Abstract
Objective
To investigate the prevalence of DD and AI with POP symptoms in females attending a urogynecology clinic, and to identify factors associated with DD and AI in POP symptoms patients.
Methods
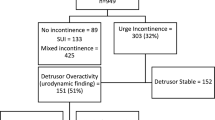
Computer-based medical records of women with POP symptoms attending a urogynecology clinic in a referral tertiary center between January 2016 and December 2020 were reviewed. Demographic data were collected. Selected defecatory dysfunction (DD) and anal incontinence (AI) were recorded. The associations between patient characteristics, site and severity of prolapse, and DD and AI symptoms in POP patients were investigated for identified associated factors.
Results
The mean age of the 754 participants was 65.77 ± 9.44 years. Seven hundred and fifteen (94.83%) were menopause. The prevalence of DD and AI in patients with POP symptoms was 44.03% (332/754) and 42.04% (317/754) according to the PFBQ and medical history records, respectively. Advanced posterior wall prolapse (OR 1.59, 95% CI 1.10–2.30) and wider GH (OR1.23, 95% CI 1.05–1.43) were identified as risk factors for DD by multivariate analysis. Additionally, single-compartment prolapse (OR 0.4, 95% CI 0.21–0.76) and a stronger pelvic floor muscle assessed with brink score (OR 0.94, 95% CI 0.88–0.98) are protective factors for AI.
Conclusion
DD and AI are prevalent among women with POP symptoms who visit a urogynecology clinic. DD should be evaluated in women with POP symptoms especially in women with increased genital hiatus and point Ap beyond the hymen. To prevent AI, women with POP should be encouraged to perform pelvic floor muscle training in order to increase pelvic floor muscle strength.


Similar content being viewed by others

Data availability
The data that support the findings of this study are available from the corresponding authors upon reasonable request.
References
Swift SE (2000) The distribution of pelvic organ support in a population of female subjects seen for routine gynecologic health care. Am J Obstet Gynecol 183(2):277–285. https://doi.org/10.1067/mob.2000.107583
Mattsson NK et al (2020) Pelvic organ prolapse surgery and quality of life-a nationwide cohort study. Am J Obstet Gynecol. https://doi.org/10.1016/j.ajog.2019.11.1285
Haylen BT et al (2009) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. https://doi.org/10.1007/s00192-009-0976-9
Meschia M, Buonaguidi A, Pifarotti P, Somigliana E, Spennacchio M, Amicarelli F (2002) Prevalence of anal incontinence in women with symptoms of urinary incontinence and genital prolapse. Obstet Gynecol 100(4):719–723. https://doi.org/10.1016/s0029-7844(02)02215-9
Raza-Khan F, Cunkelman J, Lowenstein L, Shott S, Kenton K (2010) Prevalence of bowel symptoms in women with pelvic floor disorders. Int Urogynecol J 21(8):933–938. https://doi.org/10.1007/s00192-010-1143-z
Grimes CL, Lukacz ES (2012) Posterior vaginal compartment prolapse and defecatory dysfunction: are they related? Int Urogynecol J 23(5):537–551. https://doi.org/10.1007/s00192-011-1629-3
Andy UU, Harvie HS, Pahwa AP, Markland A, Arya LA (2017) The relationship between fecal incontinence, constipation and defecatory symptoms in women with pelvic floor disorders. Neurourol Urodyn 36(2):495–498. https://doi.org/10.1002/nau.22964
Lacima G, Espuña M, Pera M, Puig-Clota M, Quintó L, García-Valdecasas JC (2002) Clinical, urodynamic, and manometric findings in women with combined fecal and urinary incontinence. Neurourol Urodyn 21(5):464–469. https://doi.org/10.1002/nau.10025
Saks EK, Harvie HS, Asfaw TS, Arya LA (2010) Clinical significance of obstructive defecatory symptoms in women with pelvic organ prolapse. Int J Gynaecol Obstet 111(3):237–240. https://doi.org/10.1016/j.ijgo.2010.06.025
Morgan DM, DeLancey JOL, Guire KE, Fenner DE (2007) Symptoms of anal incontinence and difficult defecation among women with prolapse and a matched control cohort. Am J Obstet Gynecol 197(5):509.e1-509.e5096. https://doi.org/10.1016/j.ajog.2007.03.074
Tan C, Geng J, Tang J, Yang X (2020) The relationship between obstructed defecation and true rectocele in patients with pelvic organ prolapse. Sci Rep. https://doi.org/10.1038/s41598-020-62376-2
Manonai J, Wattanayingcharoenchai R, Sarit-Apirak S, Vannatim N, Chittacharoen A (2010) Prevalence and risk factors of anorectal dysfunction in women with urinary incontinence. Arch Gynecol Obstet 281(6):1003–1007. https://doi.org/10.1007/s00404-009-1223-9
