199–212
Trotti A, Bellm LA, Epstein JB, Frame D, Fuchs HJ, Gwede CK et al (2003) Mucositis incidence, severity and associated outcomes in patients with head and neck cancer receiving radiotherapy with or without chemotherapy: a systemic literature review. Radiother Oncol 66:253–262
Sonis ST (2010) New thoughts on the initiation of mucositis. Oral Dis 16:597–600
Nagler RM (2002) The enigmatic mechanism of irradiation-induced damage to the major salivary glands. Oral Dis 8:141–146
Sonis ST (2007) Pathobiology of oral mucositis: novel insights and opportunities. J Support Oncol 5:3–11
Sonti G, Ilyin SE, Plata-Salamán CR (1996) Anorexia induced by cytokine interactions at pathophysiological concentrations. Am J Physiol 270:1394–1402
Opara EI, Laviano A, Meguid MM (1995) Correlation between food intake and cerebrospinal fluid interleukin 1α in anorectic tumor-bearing rats. Nutrition 11:678–679
Laviano A, Gleason JR, Meguid MM, Yang ZJ, Cangiano C, Rossi Fanelli F (2000) Effects of intra-VMN mianserin and IL-1ra on meal number in anorectic tumor-bearing rats. J Investig Med 48:40–48
Dörr W, Kummermehr J (1990) Accelerated repopulation of mouse tongue epithelium during fractionated irradiations or following single doses. Radiother Oncol 17:249–259
Rezvani M, Ross GA (2004) Modification of radiation-induced acute oral mucositis in the rat. Int J Radiat Biol 80:177–182
Sciubba JJ, Goldenberg D (2006) Oral complications of radiotherapy. Lancet Oncol 7:175–183
Lee SW, Jung KI, Kim YW, Jung HD, Kim HS, Hong JP (2007) Effect of epidermal growth factor against radiotherapy-induced oral mucositis in rats. Int J Radiat Oncol Biol Phys 67:1172–1178
Bowen JM, Elad S, Hutchins RD, Lalla RV (2013) Methodology for the MASCC/ISOO mucositis clinical practice guidelines update. Support Care Cancer 21:303–308
Wang K, ZhangJ PingS, Ma Q, ChenX XH et al (2014) Anti-inflammatory effects of ethanol extracts of Chinese propolis and buds from poplar (Populus×canadensis). J Ethnopharmacol 155:300–311
Singla S, Kumar NR, Kaur J (2014) In vivo studies on the protective effect of propolis on doxorubicin-induced toxicity in liver of male rats. Toxicol Int 21:191–195
Parkins CS, Fowler JF, Yu S (1983) A murine model of lip epidermal/mucosal reactions to X-irradiation. Radiother Oncol 1:159–165
BenderliCihan Y, Deniz K (2011) Effect of propolis against radiation-induced oral mucositis in rats. J Ear Nose Throat 21:32–41
Ghassemi L, Zabihi E, Mahdavi R, Seyedmajidi M, Akram S, Motallebnejad M (2010) The effect of ethanolic extract of propolis on radiation-induced mucositis in rats. Saudi Med J 31:622–626
Miyamoto H, Kanayama T, Horii K, Kawai T, Tsuchimochi T, Shigetomi T et al (2015) The relationship between the severity of radiation-induced oral mucositis and the myeloperoxidase levels in rats. Oral Surg Oral Med Oral Pathol Oral Radiol 120:329–336
Khayyal MT, Abdel-Naby DH, El-Ghazaly MA (2019) Propolis extract protects against radiation-induced intestinal mucositis through anti-apoptotic mechanisms. Environ Sci Pollut Res Int 26:24672–24682
Alfaro R, Crowder S, Sarma KP, Arthur AE, Pepino MY (2021) Taste and smell function in head and neck cancer survivors. Chem Senses 46:bjab026. https://doi.org/10.1093/chemse/bjab026 (PMID: 34050750)
Ibrahim MAAH, Elwan WM (2019) Effect of irinotecan on the tongue mucosa of juvenile male albino rat at adulthood. Int J Exp Pathol 100:244–252
Thiruthaneeswaran N, Bibby BAS, Yang L, Hoskin PJ, Bristow RG, Choudhury A et al (2021) Lost in application: measuring hypoxia for radiotherapy optimisation. Eur J Cancer 148:260–276
Berra E, Benizri E, Ginouvès A, Volmat V, Roux D, Pouysségur J (2003) HIF prolyl-hydroxylase 2 is the key oxygen sensor setting low steady-state levels of HIF-1α in normoxia. EMBO J 22:4082–4090
Gruber S, Hamedinger D, Bozsaky E, Schmidt M, Wolfram K, Haagen J et al (2015) Local hypoxia in oral mucosa (mouse) during daily fractionated irradiation—effect of pentoxifylline. Radiother Oncol 116:404–408
Funding
Financial support was received within the scope of the scientific research project of Gaziosmanpasa Üniversitesi, scientific research project no 2020-113.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conficts of interest.
Ethical approval
The study was approved by the ethics committee of Tokat Gaziosmanpaşa University Animal Experiments Local Ethics Committee with the decision no 51879863-118 on 9 September 2020.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guler Avci, G., Erdim, I., Ozmen, Z.C. et al. The effect of systemic application of propolis on tongue damage and oral mucositis in rats exposed to radiation. Eur Arch Otorhinolaryngol 279, 1043–1052 (2022). https://doi.org/10.1007/s00405-021-07159-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-021-07159-9