Abstract
Objective
This systematic review and meta-analysis compared extramedullary fixation and intramedullary fixation for stable two-part trochanteric femoral fractures (AO type 31-A1) with regards to functional outcomes, complications, and surgical outcomes.
Methods
Embase, Medline, Web of Science, Cochrane Central Register of Controlled Trials, and Google Scholar were searched for randomized controlled trials (RCTs) and observational studies. Effect estimates were pooled across studies using random effects models. Results were presented as weighted risk ratio (RR) or weighted mean difference (MD) with corresponding 95% confidence interval (95% CI).
Results
Five RCTs (397 patients) and 14 observational studies (21,396 patients) were included. No significant differences in functional outcomes, complications, or surgical outcomes were found between extramedullary and intramedullary fixation devices, except for a difference in duration of surgery (MD 14.1 min, CI 5.76–22.33, p < 0.001) and intra-operative blood loss (MD 92.30 mL, CI 13.49–171.12, p = 0.02), favoring intramedullary fixation.
Conclusion
Current literature shows no meaningful differences in complications, surgical, or functional outcomes between extramedullary and intramedullary fixation of stable two-part trochanteric femoral fractures. Both treatment options result in good outcomes. This study implicates that, costs should be taken into account when considering implants or comparing fixation methods in future research.
Similar content being viewed by others
Introduction
Proximal femoral fractures are one of the most common types of fracture in the elderly population worldwide with a global incidence of over 182.5 per 100,000 person-years [1,2,3]. The total annual medical costs associated with proximal femoral fractures are over $50,000 per patient in the U.S or over €20,000 in the Netherlands [4, 5]. Due to an aging population and increased life expectancy worldwide, the burden of these fractures on health care systems is increasing. About half of proximal femoral fractures are trochanteric fractures (AO type 31-A1, A2, or A3) [3]. These can be divided in stable two-part fractures (AO type 31-A1) and unstable fractures (AO type 31-A2 and A3) [6]. Of these fractures, type 31-A1 fractures make up 36% [7].
Various studies suggest that intramedullary fixation is the most appropriate approach for treatment of unstable fractures [8,9,10]. For stable fractures, the implant of choice remains a topic of debate. A plethora of fixation devices for both intramedullary and extramedullary fixation is available and high variability in implant preference exists between countries, hospitals, and even individual surgeons [11].
The use of intramedullary fixation devices in both stable and unstable trochanteric fractures has risen in recent years [12, 13]. Less than 2 decades ago, intramedullary fixation was discouraged as older reviews reported higher risks of revision, reoperation, and other complications [10, 14,15,16]. However, recent studies, that directly compared extramedullary and intramedullary fixation of stable two-part trochanteric fractures and a review of AO type A1–A3 trochanteric fractures reported none to minor differences favoring one of the two fixation types [17,18,19,20,21]. Due to an increased experience, development of new devices, and abolition of devices of lower quality with inferior results, the present-day intramedullary devices result in better results and are no longer inferior to extramedullary devices [22]. However, superiority over extramedullary devices has never been proven.
Therefore, current surgical guidelines, such as the Dutch Guideline for treatment of proximal femoral fractures and United Kingdom’s NICE (National Institute for Health and Care Excellence) guideline, state that due to a lack of difference in effectiveness between extramedullary and intramedullary fixation, the device with the lowest costs (i.e., a sliding hip screw) is preferred [23, 24]. The optimal and most cost-effective treatment remains a topic of debate and the steep increase in the use of intramedullary fixation may be influenced by other factors than only clinical data on complications or outcomes, such as individual preference, training, or geographical differences [12, 25].
As no extensive systematic review and meta-analysis of the literature has been conducted on treatment of, exclusively, stable two-part trochanteric fractures, the aim of this study was to compare extramedullary versus intramedullary fixation for stable two-part trochanteric femoral fractures (AO type 31-A1) only using present-day devices.