Wattanayingcharoenchai R, Vallibhakara SA, Aimjirakul K (2018) Prevalence and correlates of anal incontinence among urogynecologic patients. J Med Assoc Thai 101(8):1031
Manonai J, Wattanayingcharoenchai R (2016) Relationship between pelvic floor symptoms and POP-Q measurements. Neurourol Urodyn 35(6):724–727. https://doi.org/10.1002/nau.22786
Peterson TV, Karp DR, Aguilar VC, Davila GW (2010) Validation of a global pelvic floor symptom bother questionnaire. Int Urogynecol J 21(9):1129–1135. https://doi.org/10.1007/s00192-010-1148-7
Persu C, Chapple CR, Cauni V, Gutue S, Geavlete P (2011) Pelvic organ prolapse quantification system (POP-Q) a new era in pelvic prolapse staging. J Med Life 75:81
Hundley AF, Wu JM, Visco AG (2005) A comparison of perineometer to brink score for assessment of pelvic floor muscle strength. Am J Obstet Gynecol 192(5):1583–1591. https://doi.org/10.1016/j.ajog.2004.11.015
Bhopal RS (2016) Concepts of epidemiology: integrating the ideas, theories, principles, and methods of epidemiology. Oxf Univ Press. https://doi.org/10.1093/med/9780198739685.001.0001
Bezerra LR et al (2014) Prevalence of unreported bowel symptoms in women with pelvic floor dysfunction and the impact on their quality of life. Int Urogynecol J 25(7):927–933. https://doi.org/10.1007/s00192-013-2317-2
Varma MG, Hart SL, Brown JS, Creasman JM, Van Den Eeden SK, Thom DH (2008) Obstructive defecation in middle-aged women. Dig Dis Sci 53(10):2702–2709. https://doi.org/10.1007/s10620-008-0226-x
Whitcomb E, Lukacz E, Lawrence J, Nager C, Luber K (2009) Prevalence of defecatory dysfunction in women with and without pelvic floor disorders. Female Pelvic Med Reconstruct Surg. https://doi.org/10.1097/SPV.0b013e3181b12e01
Handa VL, Cundiff G, Chang HH, Helzlsouer KJ (2008) Female sexual function and pelvic floor disorders. Obstet Gynecol 111(5):1045–1052. https://doi.org/10.1097/AOG.0b013e31816bbe85
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE (2001) Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. https://doi.org/10.1067/mob.2001.119078
LaCross A, Groff M, Smaldone A (2015) Obstetric anal sphincter injury and anal incontinence following vaginal birth: a systematic review and meta-analysis. J Midwifery Womens Health. https://doi.org/10.1111/jmwh.12283
Shafik A, El-Sibai O (2002) Study of the levator ani muscle in the multipara: role of levator dysfunction in defecation disorders. J Obstetrics and Gynaecol. https://doi.org/10.1080/01443610120113391
Perrin S, Billecocq S (2022) Impact of obstetric lesions of the levator ani on anal continence. Prog Urol 32(17):1519–1530. https://doi.org/10.1016/j.purol.2022.09.017
Wallace SL, Miller LD, Mishra K (2019) Pelvic floor physical therapy in the treatment of pelvic floor dysfunction in women. Curr Opin Obstet Gynecol 31(6):485–493. https://doi.org/10.1097/gco.0000000000000584
Acknowledgements
The authors would like to thank Ms. Sasiporn Sitthisorn for assistance with the statistical analyses. The authors also thank Alison Sherwin, PhD, from Edanz (https://www.edanz.com/ac) for editing a draft of this manuscript. We would like to thank Dr.Kotchakorn Dulyapach for illustrating figure 2.
Funding
None.
Author information
Authors and Affiliations
Contributions
Concept/idea/research design: A. Saraluck, K. Aimjirakul, J.J. Ng, J. Manonai. Data collection: A. Saraluck, P. Mangmeesri. Data analysis: A. Saraluck, O. Chinthakanan, J.J. Ng. Project management: J. Manonai. Manuscript writing: A. Saraluck, J. Manonai. All authors edited and approved the final version to be published.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This study was approved by the Medical and Research Ethics Committee of Ramathibodi Hospital Number MURA2022/750 (Expedited). Since this project was a retrospective chart review in which the data already exist, the informed consent was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saraluck, A., Aimjirakul, K., Jiet, N.J. et al. Defecatory dysfunction and anal incontinence symptoms among women with pelvic organ prolapse: 5-year retrospective study in a tertiary center. Arch Gynecol Obstet 309, 2237–2245 (2024). https://doi.org/10.1007/s00404-024-07426-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-024-07426-0