Abstract
Introduction
Tranexamic acid (TXA) has been widely utilized to reduce blood loss and allogeneic transfusions in patients who undergo lower limb arthroplasty. In recent years, there have been several articles reporting the incidence of periprosthetic joint infection (PJI) as a primary outcome of TXA administration, but no meta-analysis has been conducted to date. The present systematic review and meta-analysis evaluated the efficacy of TXA administration in preventing PJI and surgical site infection (SSI).
Materials and methods
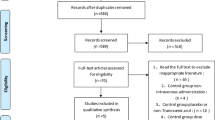
Pubmed, CINAHL, and the Cochrane Library bibliographic databases were searched for studies published by May 24, 2022, that evaluated the effects of TXA on PJI and SSI. Two researchers screened the identified studies based on the PRISMA flow diagram. The quality of each randomized clinical trial was assessed using Version 2 of the Cochrane risk-of-bias tool for randomized trials (ROB2.0), and the quality of cohort and case–control studies was assessed by risk of bias for nonrandomized studies (ROBANS-I).
Results
Of the 2259 articles identified from the database search, 31 were screened and selected. Treatment with TXA significantly reduced the incidence of overall infection, including PJI, SSI, and other infections (OR 0.55; 95% CI 0.49–0.62) (P < 0.00001), and that of PJI alone (OR 0.53; 95% CI 0.47–0.59) (P < 0.00001). TXA reduced the incidence of overall infection in patients who underwent total hip arthroplasty (THA; OR 0.51; 95% CI: 0.35–0.75) (P = 0.0005) and total knee arthroplasty (TKA; OR 0.55; 95% CI: 0.43–0.71) (P < 0.00001). Intravenous administration of TXA reduced the incidence of overall infection (OR 0.59; 95% CI 0.47–0.75) (P < 0.0001), whereas topical administration did not.
Conclusions
Intravenous administration of TXA reduces the incidence of overall infection in patients undergoing both THA and TKA.
Level of evidence
Level III.










Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, [N.K.], upon reasonable request.
References
Kurtz SM, Lau E, Watson H et al (2012) Economic burden of periprosthetic joint infection in the united states. J Arthroplasty 27:61–65. https://doi.org/10.1016/j.arth.2012.02.022
Kurtz SM, Ong KL, Lau E et al (2010) Prosthetic joint infection risk after TKA in the medicare population. Clinical Orthopaedics and Related Research. Springer, New York, pp 52–56
Ong KL, Kurtz SM, Lau E et al (2009) Prosthetic joint infection risk after total hip arthroplasty in the medicare population. J Arthroplasty 24:105–109. https://doi.org/10.1016/j.arth.2009.04.027
Johns WL, Layon D, Golladay GJ et al (2020) Preoperative risk factor screening protocols in total joint arthroplasty: a systematic review. J Arthroplasty 35:3353–3363. https://doi.org/10.1016/J.ARTH.2020.05.074
Siddiqi A, Forte SA, Docter S et al (2019) Perioperative antibiotic prophylaxis in total joint arthroplasty: a systematic review and meta-analysis. J Bone Joint Surg Am 101:828–842. https://doi.org/10.2106/JBJS.18.00990
Kobayashi N, Kamono E, Maeda K, et al (2021) Effectiveness of diluted povidone-iodine lavage for preventing periprosthetic joint infection: an updated systematic review and meta-analysis. J Orthop Surg Res 16:. https://doi.org/10.1186/S13018-021-02703-Z
Kim JL, Park JH, Han SB et al (2017) Allogeneic blood transfusion is a significant risk factor for surgical-site infection following total hip and knee arthroplasty: a meta-analysis. J Arthroplasty 32:320–325. https://doi.org/10.1016/J.ARTH.2016.08.026
Saleh K, Olson M, Resig S et al (2002) Predictors of wound infection in hip and knee joint replacement: results from a 20 year surveillance program. J Orthop Res 20:506–515. https://doi.org/10.1016/S0736-0266(01)00153-X
Lacko M, Jarčuška P, Schreierova D, Lacková A, Gharaibeh A (2020) Tranexamic acid decreases the risk of revision for acute and delayed periprosthetic joint infection after total knee replacement. Joint Diseases Related Surg 31:8–13
Yazdi H, Klement MR, Hammad M et al (2020) Tranexamic acid is associated with reduced periprosthetic joint infection after primary total joint arthroplasty. J Arthroplasty 35:840–844. https://doi.org/10.1016/j.arth.2019.10.029
Drain NP, Gobao VC, Bertolini DM, Smith C, Shah NB, Rothenberger SD, Dombrowski ME, O’Malley MJ, Klatt BA, Hamlin BR, Urish KL (2020) Administration of tranexamic acid improves long-term outcomes in total knee arthroplasty. J Arthroplasty 35:201–206
Klement MR, Padua FG, Li WT et al (2020) Tranexamic acid reduces the rate of periprosthetic joint infection after aseptic revision arthroplasty. J Bone Joint Surg Am 102:1344–1350. https://doi.org/10.2106/JBJS.19.00925
