Abstract
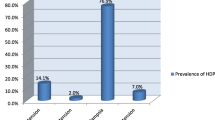
Objective: The aim of the study was to determine the risk factors, prevalance, epidemiological parameters and maternal-perinatal outcome in pregnant women with hypertensive disorder. Materials and methods: A retrospective analysis was undertaken on 255 consecutive cases of hypertensive disorder in pregnancy who were managed at Kocaeli University, School of Medicine, Department of Obstetrics and Gynecology from June 1997 to November 2004. Demographic data involving age, parity, gestational week, clinical and laboratory findings were recorded from the medical files. Additionally delivery route, indications of cesarean section, fetal and maternal complications were determined. Statistical analysis was performed by SPSS programme using Kruskal Wallis nonparametric test, ANOVA (Analysis of variance) and chi-square tests. Results: Of 5,155 deliveries in our clinic during the defined period, 438 cases (8.49%) were managed as hypertensive disorder of pregnancy. Medical records of 255 cases could be avaliable. Of 255 cases, 138 patients (54.11%) were found to have severe preeclampsia while 88 cases (34.50%) were diagnosed as mild preeclampsia. Twenty-nine patients (11.37%) were suffering from chronic hypertension. Of 138 severely preeclamptic cases, 28 cases (11%) had eclamptic convulsion and another 28 patients (11%) were demonstrated to have HELLP syndrome. Intrauterine growth restriction, oligohydramnios, placental ablation were the obstetric complications in 75 (29.4%), 49 (19.2%), 19 (7.5%) cases, respectively. Additionally multiple pregnancy and gestational diabetes mellitus were noted in 5.9% (n:15) and 3.9% (n:10) of the patients. Delivery route was vaginal in 105 patients (41.2%) while 150 patients (58.8%) underwent cesarean section with the most frequent indication to be fetal distress in 69 cases (46%). Cesarean section rate seemed to be the lowest (48.3%) in chronic hypertensive women while the highest (63.8%) in severe preeclamptic patients. Maternal mortality occured in 3 cases (1.2%) and all of those cases were complicated with HELLP syndrome. Intracranial bleeding was the cause of maternal death in one case while the other two cases were lost due to acute renal failure and disseminated intravascular coagulation, respectively. Intrauterine fetal demise was recorded in 24 cases on admission. Ten fetuses died during the intrapartum period. Mean gestational age and birth weight were 28±3.5 and 1000±416 g, respectively in this group. In these ten women, five cases were diagnosed as HELLP syndrome, two were severely preeclamptic and three were eclamptic. Perinatal mortality rate was found to be 144/1,000 births Conclusion: Hypertensive disorder of pregnancy is associated with increased risk of maternal-perinatal adverse outcome. The complications of severe preeclampsia and eclampsia could be prevented by more widespread use of prenatal care, education of primary medical care personnel, prompt diagnosis of high-risk patients and timely referral to tertiary medical centers.
Similar content being viewed by others
References
Aali BS, Ghafoorian J, Mohamed-Alizadeh S (2004) Severe preeclampsia and eclampsia in Kerman, Iran: complications and outcomes. Med Sci Monit 10(4):163–167
Al-Ghamdi Saeed MG, Al-Harbi AS, Khalil A, El-Yahya AR (1999) Hypertensive disorders of pregnancy: prevalance, classification and adverse outcomes in northwestern Saudi Arabia. Ann Saudi Med J 6:557–560
American College of Obstetricians and Gynecologists (2002) Diagnosis and management of preeclampsia and eclampsia. American College of Obstetricians and Gynecologists (ACOG) Practice Bulletin no: 33. Int J Gynecol Obstet 77:67–75
Chames MC, Livingston JC, Ivester TS, Barton JR, Sibai BM (2002) Late postpartum eclampsia: a preventable disease? Am J Obstet Gynecol 186:1174–1177
Coppage KH, Polzin WJ (2002) Severe preeclampsia and delivery outcomes: is immediate cesarean delivery beneficial? Am J Obstet Gynecol 186:921–923
Diejomaoh FME, Omu AE, Al-Busiri N, Taher S, Al-Othman S, Fatinikun T, Fernandes S (2004) Nitric oxide production is not altered in preeclampsia. Arch Gynecol Obstet 269:237–243
