Abstract
Purpose
There is a lack of data regarding maternal morbidity and neonatal hypoxia associated with shoulder dystocia (SD), particularly with respect to whether SD is managed with our without fetal manipulation (FM). Our main objective was to compare severe maternal and neonatal morbidities associated with SD according to FM execution.
Methods
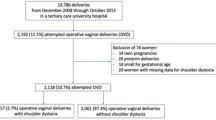
We conducted a retrospective study based on a medical record analysis that included all SD cases from 2007 to 2012. SD was considered when additional maneuvers were required to complete a delivery. Severe maternal morbidity was defined as the occurrence of an obstetric anal sphincter injury. Severe neonatal morbidity was defined as the occurrence of one of these complications: permanent brachial plexus palsy, arterial cord pH < 7.1, Apgar score < 7 at 5 min. We compared severe maternal and neonatal morbidities in the FM and the no-FM group.
Results
We report an SD incidence of 2.4 % (n = 227) with 93.8 % of patients treated without FM. We identified two cases of permanent brachial plexus palsy, fifteen cases of arterial cord pH < 7.1 and six cases with an Apgar score < 7 at 5 min; all of them were from the no-FM group. There were more cases of OASI in the FM group (odd ratio = 9.2 [1.32–50.71]). No statistical differences between these groups were observed with respect to severe neonatal morbidity.
Conclusions
Severe neonatal morbidity does not appear to be associated with FM during SD management, but severe maternal morbidity is associated with FM execution.

Similar content being viewed by others
References
Gherman RB, Chauhan S, Ouzounian JG, Lerner H, Gonik B, Goodwin TM (2006) Shoulder dystocia: the unpreventable obstetric emergency with empiric management guidelines. Am J Obstet Gynecol 195:657–672
Royal College of Obstetricians and Gynaecologists (2012) Green-top guideline No. 42—shoulder dystocia. https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg42/. Last consultation on 10/07/2015
Gurewitsch ED, Donithan M, Stallings SP et al (2004) Episiotomy versus fetal manipulation in managing severe shoulder dystocia: a comparison of outcomes. Am J Obstet Gynecol 191:911–916
Paris AE, Greenberg JA, Ecker JL, McElrath TF (2011) Is an episiotomy necessary with a shoulder dystocia? Am J Obstet Gynecol 205(217):e1–e3
Nygaard IE, Rao SS, Dawson JD (1997) Anal incontinence after anal sphincter disruption: a 30-year retrospective cohort study. Obstet Gynecol 89:896–901
Faltin DL, Otero M, Petignat P et al (2006) Women’s health 18 years after rupture of the anal sphincter during childbirth: I. Fecal incontinence. Am J Obstet Gynecol 194:1255–1259
Dixon G, Badawi N, Kurinczuk JJ et al (2002) Early developmental outcomes after newborn encephalopathy. Pediatrics 109:26–33
Chauhan SP, Blackwell SB, Ananth CV (2014) Neonatal brachial plexus palsy: incidence, prevalence, and temporal trends. Semins Perinatol 38:210–218
Gherman RB, Ouzounian JG, Goodwin TM (1998) Obstetric maneuvers for shoulder dystocia and associated fetal morbidity. Am J Obstet Gynecol 178:1126–1130
Gonik B, Stringer C, Held B (1983) An alternate maneuver for management of shoulder dystocia. Am J Obstet Gynecol 145:882–884
Chauhan SP, Laye MR, Lutgendorf M et al (2014) A multicenter assessment of 1177 cases of shoulder dystocia: lessons learned. Am J Perinatol 31:401–406
Leung TY, Stuart O, Suen SS, Sahota DS, Lau TK, Lao TT (2011) Comparison of perinatal outcomes of shoulder dystocia alleviated by different type and sequence of manoeuvres: a retrospective review. BJOG 118:985–990
MacKenzie IZ, Shah M, Lean K, Dutton S, Newdick H, Tucker DE (2007) Management of shoulder dystocia: trends in incidence and maternal and neonatal morbidity. Obstet Gynecol 110:1059–1068
American College of Obstetricians and Gynecologists (2012) Patient safety checklist No. 6: documenting shoulder dystocia. Obstet Gynecol 120:430–431
Royal College of Obstetricians and Gynaecologists (2015) Green-top guideline No. 29—the management of third- and fourth-degree perineal tears. https://www.rcog.org.uk/globalassets/documents/guidelines/gtg-29.pdf. Last consultation on 10/08/2015
Crofts J, Lenguerrand E, Bentham G et al (2016) Prevention of brachial plexus injury-12 years of shoulder dystocia training: an interrupted time-series study. BJOG 123:111–118
Spain JE, Frey HA, Tuuli MG, Colvin R, Macones GA, Cahill AG (2015) Neonatal morbidity associated with shoulder dystocia maneuvers. Am J Obstet Gynecol 212:353.e1–353.e5
Lima S, Chauleur C, Varlet MN et al (2009) La dystocie des épaules: analyse descriptive sur dix années dans une maternité de niveau III [Shoulder dystocia: a ten-year descriptive study in a level-III maternity unit]. Gynecol Obstet Fertil 37:300–306
Revicky V, Mukhopadhyay S, Morris EP, Nieto JJ (2012) Can we predict shoulder dystocia? Arch Gynecol Obstet 285:291–295
Collin A, Dellis X, Ramanah R et al (2008) La dystocie vraie des épaules: analyse de 14 cas traités par la manœuvre de Jacquemier [Severe shoulder dystocia: study of 14 cases treated by Jacquemier’s maneuver]. J Gynecol Obstet Biol Reprod 37:283–290
Noblot E, Raia-Barjat T, Lajeunesse C et al (2015) Training program for the management of two obstetric emergencies within a French perinatal care network. Eur J Obstet Gynecol Reprod Biol 189:101–105
Sentinel Event Alert Issue 30 (2004) Preventing infant death and injury during delivery. Joint Commission on Accreditation of Healthcare Organizations, Washington, 2004. http://www.jointcommission.org/sentinel_event_alert_issue_30_preventing_infant_death_and_injury_during_delivery/. Last consultation on 10/07/2015
Clinical Negligence Scheme for Trusts (2011) Maternity clinical risk management standards, version 1: National Health Service (UK), Ligitation Authority, 2013. http://www.nhsla.com/Pages/Publications.aspx?library=safety|standards. Last consultation on 10/07/2015
Inglis SR, Feier N, Chetiyaar JB et al (2011) Effects of shoulder dystocia training on the incidence of brachial plexus injury. Am J Obstet Gynecol 204(322):e1–e6
Acknowledgments
We wish to thank Mrs. Severine Besson and Mrs. Catherine Sergueenkoff for their contributions to a standardized description of SD management in patient’s medical data. We are also grateful to the midwives and obstetricians who worked in our labor ward for their contributions to everyday data collection.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest. The authors have full control of all primary data and they agree to allow the journal to review their data if requested.
Rights and permissions
About this article
Cite this article
Gachon, B., Desseauve, D., Fritel, X. et al. Is fetal manipulation during shoulder dystocia management associated with severe maternal and neonatal morbidities?. Arch Gynecol Obstet 294, 505–509 (2016). https://doi.org/10.1007/s00404-016-4013-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-016-4013-1