Hong GJ, Wilson LA, Liu J, Memtsoudis SG (2021) Tranexamic acid administration is associated with a decreased odds of prosthetic joint infection following primary total hip and primary total knee arthroplasty: a national database analysis. J Arthroplasty 36:1109–1113
Lei Y; Xie J; Huang Q; Huang W; Pei F; Journal: Archives of orthopaedic and trauma sur (2021) Is there a role of tranexamic acid in rheumatoid arthritis with total knee arthroplasty? Findings from a multicenter prospective cohort study in China. Arch Orthop Trauma Surg 141:489–496
Prieto HA, Vincent HK, Deen JT et al (2018) Tranexamic acid effectively reduces blood loss and transfusion rates during simultaneous bilateral total knee arthroplasty. J Knee Surg 31:270–276. https://doi.org/10.1055/s-0037-1603333
Mehta NGNGAJDCD (2019) A prospective comparative study between intravenous and intraarticular tranexamic acid administration in decreasing the perioperative blood loss in total knee arthroplasty. J Arthrosc Joint Surg 6:70–73
Yozawa S, Ogawa H, Matsumoto K, Akiyama H (2018) Periarticular injection of tranexamic acid reduces blood loss and the necessity for allogeneic transfusion after total knee arthroplasty using autologous transfusion: a retrospective observational study. J Arthroplasty 33:86–89
Wang J, Wang Q, Zhang X, Wang Q (2017) Intra-articular application is more effective than intravenous application of tranexamic acid in total knee arthroplasty: a prospective randomized controlled trial. J Arthroplasty 32:3385–3389
Yuan X, Li B, Wang Q, Zhang X (2017) Comparison of 3 routes of administration of tranexamic acid on primary unilateral total knee arthroplasty: a prospective, randomized, controlled study. J Arthroplasty 32:2738–2743
Liu KL, Chen IH, Wen SH (2017) Low dose tranexamic acid reduces blood transfusion rate after total knee arthroplasty: a population-based study in Taiwan. J Formos Med Assoc 116:24–31
Tzatzairis TK, Drosos GI, Kotsios SE, Ververidis AN, Vogiatzaki TD, Kazakos KI (2016) Intravenous vs topical tranexamic acid in total knee arthroplasty without tourniquet application: a randomized controlled study. J Arthroplasty 31:2465–2470
Formby PM, Pickett AM, van Blarcum GS et al (2015) The use of intravenous tranexamic acid in patients undergoing total hip or knee arthroplasty: a retrospective analysis at a single military institution. Mil Med 180:1087–1090. https://doi.org/10.7205/MILMED-D-14-00657
Alshryda S, Mason J, Vaghela M et al (2013) Topical (intra-articular) tranexamic acid reduces blood loss and transfusion rates following total knee replacement: a randomized controlled trial (TRANX-K). J Bone Joint Surg 95:1961–1968. https://doi.org/10.2106/JBJS.L.00907
Xu X, Jiang J, Liu W, Li X, Lu H (2019) Application of thromboelastography to evaluate the effect of different routes administration of tranexamic acid on coagulation function in total hip arthroplasty. J Orthop Surg Res 14:430
Xie J, Zhang S, Chen G, Xu H, Zhou Z, Pei F (2019) Optimal route for administering tranexamic acid in primary unilateral total hip arthroplasty: results from a multicenter cohort study. Br J Clin Pharmacol 85:2089–2097
Tavares Sánchez-Monge FJ, Aguado Maestro I, Bañuelos Díaz A et al (2018) Efficacy and safety of the topical application of tranexamic acid in primary cementless hip arthroplasty: prospective, randomised, double-blind and controlled study. Revista Española de Cirugía Ortopédica y Traumatología (English Edition) 62:47–54. https://doi.org/10.1016/j.recote.2017.12.004
Zeng Y, Si HB, Shen B, Yang J, Zhou ZK, Kang PD, Pei FX (2017) Intravenous combined with topical administration of tranexamic acid in primary total hip arthroplasty: a randomized controlled trial. Orthop Surg 9:174–179
Kang JS, Moon KH, Kim BS, Yang SJ (2017) Topical administration of tranexamic acid in hip arthroplasty. Int Orthop 41:259–263
Hsu CH, Lin PC, Kuo FC, Wang JW (2015) A regime of two intravenous injections of tranexamic acid reduces blood loss in minimally invasive total hip arthroplasty: a prospective randomised double-blind study. Bone Joint J 97:905–910
Chen JY, Lo NN, Tay DK, Chin PL, Chia SL, Yeo SJ (2015) Intra-articular administration of tranexamic acid in total hip arthroplasty. J Orthop Surg 23:213–217
Yue C, Kang P, Yang P, Xie J, Pei F (2014) Topical application of tranexamic acid in primary total hip arthroplasty: a randomized double-blind controlled trial. J Arthroplasty 29:2452–2456
Viola J, Gomez MM, Restrepo C et al (2015) Preoperative anemia increases postoperative complications and mortality following total joint arthroplasty. J Arthroplasty 30:846–848. https://doi.org/10.1016/J.ARTH.2014.12.026
