Abstract
Background
Cortical thickness and porosity are two main determinants of cortical bone strength. Thus, mapping variations in these parameters across the full width of the distal end of the clavicle may be helpful for better understanding the basis of distal clavicle fractures and for selecting optimal surgical treatment.
Methods
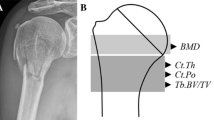
Distal ends of 11 clavicles (6 men, 5 women; age: 81.9 ± 15.1 years) were scanned by micro-computed tomography at 10-µm resolution. We first analyzed cortical thickness and porosity of each 500-μm-wide area across the superior surface of distal clavicle at the level of conoid tubercle in an antero-posterior direction. This level was chosen for detailed evaluation because previous studies have demonstrated its superior microarchitecture relative to the rest of the distal clavicle. Subsequently, we divided the full width of distal clavicle to three subregions (anterior, middle, and posterior) and analyzed cortical porosity, pore diameter, pore separation, and cortical thickness.
Results
We found the largest number of low-thickness and high-porosity areas in the anterior subregion. Cortical porosity, pore diameter, pore separation, and cortical thickness varied significantly among the three subregions (p < 0.001 p = 0.016, p = 0.001, p < 0.001, respectively). Cortex of the anterior subregion was more porous than that of the middle subregion (p < 0.001) and more porous and thinner than that of the posterior subregion (p < 0.001, p = 0.030, respectively). Interaction of site and sex revealed higher porosity of the anterior subregion in women (p < 0.001). The anterior subregion had larger pores than the middle subregion (p = 0.019), whereas the middle subregion had greater pore separation compared with the anterior (p = 0.002) and posterior subregions (p = 0.006). In general, compared with men, women had thinner (p < 0.001) and more porous cortex (p = 0.03) with larger cortical pores (p < 0.001).
Conclusions
Due to high cortical porosity and low thickness, the anterior conoid subregion exhibits poor bone microarchitecture, particularly in women, which may be considered in clinical practice.
Levels of evidence
Level IV.
Graphical abstract



Similar content being viewed by others
Data availability
All the authors decided that the data and material will not be deposited in a public repository.
Code availability
Not applicable.
References
Robinson CM (1998) Fractures of the clavicle in the adult. epidemiology and classification. J Bone Joint Surg Br 80:476–484
Kihlstrom C, Moller M, Lonn K, Wolf O (2017) Clavicle fractures: epidemiology, classification and treatment of 2 422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord 18:82
Postacchini F, Gumina S, De Santis P, Albo F (2002) Epidemiology of clavicle fractures. J Shoulder Elbow Surg 11:452–456
Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE (2004) Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 86:1359–1365
Huttunen TT, Launonen AP, Berg HE, Lepola V, Fellander-Tsai L, Mattila VM (2016) Trends in the Incidence of Clavicle Fractures and Surgical Repair in Sweden: 2001–2012. J Bone Joint Surg Am 98:1837–1842
Ong T, Sahota O, Marshall L (2015) Epidemiology of appendicular skeletal fractures: a cross-sectional analysis of data from the Nottingham Fracture Liaison Service. J Orthop Sci 20:517–521
Gutierrez S (2019) CORR Insights(R): what regions of the distal clavicle have the greatest bone mineral density and cortical thickness? a cadaveric study. Clin Orthop Relat Res 477:2733–2734
Neer CS 2nd (1968) Fractures of the distal third of the clavicle. Clin Orthop Relat Res 58:43–50
Nordqvist A, Petersson C, Redlund-Johnell I (1993) The natural course of lateral clavicle fracture. 15 (11–21) year follow-up of 110 cases. Acta Orthop Scand 64:87–91
Oh JH, Kim SH, Lee JH, Shin SH, Gong HS (2011) Treatment of distal clavicle fracture: a systematic review of treatment modalities in 425 fractures. Arch Orthop Trauma Surg 131:525–533
Chen RE, Soin SP, El-Shaar R, Nicandri GT, Awad HA, Maloney MD, Voloshin I (2019) What regions of the distal clavicle have the greatest bone mineral density and cortical thickness? a cadaveric study. Clin Orthop Relat Res 477:2726–2732
Seebeck J, Goldhahn J, Stadele H, Messmer P, Morlock MM, Schneider E (2004) Effect of cortical thickness and cancellous bone density on the holding strength of internal fixator screws. J Orthop Res 22:1237–1242
Sundh D, Mellström D, Nilsson M, Karlsson M, Ohlsson C, Lorentzon M (2015) Increased cortical porosity in older men with fracture. J Bone Miner Res 30:1692–1700
Cirovic A, Djonic D, Zivkovic V, Nikolic S, Djuric M, Milovanovic P (2020) Three-dimensional microstructural basis for differential occurrence of subcapital versus basicervical hip fractures in men. Calcif Tissue Int 107:240–248