Methods
This systematic review and meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guideline [26]. A protocol was developed prior to conducting the current study.
Search strategy and selection criteria
Embase, Pubmed/Medline, Web of Science databases, and the Cochrane Central Register of Controlled Trials (CENTRAL) were initially searched on 22 March 2021 for studies comparing extramedullary and intramedullary fixation of AO type trochanteric fractures. The initial search was updated on 26 September 2022. Online Resource 1 shows the search string used and the search results. After deduplication, two reviewers (LHTN and ACP) independently screened titles and abstracts for eligibility for inclusion. Any disagreement was resolved by consensus. The same two reviewers subsequently conducted the full-text screening of eligible articles.
Studies were included when they presented data (a) published after 1990 of (b) acute (c) AO-OTA 31-A1 trochanteric fractures, (d) comparing intramedullary and extramedullary fixation (e) in patients > 50 years, (f) using currently available devices (an overview of included devices per study is provided in Online Resource 2). Studies were excluded when they (a) presented no original data, (b) did not mention relevant outcomes (e.g. only incidence of fixation with specific devices), (c) were biomechanical, in vitro or cadaveric studies, (d) pathological fractures, (e) bilateral fractures, (f) periprosthetic fractures, (g) were case reports, or (h) did not make distinction between type of fracture or treatment.
Data extraction
All baseline characteristics were independently extracted by two reviewers (LHTN and ACP) using a predefined data extraction sheet and included: first author, publication year, setting, study design, study period, follow-up time, total study population, and study population with type 31-A1 fracture. In addition, patient characteristics were collected including age, sex, implant type, and number of patients treated using extramedullary or intramedullary fixation.
Data were collected for the following outcome measures: functional outcomes: Harris hip score, pain, parker mobility score, and walking ability (cases of unassisted/good walking ability were compared with assisted or no walking ability). Complications: reoperation, non-union, cut-out, peri-implant fracture, conversion to prosthesis, implant/fixation failure, superficial and deep infection, malunion, limb-length discrepancy, heterotopic ossification, osteolysis in fixed implants, and mortality. Surgical outcomes/operation characteristics: operation time, blood loss, bone-healing time, quality of reduction, hospital stay, fluoroscopy time, and costs/cost-effectiveness. All outcomes were included as defined by individual presenting articles.
If case data were not described sufficiently in the full-text or supplementary materials, the authors were contacted by e-mail once. If this approach was unsuccessful, missing data were imputed based on the average standard deviation for the total included population across all studies with no missing data and adjusted for population size. This was done for the standard deviations of Harris hip score in Sevinc et al.[27], the standard deviations of 1-year pain scores by Matre et al. [28], and standard deviations for bone-healing time by Cho et al. [29].
Quality assessment
Two reviewers (LHTN and ACP) independently assessed the methodological quality of all included studies using the risk of bias 2 (RoB 2) tool for assessing risk of bias in randomized trials and MINORS, a methodological index for non-randomized studies [30, 31]. Disagreement was resolved by consensus. The RoB 2 is structured into a fixed set of domains of bias, trial design, conduct, and reporting. Within each domain, a series of signaling questions indicate features that are relevant to risk of bias. A proposed judgement about the risk of bias for each domain is generated by an algorithm, based on the signaling questions. Judgement can be 'Low' or 'High' risk of bias, or can express 'Some concerns’. The MINORS ranges from 0 (poor quality) to 24 (high quality).