Duley L (2003) Pre-eclampsia and the hypertensive disorders of pregnancy. Br Med Bull 67:161–176
Foy R, Ramsay CR, Grimshaw JM, Penney GC, Vale L, Thomson A, Greer IA (2004) The impact of guidelines on mild hypertension in pregnancy: time series analysis. BJOG 111:765–770
Gaio DS, Schmidt MI, Duncan BB, Nucci LB, Matos MC, Branchtein L (2001) Hypertensive disorders in pregnancy: frequency, and associate factors in a cohort of Brazilian women. Hypertens Pregnancy 20:269–281
Geary M (1997) The HELLP syndrome. Br J Obstet Gynecol 104(8):887–891
Gofton EN, Capewell V, Natale R, Gratton RJ (2001) Obstetrical intervention rates and maternal and neonatal outcomes of women with gestational hypertension. Am J Obstet Gynecol 185:798–803
Hanisch CG, Pfeiffer KA, Harald Schlebusch H, Schmolling J (2004) Adhesion molecules, activin and inhibin- candidates for the biochemical prediction of hypertensive diseases in pregnancy? Arch Gynecol Obstet 270:110–115
Hernandez R, Lopez JL (2001) Preeclampsia and eclampsia: experience at the Cento Medic Nacional de Terreon. Ginecol Obstet Mex 69:341–345
Isler CM, Rinehart BK, Terrone DA, Martin PW; Magann EF, Martin JN (2000) Maternal mortality associated with HELLP (hemolysis, elevated liver enzymes, and low platelets) syndrome. Am J Obstet Gynecol 183(2):444–448
Katz VL, Farmer R, Kuller JA (2000) Preeclampsia into eclampsia: toward a new paradigm. Am J Obstet Gynecol 182:1389–1396
Kullberg G, Lindeberg S, Hanson U (2002) Eclampsia in Sweden. Hypertens Pregnancy 21(1):13–21
Kuschel B, Zimmermann A, Schneider KTM, Fischer T (2004) Prolongation of pregnancy following eclampsia. Eur J Obstet Gynecol Reprod Biol 113:245–247
Lee W, O’Connell CM, Basket TF (2004) Maternal and perinatal outcomes of eclampsia: Nova Scotia, 1981–2000. J Obstet Gynaecol Can 26(2):119–123
Livingston CJ, Sibai BM (2001) Chronic hypertension in pregnancy. Obstet Gynecol Clin North Am 28:447–463
Matthys LA, Coppage KH, Lambers DS, Barton JR, Sibai BM (2004) Delayed postpartum preeclampsia: an experience of 151 cases. Am J Obstet Gynecol 190:1464–1466
McCowan LM, Buist RG, North RA, Gamble G (1996) Perinatal morbidity in chronic hypertension. Br J Obstet Gynaecol 103:123–129
National High Blood Pressure Education Program Working Group (2000) Report of the National High Blood Pressure Education Program Working Group on high blood pressure in pregnancy. Am J Obstet Gynecol 183:S1–S22
Nisell H, Palm K, Wolff K (2000) Prediction of maternal and fetal complications in preeclampsia. Acta Obstet Gynecol Scand 79:19–23
Sawhney H, Aggarwal N, Biswas R (2000) Maternal mortality associated with eclampsia and preeclampsia of pregnancy. J Obstet Gynecol Res 26(5):351–356
Serdar S, Gür E, Çolakoğulları M, Develioğlu O, Sarandöl E (2003) Lipid and protein oxidation and antioxidant function in women with mild and severe preeclampsia. Arch Gynecol Obstet 268:19–25
Sibai BM (1996) Hypertension in pregnancy. In: Gabbe SG, Niebyl JR, Simpson JL (eds) Obstetrics: normal and problem pregnancies, 3rd edn. Churchill Livingston, New York, pp 935–996
Tranquilli AL, Giannibulo SR (2004) The weight of fetal growth restriction in 437 hypertensive pregnancies. Arch Gynecol Obstet 270:214–16
Ventura SJ, Martin JA, Cortin SG, Mathews TJ, Park MM (2000) Births: final data for 1998 national vital statistics. Reports 48 (No.3)
Vigil-De Gracia P, Montufar-Rueda C, Ruiz J (2003) Expectant management of severe preeclampsia and preeclampsia superimposed on chronic hypertension between 24 and 34 weeks’ gestation. Eur J Obstet Gynecol Reprod Biol 107:24–27
Walker JJ (2000) Preeclampsia. Baillieres Best Pract Res Clin Obstet Gynecol 14(1):57–71
Xiong X, FraserWD (2004) Impact of pregnancy-induced hypertension on birth weight by gestational age. Ped Perinatal Epidemiol 18:186–191
Zarean Z (2004) Hypertensive disorders of pregnancy. Int J Gynecol Obstet 87:194–198
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yücesoy, G., Özkan, S., Bodur, H. et al. Maternal and perinatal outcome in pregnancies complicated with hypertensive disorder of pregnancy: a seven year experience of a tertiary care center. Arch Gynecol Obstet 273, 43–49 (2005). https://doi.org/10.1007/s00404-005-0741-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-005-0741-3