Abstract
Purpose
To compare the effectiveness of the Cook vaginal cervical ripening balloon (CCRB) with prostaglandin E2 (PGE2) insert for induction of labor in late pregnancy in primipara.
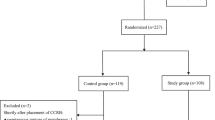
Methods
We evaluated the effectiveness and safety of induction of labor using the improved Bishop score after CCRB or PGE2 administration, total stage of labor, hours until delivery (hours from placement of CCRB or PGE2 insert to parturition and delivery), delivery rate within 24 h, spontaneous delivery rate, successful induction rate, overstimulation syndrome, urgent delivery rate, pain scores, cesarean section rate, and outcomes related to delivery and perinatal morbidity, such as puerperal infection rate, total cost, satisfaction survey, and so on.
Results
The improved Bishop Score and delivery rate within 24 h in the CCRB group were significantly higher than in the PGE2 group. The total stage of labor and hours until delivery in the CCRB group were significantly shorter than that in the PGE2 group. Rate of overstimulation syndrome and pain scores in the CCRB group were significantly lower than in the PGE2 group. Compared with the PGE2 group, the mean duration of hospitalization in the CCRB group was shorter and the total cost was less. No difference in satisfaction between the PGE2 and CCRB groups was observed.
Conclusions
Compared with PGE2, CCRB reduced the total stage of labor, hours until delivery, pain scores, mean length of hospitalization, and total cost. CCRB increased the rate of delivery within 24 h with similar safety and maternal satisfaction compared with PGE2.

Similar content being viewed by others
References
Karahan MA, Incebiyik A, Buyukfirat E, Altay N, Binici O, Besli F (2019) Effect of spinal anesthesia on the QT interval in term and post-term pregnancies scheduled for elective cesarean section: a prospective study. J Matern Fetal Neonatal Med 27:1–5
Ferrazzi E, Brembilla G, Cipriani S, Livio S, Paganelli A, Parazzini F (2019) Maternal age and body mass index at term: risk factors for requiring an induced labour for a late-term pregnancy. Eur J Obstet Gynecol Reprod Biol 233:151–157
Bovbjerg ML, Cheyney M, Brown J, Cox KJ, Leeman L (2017) Perspectives on risk: assessment of risk profiles and outcomes among women planning community birth in the United States. Birth 44:209–221
Wagner MM, Visser J, Verburg H, Hukkelhoven C, Van Lith JMM, Bloemenkamp KWM (2018) Pregnancy before recurrent pregnancy loss more often complicated by post-term birth and perinatal death. Acta Obstet Gynecol Scand 97:82–88
Ferguson KK, Rosario Z, McElrath TF, Velez Vega C, Cordero JF, Alshawabkeh A, Meeker JD (2019) Demographic risk factors for adverse birth outcomes in Puerto Rico in the protect cohort. PLoS ONE 14:e0217770
Hermesch AC, Allshouse AA, Heyborne KD (2016) Body mass index and the spontaneous onset of parturition. Obstet Gynecol 128:1033–1038
Oberg AS, Frisell T, Svensson AC, Iliadou AN (2013) Maternal and fetal genetic contributions to postterm birth: familial clustering in a population-based sample of 475, 429 Swedish births. Am J Epidemiol 177:531–537
Bleicher I, Vitner D, Iofe A, Sagi S, Bader D, Gonen R (2017) When should pregnancies that extended beyond term be induced? J Matern Fetal Neonatal Med 30:219–223
Rydahl E, Eriksen L, Juhl M (2019) Effects of induction of labor prior to post-term in low-risk pregnancies: a systematic review. JBI Database Syst Rev Implement Rep 17:170–208
Maoz O, Wainstock T, Sheiner E, Walfisch A (2019) Immediate perinatal outcomes of post term deliveries. J Matern Fetal Neonatal Med 32:1847–1852
Tsikouras P, Koukouli Z, Manav B, Soilemetzidis M, Liberis A, Csorba R, Trypsianis G, Galazios G (2016) Induction of labor in post-term nulliparous and parous women–potential advantages of misoprostol over dinoprostone. Geburtshilfe Frauenheilkd 76:785–792
Keulen JKJ, Bruinsma A, Kortekaas JC, van Dillen J, van der Post JAM, de Miranda E (2018) Timing induction of labour at 41 or 42 weeks? A closer look at time frames of comparison: a review. Midwifery 66:111–118
Kortekaas JC, Scheuer AC, de Miranda E, van Dijk AE, Keulen JKJ, Bruinsma A, Mol BWJ, Vandenbussche F, van Dillen J (2018) Perinatal death beyond 41 weeks pregnancy: an evaluation of causes and substandard care factors as identified in perinatal audit in the Netherlands. BMC Pregnancy Childbirth 18:380
Kortekaas JC, Kazemier BM, Ravelli AC, de Boer K, van Dillen J, Mol B, de Miranda E (2015) Recurrence rate and outcome of postterm pregnancy, a national cohort study. Eur J Obstet Gynecol Reprod Biol 193:70–74
Deng K, Huang Y, Wang Y, Zhu J, Mu Y, Li X, Xing A, Liu Z, Li M, Wang X, Liang J (2019) Prevalence of postterm births and associated maternal risk factors in China: data from over 6 million births at health facilities between 2012 and 2016. Sci Rep 9:273
Avci S, Simsek M, Soylu H, Ustunel I (2019) Misoprostol-Induced modification of the notch signaling pathway in the human cervix. Reprod Sci 26:909–917