Statistical analysis
Data were analyzed using Review Manager (Revman, version 5.3.5). Input in the analysis was sample size, mean, and standard deviation (SD) for continuous outcomes and sample size and number of cases with the specific outcome for binary outcomes. Random effects models were used for measuring treatment effects because of the expected heterogeneity due the inclusion of both RCT and observational studies and comparison of multiple types of devices in different countries and clinical settings. No (age-)adjusted analyses were performed, all data were analyzed as described in the original studies. Treatment effects of the binary outcome measures were pooled using the Cochran–Mantel–Haenszel statistic and are presented as risk ratio (RR) with 95% confidence intervals (CI). Treatment effects of the continuous outcome measures were pooled using the inverse variance weighting method and are presented as mean difference (MD) or standardized mean difference (SMD) with 95% confidence intervals (CI). SMD was used when included studies used different measurement scales for the same variable. All analyses were stratified on study design (randomized controlled trials (RCTs) or observational studies) and were presented as Forest plots. Differences between pooled estimates for the two types of study design were compared using the χ2-test test. Heterogeneity between studies was assessed qualitatively using the Cochran’s Q-test and quantified using the I2 statistic. Statistical significance was assumed using a p value threshold of 0.05. Publication bias was assessed by visual inspection of funnel plots for all studied variables (Online Resource 3).
Results
Search
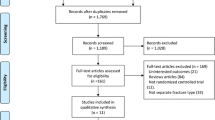
The literature search and selection of included studies is shown in Fig. 1. The primary search resulted in 14,577 records. After deduplication, 7,213 records were screened on title and abstract. Out of the 473 articles assessed for eligibility, a total of 19 studies (five RCTs [17, 32,33,34,35] and 14 observational studies [18, 19, 27,28,29, 36,37,38,39,40,41,42,43,44]) were included in the final analysis. All studies were published between 2005 and 2022.
Baseline study characteristics
The 19 included studies (Table 1) comprised a total of 21,793 patients. The RCTs included a total of 397 patients and the observational studies a total of 21,396 patients. Extramedullary fixation was used in 15,910 patients and 5,883 patients were treated using intramedullary fixation. The follow-up ranged from 6 to 60 months. A complete overview of reported variables per study is shown in Table 2.
Quality assessment
The details and distribution of the quality assessment using the RoB 2 for RCTs and MINORS for observational studies are described in Tables 3 and 4. The overall bias assessment in the RoB 2 ranged from high overall risk of bias in Pajarinen et al. [32] to low overall risk of bias in Tao et al. [35] and Ovesen et al. [33]. The mean score for the MINORS was 18 (SD 2.5) and ranged from 15 (moderate quality) to 22 (high quality).
A summary of all study results and meta-analyses is provided in Table 5. The most (clinically) relevant and statistically significant outcome measures are described below. Forrest plots for additional outcome measures can be found in Online Resource 4 (OR4).
Functional outcomes
Harris hip score (HHS)
The mean HHS (six studies, Fig. 2) at a minimum of 1 year after trauma was 82.2 in 261 patients for extramedullary fixation and 82.9 in 249 patients for intramedullary fixation. There was no significant difference between groups, with a considerable level of heterogeneity of effect across studies (MD 1.38, CI − 3.43 to 6.18, I2 = 92%, p = 0.57) [19, 27, 35, 38, 39, 41].
Pain
The mean 1-year post-operative pain score (four studies, Fig. 3) was 2.4 in 2679 patients for extramedullary fixation and 2.2 in 1006 patients for intramedullary fixation, on a 10-point scale. There was no significant difference in standardized 1-year post-operative pain between groups (SMD 0.04, CI − 0.04 to 0.11, I2 = 0%, p = 0.36) [17, 28, 40, 42].
Other functional outcomes
No significant difference between groups was found in Parker mobility score (MD 0.52, CI − 0.11 to 1.14, I2 = 0%, p = 0.11) (Online resource 4, Fig. 1) [18, 41] and 1-year post-operative walking ability (RR 1.11, CI 0.82–1.50, I2 = 0%, p = 0.97) (OR4, Fig. 2) [35, 39].
Complications
Reoperation
Reoperation (11 studies, Fig. 4) was performed in 483 out of 15,389 (3.1%) in extramedullary fixation and 199 out of 5548 (3.6%) patients in intramedullary fixation. No significant difference between groups was found, with a moderate level of heterogeneity of effect across studies (RR 0.94, 0.72–1.23, I2 = 34%, p = 0.85) [17, 19, 28, 33, 34, 38,39,40,41,42, 44].
