Abstract
Purpose
This study aimed to identify factors associated with poorer patient outcomes for lumbar decompression and/or discectomy (PLDD).
Methods
We extracted data from the Hospital Episodes Statistics database for the 5 years from 1st April 2014 to 31st March 2019. Patients undergoing an elective one- or two-level PLDD aged ≥ 17 years and without evidence of revision surgery during the index stay were included. The primary patient outcome measure was readmission within 90 days post-discharge.
Results
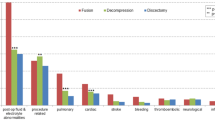
Data for 93,813 PLDDs across 111 hospital trusts were analysed. For the primary outcome, greater age [< 40 years vs 70–79 years odds ratio (OR) 1.28 (95% confidence interval (CI) 1.14 to 1.42), < 40 years vs ≥ 80 years OR 2.01 (95% CI 1.76–2.30)], female sex [OR 1.09 (95% CI 1.02–1.16)], surgery over two spinal levels [OR 1.16 (95% CI 1.06–1.26)] and the comorbidities chronic pulmonary disease, connective tissue disease, liver disease, diabetes, hemi/paraplegia, renal disease and cancer were all associated with emergency readmission within 90 days. Other outcomes studied had a similar pattern of associations.
Conclusions
A high-throughput PLDD pathway will not be suitable for all patients. Extra care should be taken for patients aged ≥ 70 years, females, patients undergoing surgery over two spinal levels and those with specific comorbidities or generalised frailty.


Similar content being viewed by others
Availability of data and materials
This report does not contain patient identifiable data. The data in this report are anonymised. Request for any underlying data cannot be granted as the data are calculated from data under licence/data sharing agreement from NHS Digital and/or other data provider where conditions of use (and further use) apply. The data can be obtained from NHS Digital upon request.
Availability of code
Data were analysed using the Stata software. The code used in the analysis was relatively trivial, but can be made available by the authors upon request.
References
NHS England (2022) Delivery plan for tackling the COVID-19 backlog of elective care. NHS England, London
Howlett NC, Wood RM (2022) Modeling the Recovery of Elective Waiting Lists Following COVID-19: Scenario Projections for England. Value Health 25(11):1805–1813. https://doi.org/10.1016/j.jval.2022.06.016
NHS England and NHS Improvement: Delivery plan for tackling the COVID-19 backlog of elective care (2022) https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2022/02/C1466-delivery-plan-for-tackling-the-covid-19-backlog-of-elective-care.pdf. Accessed 14 Sep 2023
Gray WK, Day J, Briggs TWR, Hutton M (2022) Safety of same-day discharge posterior lumbar decompression and/or discectomy: an observational study using administrative data from England. Global Spine J. https://doi.org/10.1177/21925682221131764
NHS Digital (2018) Hospital Episode Statistics (HES) Analysis Guide. NHS Digital, London
NHS England (2021) 2021/22 National Tariff Payment System. NHS England, London
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40(5):373–383. https://doi.org/10.1016/0021-9681(87)90171-8
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P et al (2011) Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol 173(6):676–682. https://doi.org/10.1093/aje/kwq433
Gilbert T, Neuburger J, Kraindler J, Keeble E, Smith P, Ariti C et al (2018) Development and validation of a Hospital Frailty Risk Score focusing on older people in acute care settings using electronic hospital records: an observational study. Lancet 391(10132):1775–1782. https://doi.org/10.1016/S0140-6736(18)30668-8
Westreich D, Greenland S (2013) The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. Am J Epidemiol 177(4):292–298. https://doi.org/10.1093/aje/kws412
Getting It Right First Time programme: High Volume, Low Complexity (HVLC) Surgery (2022). https://www.gettingitrightfirsttime.co.uk/bpl/hvlc/. Accessed 14 Sep 2023
Murphy ME, Gilder H, Maloney PR, McCutcheon BA, Rinaldo L, Shepherd D et al (2017) Lumbar decompression in the elderly: increased age as a risk factor for complications and nonhome discharge. J Neurosurg Spine 26(3):353–362. https://doi.org/10.3171/2016.8.SPINE16616
Gruskay JA, Fu M, Bohl DD, Webb ML, Grauer JN (2015) Factors affecting length of stay after elective posterior lumbar spine surgery: a multivariate analysis. Spine J 15(6):1188–1195. https://doi.org/10.1016/j.spinee.2013.10.022
Ali R, Schwalb JM, Nerenz DR, Antoine HJ, Rubinfeld I (2016) Use of the modified frailty index to predict 30-day morbidity and mortality from spine surgery. J Neurosurg Spine 25(4):537–541. https://doi.org/10.3171/2015.10.SPINE14582
Shabat S, Arinzon Z, Gepstein R, Folman Y (2011) Long-term follow-up of revision decompressive lumbar spinal surgery in elderly patients. J Spinal Disord Tech 24(3):142–145. https://doi.org/10.1097/BSD.0b013e3181de4b61
Gerhardt J, Bette S, Janssen I, Gempt J, Meyer B, Ryang YM (2018) Is eighty the new sixty? Outcomes and complications after lumbar decompression surgery in elderly patients over 80 years of age. World Neurosurg 112:e555–e560. https://doi.org/10.1016/j.wneu.2018.01.082
Glassman SD, Carreon LY, Dimar JR, Campbell MJ, Puno RM, Johnson JR (2007) Clinical outcomes in older patients after posterolateral lumbar fusion. Spine J 7(5):547–551. https://doi.org/10.1016/j.spinee.2006.11.003
Hutton M (2019) Spinal services: GIRFT Programme National Specialty Report. GIRFT/NHS England and NHS Improvement, London
Hardy F, Heyl J, Tucker K, Hopper A, Marcha MJ, Briggs TWR et al (2022) Data consistency in the English Hospital Episodes Statistics database. BMJ Health Care Inform 29(1):e100633. https://doi.org/10.1136/bmjhci-2022-100633
Acknowledgements
The authors acknowledge The UK ONS and NHS Digital for permission to use their data in this report. They also thank all staff within individual NHS trusts who collected and entered the data used in this study.
Funding
Johannes Heyl and Flavien Hardy conducted this work as part of a fellowship from Distributed Research utilising Advanced Computing (DiRAC), which is funded by the Science and Technology Facilities Council (grant numbers ST/S003916/1 and ST/W002760/1).
Author information
Authors and Affiliations
Contributions
This study was designed and organised by JH, FH, MH, MM, KT, JM, TWRB and WKG. Data cleaning, analysis and writing of the first draft was by JH supported by FH and WKG. All authors critically reviewed the manuscript and agreed to submission of the final draft.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest.
Consent to participate
Informed consent was not sought for the present study because it was an analysis of routine clinical data.
Ethical approval
Ethical approval was not sought for the present study because it did not directly involve human participants. This study was completed in accordance with the Helsinki Declaration as revised in 2013.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Heyl, J., Hardy, F., Gray, W.K. et al. Factors associated with poorer outcomes for posterior lumbar decompression and or/or discectomy: an exploratory analysis of administrative data. Arch Orthop Trauma Surg 144, 1129–1137 (2024). https://doi.org/10.1007/s00402-023-05182-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05182-5