Abstract
Introduction
Intramedullary (IM) nailing is the treatment of choice for femoral shaft fractures, but nonunion rates have been reported to be as high as 12%. Surgical interventions for nonunion involve exchange nailing or plate augmentation. Recently, a combined treatment of exchange nailing and plate augmentation has demonstrated good results, but its comparative effectiveness remains unclear. This study aimed to compare the clinical and radiographic outcomes of three different surgical interventions for atrophic femoral shaft nonunion, and investigate the factors that affect bone healing after reoperation.
Materials and methods
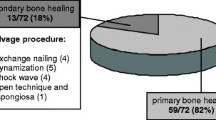
A retrospective study was conducted at five university hospitals involving 149 patients with aseptic atrophic nonunion after IM nailing. These patients underwent reoperation with plate augmentation, exchange nailing, or combined treatment. Clinical and radiographic outcomes were assessed and compared according to reoperation procedure. Logistic regression analysis was performed to identify factors affecting persistent nonunion after reoperation.
Results
Of the cohort, 57 patients underwent plate augmentation, 64 underwent exchange nailing, and 28 received combined treatment. There were no significant differences in patient demographics among the groups. Exchange nailing produced a significantly lower union rate than did the combined treatment (82.8% vs. 100%, p = 0.016), whereas no significant difference was observed in the union rate and time to the union between plate augmentation and the combined treatment. Combined treatment showed the longest operative time and the greatest transfusion requirements. The risk factors for persistent nonunion included age, absence of autogenous bone grafts, and use of an exchange nailing technique.
Conclusions
Exchange nailing as a treatment for atrophic femoral shaft nonunion after IM nailing resulted in a lower union rate. The efficacy of the combined treatment requires further study, and persistent nonunion may be influenced by age, bone grafting, and surgical techniques. A comprehensive approach targeting both biological environment and mechanical stability is crucial in the treatment of atrophic femoral shaft nonunion.


Similar content being viewed by others
Data availability
Data on this research are available from the corresponding author, K-CP, upon reasonable request.
References
Ricci WM, Gallagher B, Haidukewych GJ (2009) Intramedullary nailing of femoral shaft fractures: current concepts. J Am Acad Orthop Surg 17(5):296–305. https://doi.org/10.5435/00124635-200905000-00004
Ricci WM, Bellabarba C, Evanoff B, Herscovici D, DiPasquale T, Sanders R (2001) Retrograde versus antegrade nailing of femoral shaft fractures. J Orthop Trauma 15(3):161–169. https://doi.org/10.1097/00005131-200103000-00003
Wolinsky PR, McCarty E, Shyr Y, Johnson K (1999) Reamed intramedullary nailing of the femur: 551 cases. J Trauma 46(3):392–399. https://doi.org/10.1097/00005373-199903000-00007
Winquist RA, Hansen ST Jr, Clawson DK (1984) Closed intramedullary nailing of femoral fractures. A report of five hundred and twenty cases. J Bone Jt Surg Am 66(4):529–539
Garnavos C (2017) Treatment of aseptic non-union after intramedullary nailing without removal of the nail. Injury 48(Suppl 1):S76-81. https://doi.org/10.1016/j.injury.2017.04.022
Park K, Kim K, Choi YS (2011) Comparison of mechanical rigidity between plate augmentation leaving the nail in situ and interlocking nail using cadaveric fracture model of the femur. Int Orthop 35(4):581–585. https://doi.org/10.1007/s00264-010-0983-y
Vaishya R, Agarwal AK, Gupta N, Vijay V (2016) Plate augmentation with retention of intramedullary nail is effective for resistant femoral shaft non-union. J Orthop 13(4):242–245. https://doi.org/10.1016/j.jor.2016.06.003
Hak DJ, Lee SS, Goulet JA (2000) Success of exchange reamed intramedullary nailing for femoral shaft nonunion or delayed union. J Orthop Trauma 14(3):178–182. https://doi.org/10.1097/00005131-200003000-00005
Bellabarba C, Ricci WM, Bolhofner BR (2001) Results of indirect reduction and plating of femoral shaft nonunions after intramedullary nailing. J Orthop Trauma 15(4):254–263. https://doi.org/10.1097/00005131-200105000-00004
Lai PJ, Hsu YH, Chou YC, Yeh WL, Ueng SWN, Yu YH (2019) Augmentative antirotational plating provided a significantly higher union rate than exchanging reamed nailing in treatment for femoral shaft aseptic atrophic nonunion - retrospective cohort study. BMC Musculoskelet Disord 20(1):127. https://doi.org/10.1186/s12891-019-2514-3
Çimen O, Öner A, Köksal A, Dırvar F, Mert M, Kargın D (2023) A comparison of exchange nailing and plate augmentation over a retained intramedullary nail in aseptic oligotrophic and atrophic femoral shaft pseudoarthrosis. Jt Dis Relat Surg 34(1):121–129. https://doi.org/10.52312/jdrs.2023.788
Khalifa AA, Fadle AA, Elsherif ME et al (2022) Concomitant intramedullary nailing and plate augmentation as a single-stage procedure in treating complicated nonunited femoral shaft fractures. Trauma 24(4):286–293. https://doi.org/10.1177/14604086211007037