Nonunion
Nonunion (nine studies, Fig. 5) occurred in 26 cases out of 6933 (0.4%) in extramedullary fixation and seven cases out of 1790 (0.4%) in intramedullary fixation. There was no significant difference in non-union between groups (RR 1.41, CI 0.58–3.42, I2 = 0%, p = 0.45 [17,18,19, 28, 29, 34, 38, 39, 41].
Cut-out
Cut-out (12 studies, Fig. 6) occurred in 36 cases out of 7158 (0.5%) in extramedullary fixation and 20 cases out of 1852 (1.1%) in intramedullary fixation. There was no significant difference in cut-out rate between groups (RR 0.69, CI 0.40–1.20, I2 = 0%, p = 0.19) [17,18,19, 28, 29, 32,33,34, 36,37,38,39].
Peri-implant fracture
Peri-implant fracture (five studies, Fig. 7) occurred in 16 cases out of 6732 (0.2%) in extramedullary fixation and 7 cases out of 1600 (0.4%) in intramedullary fixation. There was no significant difference in peri-implant fracture rate between fixation groups, with a moderate to substantial level of heterogeneity of effect across studies (RR 1.14, CI 0.16–8.18, I2 = 66%, p = 0.89) [17, 19, 28, 34, 38].
Conversion to prosthesis
Conversion to prosthesis (eight studies, Fig. 8) occurred in 269 cases out 15,118 (1.8%) in extramedullary fixation and 105 cases out of 5282 (2.0%) in intramedullary fixation. There was no significant difference between groups (RR 0.87, CI 0.66–1.15, I2 = 15%, p = 0.32) [17, 28, 29, 33, 39, 41, 42, 44].
Implant/fixation failure
Implant or fixation failure (eight studies, Fig. 9) was reported in 70 cases out of 6858 (1.0%) in extramedullary fixation and 15 cases out of 1767 (0.8%) in intramedullary fixation. There was no significant difference between groups (RR 1.78, CI 0.82–3.86, I2 = 20%, p = 0.15) [19, 28, 29, 34, 38,39,40,41].
Other complications
There were no significant differences between groups in deep infection (RR 2.39, CI 0.47–12.25, I2 = 0%, p = 0.30, OR4, Fig. 3) [18, 29, 32,33,34, 38, 39, 41], superficial infection (RR 1.12, CI 0.43–2.90, I2 = 0%, p = 0.81, OR4, Fig. 4) [19, 29, 32, 34, 38, 39, 41, 43], malunion (RR 0.78, CI 0.33–1.84, I2 = 0%, p = 0.58, OR4, Fig. 5) [19, 38, 41], limb-length discrepancy > 25 mm (RR 3.36, CI 0.25–45.01, I2 = 48%, p = 0.36, OR4, Fig. 6) [19, 29, 38], heterotopic ossification (RR 0.76, CI 0.26–2.25, I2 = 23%, p = 0.62, OR4, Fig. 7) [19, 38, 41], osteolysis in well-fixed implants (RR 0.74, CI 0.05–11.03, I2 = 30%, p = 0.83, OR4, Fig. 8) [19, 38], and 1-year mortality (RR 0.98, CI 0.61–1.56, I2 = 0%, p = 0.92, OR4, Fig. 9) [19, 40].
Surgical outcomes
There was a significantly longer operation time (9 studies, Fig. 10) for extramedullary fixation, with a mean of 53.5 min in 6704 patients versus 53.2 min in 1685 patients in the intramedullary group (MD 14.1, CI 6.98–21.29, I2 = 96%, p < 0.001) [18, 19, 28, 29, 35, 39,40,41, 43]. Operative blood loss (7 studies, Fig. 11) in the extramedullary group was significantly higher as well, with a mean of 351 mL in 305 patients versus a mean of 204 mL in 355 patients in the intramedullary group (MD 92.30, CI 13.49–171.12, I2 = 98%, p = 0.02) [18, 19, 29, 35, 39, 40, 43].
