Abstract
Purpose
The purpose of this study was to evaluate the reproducibility and the accuracy of distal tibiofibular syndesmosis (DTFS) as landmark to perform controlled varus tibial resections during total knee arthroplasty (TKA). The hypothesis was that DTFS can be used to perform an accurate 3° varus tibial cut.
Methods
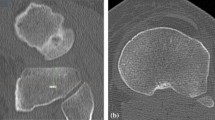
A retrospective analysis on a consecutive series of standard weightbearing full-length anteroposterior views of the lower limbs radiographic images was conducted. For each radiograph, the hip–knee–ankle (HKA) angle, the angle between the tibial mechanical axis and the line connecting the centre of the tibial spines and the DTFS (tibiofibular angle, TFA) and the medial proximal tibial angle (MPTA) were calculated. Each measurement was carried out twice by three independent observers, and intra- and inter-observer measurement reliability were assessed using the intraclass correlation coefficient (ICC) analysis.
Results
A total of 1296 lower limbs were analysed from a series of 648 weightbearing full-length anteroposterior radiographs. The ICC were > 90% for all measurements. The mean TFA value was 2.94 ± 0.68 (range 2.38–3.51). No differences were detected comparing the mean TFA value on the right and left limb (p = 0.795) as well as comparing the values in male and female patients (p = 0.691). Linear regression analysis did not find statistically significant correlation between TFA and MPTA, or TFA and HKA angles, respectively.
Conclusion
The distal tibiofibular syndesmosis is a reliable and easy reproducible radiographic landmark that can be used when planning a 3° varus tibial cut. Future studies are needed to confirm the validity of this method also in clinical settings.
Level of evidence
IV, retrospective case series.



Similar content being viewed by others
Availability of data and materials
All radiographic images used for this study are available in the database of the promoter center. This database can be consulted only by licensed physicians.
Code availability
Not applicable.
References
Rivière C, Iranpour F, Auvinet E, Howell S, Vendittoli PA, Cobb J, Parratte S (2017) Alignment options for total knee arthroplasty: a systematic review. Orthop Traumatol Surg Res 103(7):1047–1056. https://doi.org/10.1016/j.otsr.2017.07.010
Evans JT, Walker RW, Evans JP, Blom AW, Sayers A, Whitehouse MR (2019) How long does a knee replacement last? A systematic review and meta-analysis of case series and national registry reports with more than 15 years of follow-up. Lancet 393(10172):655–663. https://doi.org/10.1016/S0140-6736(18)32531-5
Nam D, Nunley RM, Barrack RL (2014) Patient dissatisfaction following total knee replacement: a growing concern? Bone Jt J 96(11 Suppl A):96–100. https://doi.org/10.1302/0301-620X.96B11.34152
Bellemans J, Colyn W, Vandenneucker H, Victor J (2012) The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res 470(1):45–53. https://doi.org/10.1007/s11999-011-1936-5
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27(5):1394–1402. https://doi.org/10.1007/s00167-019-05509-z
Kim YH, Park JW, Kim JS, Park SD (2014) The relationship between the survival of total knee arthroplasty and postoperative coronal, sagittal and rotational alignment of knee prosthesis. Int Orthop 38(2):379–385. https://doi.org/10.1007/s00264-013-2097-9
Wong J, Steklov N, Patil S, Flores-Hernandez C, Kester M, Colwell CW Jr, D’Lima DD (2011) Predicting the effect of tray malalignment on risk for bone damage and implant subsidence after total knee arthroplasty. J Orthop Res 29(3):347–353. https://doi.org/10.1002/jor.21221
Berend ME, Ritter MA, Meding JB, Faris PM, Keating EM, Redelman R, Faris GW, Davis KE (2004) Tibial component failure mechanisms in total knee arthroplasty. Clin Orthop Relat Res 428:26–34. https://doi.org/10.1097/01.blo.0000148578.22729.0e
van Hamersveld KT, Marang-van de Mheen PJ, Nelissen RGHH (2019) The effect of coronal alignment on tibial component migration following total knee arthroplasty: a cohort study with long-term radiostereometric analysis results. J Bone Jt Surg Am 101(13):1203–1212. https://doi.org/10.2106/JBJS.18.00691
Teeter MG, Naudie DD, McCalden RW, Yuan X, Holdsworth DW, MacDonald SJ (2018) Lanting BA (2018) Varus tibial alignment is associated with greater tibial baseplate migration at 10 years following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 26(6):1610–1617. https://doi.org/10.1007/s00167-017-4765-6
Parratte S, Pagnano MW, Trousdale RT, Berry DJ (2010) Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Jt Surg Am 92(12):2143–2149. https://doi.org/10.2106/JBJS.I.01398
Jeffery RS, Morris RW, Denham RA (1991) Coronal alignment after total knee replacement. J Bone Jt Surg Br 73(5):709–714. https://doi.org/10.1302/0301-620X.73B5
Park JK, Seon JK, Cho KJ, Lee NH, Song EK (2018) Is immediate postoperative mechanical axis associated with the revision rate of primary total knee arthroplasty? A 10-year follow-up study. Clin Orthop Surg 10(2):167–173. https://doi.org/10.4055/cios.2018.10.2.167