Akonjom M, Battenberg A, Beverland D, et al (2019) General Assembly, Prevention, Blood Conservation: Proceedings of International Consensus on Orthopedic Infections. J Arthroplasty 34:S147–S155. https://doi.org/10.1016/J.ARTH.2018.09.065
Greenky M, Gandhi K, Pulido L et al (2012) Preoperative anemia in total joint arthroplasty: Is it associated with periprosthetic joint infection? hip. Clin Orthop Relat Res 470:2695–2701. https://doi.org/10.1007/S11999-012-2435-Z
Spahn DR (2010) Anemia and patient blood management in hip and knee surgery: a systematic review of the literature. Anesthesiology 113:482–495. https://doi.org/10.1097/ALN.0B013E3181E08E97
Myers E, Grady PO, Dolan AM (2004) The influence of preclinical anaemia on outcome following total hip replacement. Arch Orthop Trauma Surg 124:699–701. https://doi.org/10.1007/S00402-004-0754-6
Pulido L, Ghanem E, Joshi A et al (2008) Periprosthetic joint infection: the incidence, timing, and predisposing factors. Clin Orthop Relat Res 466:1710–1715. https://doi.org/10.1007/S11999-008-0209-4
Taeuber I, Weibel S, Herrmann E, et al (2021) Association of intravenous tranexamic acid with thromboembolic events and mortality: a systematic review, meta-analysis, and meta-regression. JAMA Surg 156:. https://doi.org/10.1001/JAMASURG.2021.0884
Cheung E v., Sperling JW, Cofield RH (2008) Infection associated with hematoma formation after shoulder arthroplasty. Clin Orthop Relat Res 466:1363–1367. https://doi.org/10.1007/S11999-008-0226-3
Rohde JM, Dimcheff DE, Blumberg N et al (2014) Health care-associated infection after red blood cell transfusion: a systematic review and meta-analysis. JAMA 311:1317–1326. https://doi.org/10.1001/JAMA.2014.2726
Draxler DF, Yep K, Hanafi G et al (2019) Tranexamic acid modulates the immune response and reduces postsurgical infection rates. Blood Adv 3:1598–1609. https://doi.org/10.1182/bloodadvances.2019000092
Beam E, Osmon D (2018) Prosthetic Joint Infection Update. Infect Dis Clin North Am 32:843–859. https://doi.org/10.1016/J.IDC.2018.06.005
Yi S, Tan J, Chen C et al (2014) The use of pneumatic tourniquet in total knee arthroplasty: a meta-analysis. Arch Orthop Trauma Surg 134:1469–1476. https://doi.org/10.1007/S00402-014-2056-Y
Clarke MT, Longstaff L, Edwards D, Rushton N (2001) Tourniquet-induced wound hypoxia after total knee replacement. J Bone Joint Surg Br 83:40–44. https://doi.org/10.1302/0301-620X.83B1.10795
Martin JG, Cassatt KB, Kincaid-Cinnamon KA, Westendorf DS, Garton AS, Lemke JH (2014) Topical administration of tranexamic acid in primary total hip and total knee arthroplasty. J Arthroplasty 29:889–894
Qunn Jid Lee FWYCB and YCWF (2017) Blood sparing efficacy of oral tranexamic acid in primary total knee arthroplasty: a randomized controlled trial. Knee Surg Relat Res 29:57–62
Lee QJ, Chang WY, Wong YC (2017) Blood-sparing efficacy of oral tranexamic acid in primary total hip arthroplasty. J Arthroplasty 32:139–142
Wu KT, Siu KK, Ko JY, et al (2019) Tranexamic acid reduces total blood loss and inflammatory response in computer-assisted navigation total knee arthroplasty. Biomed Res Int 2019:. https://doi.org/10.1155/2019/5207517
Wu J, Feng S, Chen X, Lv Z, Qu Z, Chen H, Xue C, Zhu M, Guo K, Wu P (2019) Intra-articular injection of tranexamic acid on perioperative blood loss during unicompartmental knee arthroplasty. Med Sci Monit 25:5068–5074
Qiu J, Sun X, Zhang W, Ke X, Yang G, Zhang L (2019) Effect of topical tranexamic acid in total hip arthroplasty patients who receive continuous aspirin for prevention of cardiovascular or cerebrovascular events: a prospective randomized study. Orthop Traumatol Surg Res 105:1327–1332
Steinmetz RG, Luick L, Tkach S et al (2020) Effect of tranexamic acid on wound complications and blood loss in total ankle arthroplasty. Foot Ankle Int 41:1117–1121. https://doi.org/10.1177/1071100720934889
Goh GS, D’Amore T, Lonner JH, Fillingham YA (2021) Tranexamic acid is associated with decreasing the risk of complications in patients undergoing arthroplasty with preoperative coagulopathy. J Arthroplasty 36:3864–3869
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
Not applicable.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Imanishi, K., Kobayashi, N., Kamono, E. et al. Tranexamic acid administration for the prevention of periprosthetic joint infection and surgical site infection: a systematic review and meta-analysis. Arch Orthop Trauma Surg 143, 6883–6899 (2023). https://doi.org/10.1007/s00402-023-04914-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04914-x