Zhao L, Lin Y, Jiang TT, Wang L, Li M, Wang Y, Sun GQ, Xiao M (2019) Vaginal delivery among women who underwent labor induction with vaginal dinoprostone (PGE2) insert: a retrospective study of 1656 women in China. J Matern Fetal Neonatal Med 32:1721–1727
Lajusticia H, Martinez-Dominguez SJ, Perez-Roncero GR, Chedraui P, Perez-Lopez FR (2018) Single versus double-balloon catheters for the induction of labor of singleton pregnancies: a meta-analysis of randomized and quasi-randomized controlled trials. Arch Gynecol Obstet 297:1089–1100
Bakker R, Pierce S, Myers D (2017) The role of prostaglandins E1 and E2, dinoprostone, and misoprostol in cervical ripening and the induction of labor: a mechanistic approach. Arch Gynecol Obstet 296:167–179
Yayla Abide C, Kurek Eken M, Ozkaya E, Yenidede I, Bostanci Ergen E, Kilicci C, Sanverdi I, Eroglu M (2018) Effect of vaginal washing before intravaginal dinoprostone insertion for labor induction: a randomized clinical trial. J obstet Gynaecol Res 44:2149–2155
Wu X, Wang C, Li Y, Ouyang C, Liao J, Cai W, Zhong Y, Zhang J, Chen H (2018) Cervical dilation balloon combined with intravenous drip of oxytocin for induction of term labor: a multicenter clinical trial. Arch Gynecol Obstet 297:77–83
Olafsdottir AH, Kristofersson DM, Karlsdottir SI (2019) The effects of induced labor at 41 week of pregnancy on mode of delivery and outcome. Laeknabladid 105:115–123
Ciardulli A, D'Antonio F (2019) Fetal brain hemodynamics in pregnancies at term: correlation with gestational age, birthweight and clinical outcome. J Matern Fetal Neonatal Med 9:1–7
Vitner D, Hiersch L, Ashwal E, Shmueli A, Yogev Y, Aviram A (2019) Induction of labor versus expectant management for gestational diabetes mellitus at term. Arch Gynecol Obstet 300:79–86
Leigh S, Granby P, Haycox A, Mundle S, Bracken H, Khedikar V, Mulik J, Faragher B, Easterling T, Turner MA, Alfirevic Z, Winikoff B, Weeks AD (2018) Foley catheter vs. oral misoprostol to induce labour among hypertensive women in India: a cost-consequence analysis alongside a clinical trial. BJOG 125:1734–1742
Church S, Van Meter A, Whitfield R (2009) Dinoprostone compared with misoprostol for cervical ripening for induction of labor at term. J Midwifery Women’s Health 54:405–411
Zhao L, Lin Y, Jiang T, Wang L, Li M, Wang Y, Sun G, Xiao M (2019) Prediction of the induction to delivery time interval in vaginal dinoprostone-induced labor: a retrospective study in a Chinese tertiary maternity hospital. J Int Med Res 47:2647–2654
Chowdhary A, Bagga R (2019) Comparison of intracervical Foley catheter used alone or combined with a single dose of dinoprostone gel for cervical ripening: a randomised study. J Obstet Gynaecol 39:461–467
Kim YM, Park JY, Sung JH, Choi SJ, Oh SY (2017) Predicting factors for success of vaginal delivery in preterm induction with prostaglandin E2. Obstet Gynecol Sci 60:163–169
Vijayasree M (2016) Efficacy of prophylactic b-lynch suture during lower segment caesarean section in high risk patients for atonic postpartum haemorrhage. Kathmandu Univ Med (KUMJ) 14:9–12
Ragusa A, Svelato A (2017) Adjunctive azithromycin prophylaxis for caesarean delivery. N Engl J Med 376:181–182
Mozurkewich EL, Chilimigras JL, Berman DR, Perni UC, Romero VC, King VJ, Keeton KL (2011) Methods of induction of labour: a systematic review. BMC Pregnancy Childbirth 11:84
Diguisto C, Le Gouge A, Giraudeau B, Perrotin F (2017) Mechanical cervical ripening for women with prolongedpregnancies (MAGPOP): protocol for a randomised controlled trial of a silicone double balloon catheter versus the propess system for the slow release of dinoprostone for cervical ripening of prolonged pregnancies. BMJ Open 7:e016069
Ornat L, Alonso-Ventura V, Bueno-Notivol J, Chedraui P (2019) Misoprostol combined with cervical single or double balloon catheters versus misoprostol alone for labor induction of singleton pregnancies: a meta-analysis of randomized trials. J Matern Fetal Neonatal Med 10:1–16
Funding
This study was supported by the grants from Science and Technology Benefit People Special of Qingdao Science and Technology Bureau in China (Grant number: 19-6-1-56-nsh).
Author information
Authors and Affiliations
Contributions
LW designed the protocol and wrote the manuscript. GW, WC, and LG were responsible for statistics of experimental data. YL and HH were charge of chart making. QZ, as the corresponding author, designed the protocol and revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
We have no conflicts of interest to declare.
Ethical approval
This study was approved by the institutional review board of Qingdao Municipal Hospital.
Informed consent
Informed consent was signed by all pregnant women involved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, L., Wang, G., Cao, W. et al. Comparison of the Cook vaginal cervical ripening balloon with prostaglandin E2 insert for induction of labor in late pregnancy. Arch Gynecol Obstet 302, 579–584 (2020). https://doi.org/10.1007/s00404-020-05597-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-020-05597-0