Perillo-Marcone A, Taylor M (2007) Effect of varus/valgus malalignment on bone strains in the proximal tibia after TKR: an explicit finite element study. J Biomech Eng 129(1):1–11. https://doi.org/10.1115/1.2401177
Faschingbauer M, Hacker S, Seitz A, Dürselen L, Boettner F, Reichel H (2021) The tibial cut in total knee arthroplasty influences the varus alignment, the femoral roll-back and the tibiofemoral rotation in patients with constitutional varus. Knee Surg Sports Traumatol Arthrosc 29(2):641–651. https://doi.org/10.1007/s00167-020-05996-5
Batailler C, Swan J, Sappey Marinier E, Servien E, Lustig S (2020) New technologies in knee arthroplasty: current concepts. J Clin Med 10(1):47. https://doi.org/10.3390/jcm10010047
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, STROBE Initiative (2014) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg 12(12):1495–1499. https://doi.org/10.1016/j.ijsu.2014.07.013
General Assembly of the World Medical Association (2014) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. J Am Coll Dent 81(3):14–18
Amin A, Janney C, Sheu C, Jupiter DC, Panchbhavi VK (2019) Weight-bearing radiographic analysis of the tibiofibular syndesmosis. Foot Ankle Spec 12(3):211–217. https://doi.org/10.1177/1938640018766631
Kaloo RA, Khurshid N (2019) Study of correlation of length of the tibia with dimensions of the distal articular surfaces of the tibia. Int J Cont Med Res 6(9):I1-3
Akinmokun OI, Ibeabuchi NM (2020) Anthropometric study of adult tibia bone for pre-operative determination of length of intramedullary nail. East Afr Orthop J 14:14–21
Banerjee M, Samanta C, Sangram S, Hota M, Kundu P, Mondal M, Ghosh R, Majumdar S (2015) Estimation of human height from the length of tibia. Indian J Basic Appl Med Res 5(1):30–47
Holland TD (1992) Estimation of adult stature from fragmentary tibias. J Forensic Sci 37(5):1223–1229
Chibba K, Bidmos MA (2007) Using tibia fragments from South Africans of European descent to estimate maximum tibia length and stature. Forensic Sci Int 169(2–3):145–151. https://doi.org/10.1016/j.forsciint.2006.08.011
Tew M, Waugh W (1985) Tibiofemoral alignment and the results of knee replacement. J Bone Jt Surg (Br) 67(4):551–556. https://doi.org/10.1302/0301-620X.67B4.4030849
Simmons ED Jr, Sullivan JA, Rackemann S, Scott RD (1991) The accuracy of tibial intramedullary alignment devices in total knee arthroplasty. J Arthroplasty 6(1):45–50. https://doi.org/10.1016/s0883-5403(06)80156-7
Scuderi GR, Insall JN (1992) Total knee arthroplasty. Current clinical perspectives. Clin Orthop Relat Res 276:26–32
Schneider M, Heisel C, Aldinger PR, Breusch SJ (2007) Use of palpable tendons for extramedullary tibial alignment in total knee arthroplasty. J Arthroplasty 22(2):219–226. https://doi.org/10.1016/j.arth.2006.04.023
Dalury DF, Aram LJ (2016) The “midsulcus line” as a landmark for tibial resection during total knee arthroplasty. Knee 23(3):529–531. https://doi.org/10.1016/j.knee.2016.01.019
Liu MY, Wang HB, Liu SW, Zhang GP, Liu JG, Yang C (2020) Three-point method to guide the tibial resection and component placing in total knee arthroplasty. Orthop Surg 12(3):861–868. https://doi.org/10.1111/os.12693
Nishikawa K, Mizu-uchi H, Okazaki K, Matsuda S, Tashiro Y, Iwamoto Y (2015) Accuracy of proximal tibial bone cut using anterior border of tibia as bony landmark in total knee arthroplasty. J Arthroplasty 30(12):2121–2124. https://doi.org/10.1016/j.arth.2015.06.055
Gong T, Wang R, Gong S, Han L, Yi Y, Wang Y, Xu W (2022) A coronal landmark for tibial component positioning with anatomical alignment in total knee arthroplasty: a radiological and clinical study. Front Surg 9:847987. https://doi.org/10.3389/fsurg.2022.847987
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
SP was involved in concept and study design, data collection and statistical analysis; GGC was involved in manuscript writing and figures preparation, AR was involved in manuscript writing, PH, RT-C, JS-S were involved in data collection, RM-A was involved in study design and statistical analysis, JCM was involved in final revision and language editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of University of Barcelona (TIB-FIB-01).
Consent to participate
Informed consent was not obtained from participants included in the study, because all radiographic examinations were obtained for medical reasons not related to this study.
Consent to publish
All participants provided consent for anonymous publication of the radiographic images.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Perelli, S., Costa, G.G., Russo, A. et al. The distal tibiofibular syndesmosis is a reliable landmark for 3° varus tibial resection in total knee arthroplasty: a radiological evaluation on 1296 cases. Arch Orthop Trauma Surg 144, 879–885 (2024). https://doi.org/10.1007/s00402-023-05099-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-05099-z