Sundh D, Nilsson AG, Nilsson M, Johansson L, Mellström D, Lorentzon M (2017) Increased cortical porosity in women with hip fracture. J Intern Med 281:496–506
McCalden RW, McGeough JA, Barker MB, Court-Brown CM (1993) Age-related changes in the tensile properties of cortical bone. The relative importance of changes in porosity, mineralization, and microstructure. The Journal of bone and joint surgery. American 75:1193–1205
Pearson AM, Tosteson AN, Koval KJ, McKee MD, Cantu RV, Bell JE, Vicente M (2010) Is surgery for displaced, midshaft clavicle fractures in adults cost-effective? Results based on a multicenter randomized, controlled trial. J Orthop Trauma 24:426–433
Vaishya R, Vijay V, Khanna V (2017) Outcome of distal end clavicle fractures treated with locking plates. Chin J Traumatol 20:45–48
Tan HL, Zhao JK, Qian C, Shi Y, Zhou Q (2012) Clinical results of treatment using a clavicular hook plate versus a T-plate in neer type II distal clavicle fractures. Orthopedics 35:e1191-1197
Zhang C, Huang J, Luo Y, Sun H (2014) Comparison of the efficacy of a distal clavicular locking plate versus a clavicular hook plate in the treatment of unstable distal clavicle fractures and a systematic literature review. Int Orthop 38:1461–1468
Yan HW, Li L, Wang RC, Yang Y, Xie Y, Tang J, Shi ZY (2017) Clinical efficacies of coracoclavicular ligament reconstruction using suture anchor versus hook plate in the treatment of distal clavicle fracture. Orthop Traumatol Surg Res 103:1287–1293
Cirovic A, Cirovic A, Djonic D, Zivkovic V, Nikolic S, Djuric M, Milovanovic P (2020) Three-dimensional microstructural basis for differential occurrence of subcapital versus basicervical hip fractures in men. Calcif Tissue Int 107:240–248
Cirovic A, Jadzic J, Djukic D, Djonic D, Zivkovic V, Nikolic S, Djuric M, Milovanovic P (2022) Increased cortical porosity, reduced cortical thickness, and reduced trabecular and cortical microhardness of the superolateral femoral neck confer the increased hip fracture risk in individuals with type 2 diabetes. Calcif Tissue Int 111:457–465
Cirovic A, Cirovic A, Djukic D, Djonic D, Zivkovic V, Nikolic S, Djuric M, Milovanovic P (2022) Three-dimensional mapping of cortical porosity and thickness along the superolateral femoral neck in older women. Sci Rep 12:15544
Kral R, Osima M, Borgen TT, Vestgaard R, Richardsen E, Bjornerem A (2017) Increased cortical porosity and reduced cortical thickness of the proximal femur are associated with nonvertebral fracture independent of Fracture Risk Assessment Tool and Garvan estimates in postmenopausal women. PLoS ONE 12:e0185363
Iori G, Schneider J, Reisinger A, Heyer F, Peralta L, Wyers C, Grasel M, Barkmann R, Gluer CC, van den Bergh JP, Pahr D, Raum K (2019) Large cortical bone pores in the tibia are associated with proximal femur strength. PLoS ONE 14:e0215405
Gewiess J, Sprecher C, Milz S, Gleich J, Helfen T (2023) Osseous microarchitecture in frequent fracture zones of the distal clavicle. JSES Int 7:98–103
Endo D, Ogami-Takamura K, Imamura T, Saiki K, Murai K, Okamoto K, Tsurumoto T (2020) Reduced cortical bone thickness increases stress and strain in the female femoral diaphysis analyzed by a CT-based finite element method: Implications for the anatomical background of fatigue fracture of the femur. Bone Rep 13:100733
Sobol J, Ptaszyńska-Sarosiek I, Charuta A, Oklota-Horba M, Żaba C, Niemcunowicz-Janica A (2015) Estimation of age at death: examination of variation in cortical bone histology within the human clavicle. Folia Morphol 74:378–388
Acknowledgements
This research was supported by the Science Fund of the Republic of Serbia (IDEAS program, grant no. 7749444, BoFraM project) and by Ministry of Science of the Republic of Serbia (to the Center of Bone Biology as the center of excellence).
Funding
The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
All individuals listed as authors substantially contributed to the design, execution, and analysis of the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no financial or non-financial conflicts of interest.
Ethical approval
Ethics Committee of the Faculty of Medicine University of Belgrade approved the research. The study was conducted in accordance with the 1964 Helsinki Declaration and its subsequent amendments or comparable ethical standards.
Informed consent/consent to participate
N/A.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cirovic, A.V., Cirovic, A.V., Vujacic, M.D. et al. Ex vivo analysis of cortical microarchitecture of the distal clavicle: implications for surgical management of fractures. Arch Orthop Trauma Surg (2024). https://doi.org/10.1007/s00402-024-05345-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00402-024-05345-y