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF (2018) Fracture and dislocation classification compendium-2018. J Orthop Trauma 32(1 Suppl):1s–170s. https://doi.org/10.1097/bot.0000000000001063
Weber BG, Brunner C (1981) The treatment of nonunions without electrical stimulation. Clin Orthop Relat Res 161:24–32
Wittauer M, Burch MA, McNally M et al (2021) Definition of long-bone nonunion: a scoping review of prospective clinical trials to evaluate current practice. Injury 52(11):3200–3205. https://doi.org/10.1016/j.injury.2021.09.008
Govaert GAM, Kuehl R, Atkins BL et al (2020) Diagnosing fracture-related infection: current concepts and recommendations. J Orthop Trauma 34(1):8–17. https://doi.org/10.1097/bot.0000000000001614
Gustilo RB, Mendoza RM, Williams DN (1984) Problems in the management of type III (severe) open fractures: a new classification of type III open fractures. J Trauma 24(8):742–746. https://doi.org/10.1097/00005373-198408000-00009
Ru J-y, Chen L-x, Hu F-y et al (2018) Factors associated with development of re-nonunion after primary revision in femoral shaft nonunion subsequent to failed intramedullary nailing. J Orthop Surg Res 13(1):180. https://doi.org/10.1186/s13018-018-0886-y
Cone R, Roszman A, Conway Y, Cichos K, McGwin G, Spitler CA (2023) Risk factors for nonunion of distal femur fractures. J Orthop Trauma 37(4):175–180. https://doi.org/10.1097/bot.0000000000002553
Reichert IL, McCarthy ID, Hughes SP (1995) The acute vascular response to intramedullary reaming. Microsphere estimation of blood flow in the intact ovine tibia. J Bone Jt Surg Br 77(3):490–493
Greksa F, Tóth K, Boros M, Szabó A (2012) Periosteal microvascular reorganization after tibial reaming and intramedullary nailing in rats. J Orthop Sci 17(4):477–483. https://doi.org/10.1007/s00776-012-0222-z
Clark D, Nakamura M, Miclau T, Marcucio R (2017) Effects of aging on fracture healing. Curr Osteoporos Rep 15(6):601–608. https://doi.org/10.1007/s11914-017-0413-9
Nicholson JA, Makaram N, Simpson A, Keating JF (2021) Fracture nonunion in long bones: a literature review of risk factors and surgical management. Injury 52(2 Suppl):3s–11s. https://doi.org/10.1016/j.injury.2020.11.029
Jhunjhunwala HR, Dhawale AA (2016) Is augmentation plating an effective treatment for non-union of femoral shaft fractures with nail in situ? Eur J Trauma Emerg Surg 42(3):339–343. https://doi.org/10.1007/s00068-015-0534-8
Jones CB, Mayo KA (2005) Nonunion treatment: iliac crest bone graft techniques. J Orthop Trauma 19(10 Suppl):S11-13. https://doi.org/10.1097/00005131-200511101-00004
Myeroff C, Archdeacon M (2011) Autogenous bone graft: donor sites and techniques. J Bone Jt Surg Am 93(23):2227–2236. https://doi.org/10.2106/jbjs.J.01513
Grundnes O, Reikerås O (1993) Effects of instability on bone healing. Femoral osteotomies studied in rats. Acta Orthop Scand 64(1):55–58. https://doi.org/10.3109/17453679308994529
Mølster AO (1984) Effects of rotational instability on healing of femoral osteotomies in the rat. Acta Orthop Scand 55(6):632–636. https://doi.org/10.3109/17453678408992411
Walcher MG, Day RE, Gesslein M, Bail HJ, Kuster MS (2023) Augmentative plating versus exchange intramedullary nailing for the treatment of aseptic non-unions of the femoral shaf—a biomechanical study in a SawboneTM model. J Pers Med 13(4):650
Rupp M, Biehl C, Budak M, Thormann U, Heiss C, Alt V (2018) Diaphyseal long bone nonunions—types, aetiology, economics, and treatment recommendations. Int Orthop 42(2):247–258. https://doi.org/10.1007/s00264-017-3734-5
Quan K, Xu Q, Zhu M, Liu X, Dai M (2021) Analysis of risk factors for non-union after surgery for limb fractures: a case-control study of 669 subjects. Front Surg 8:754150. https://doi.org/10.3389/fsurg.2021.754150
Funding
No funding or other support was offered or received from any organization.
Author information
Authors and Affiliations
Contributions
C-WO, O-JS, Joon-Woo Kim, Ji-Wan Kim, and KTH contributed to the study conception and design. IK organized and interpreted the data, wrote the manuscript, and performed the statistical analysis. C-WO, O-JS, Joon-Woo Kim, Ji-Wan Kim, and KTH contributed in the revision process. K-CP conceptualized the study and participated in its design and helped to modify the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was obtained from the ethics committee of Hanyang university Guri hospital (Approval no.: 2023-02-030).
Informed consent
Informed consent was waived due to the retrospective study design.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kook, I., Oh, CW., Shon, OJ. et al. Comparing outcomes of plate augmentation, nail exchange, and nail exchange with plate augmentation in the treatment of atrophic femoral shaft nonunion after intramedullary nailing: a multicenter retrospective study. Arch Orthop Trauma Surg 144, 1259–1268 (2024). https://doi.org/10.1007/s00402-023-05183-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05183-4