No significant differences between the groups were found in the other surgical outcomes or operation characteristics: time to radiological union (MD − 0.04, CI − 1.10 to 1.02, I2 = 84%, p = 0.94, OR4, Fig. 10) [19, 29, 35, 38, 39], good quality of reduction (RR 1.03, CI 0.95–1.11, I2 = 0%, p = 0.46, OR4, Fig. 11) [19, 35, 38, 40, 41], hospital stay (MD 0.50, CI − 0.25 to 1.25, I2 = 48%, p = 0.19, Online Resource 4, Fig. 12) [19, 35, 39, 41, 43], or fluoroscopy time (MD 13.12, CI − 3.28 to 29.52, I2 = 73%, p = 0.12, Online Resource 4, Fig. 13) [19, 35, 41].
Only two studies reported data on hospital or surgery-related costs [41, 43]. Due to differences in included cost variables, no pooled effect could be calculated. None of the included studies reported data on cost-effectiveness.
Discussion
This systematic review and meta-analysis compared extramedullary and intramedullary fixation for stable two-part trochanteric fractures (AO 31-A1). No differences between fixation groups were found in functional outcomes and complications. Duration of surgery and intra-operative blood loss were found to be statically different between fixation groups, in favor of intramedullary fixation, though with a high level of heterogeneity.
This is the first systematic review and meta-analysis that restricted the evaluation of treatment effect, in present-day devices, to patients with only stable two-part trochanteric fractures. It includes a substantially larger number of patients than all previous meta-analyses [9, 14, 21, 22, 45, 46]. The most recent Cochrane review, by Lewis et al. [45], on RCTs and ‘RCT-like’ cohort studies published up to July 2020 compared EM and IM fixation for a combination of AO A1-A3 fractures. In the only stratified analysis on A1 fractures, and in accordance with the current study’s data, it found no differences between fixation groups for reoperation. For all combined fractures, it found no difference in reoperation, mortality, and several functional outcomes. Contrary to this review, it did find an increased risk of many complications including non-union, both superficial and deep infection, cut-out and implant failure for extramedullary devices. Intramedullary devices were associated with an increased intra- and post-operative periprosthetic fracture rate. The differences between this Cochrane review and our meta-analysis can largely be explained by the absence of several recently published large cohort studies, its combination of both stable, and unstable fractures, and inclusion of older studies with a relatively higher rate of complications.
Another review by Wessels et al. [21], comparing SHS vs IMN for AO A1-A3 trochanteric fractures, also found no significant differences between fixation devices in the A1 fracture subgroup. Wessels et al. only described a combination of major complications and, specifically, non-union. Both Lewis et al. and Wessels et al. did not include surgical outcomes or operation characteristics and also included pathological fractures.
Older reviews by Parker et al. [46] and Jones et al. [14] studied fixation of all types of trochanteric fractures by cephalomedullary nail or sliding hip screw. As opposed to the current meta-analysis and review by Wessels et al., they reported a significantly higher number of post- and intra-operative femoral fractures and higher reoperation rate for patients treated with a cephalomedullary nail. Both did not provide a stratified analysis for type of fracture. The difference between Jones et al., our findings and other recent reviews is likely caused by the fact that it included older studies, from the earlier days of intramedullary fixation. Since then, device quality, design and surgical experience with intramedullary devices have greatly improved. Where older research advised against the use of intramedullary fixation, current data on clinical and functional outcomes do not warrant any statement on the preferred type of device from a clinical perspective.
Interpretation of results
This meta-analysis found that only the duration of surgery and intra-operative blood loss to be statistically significantly in favor of intramedullary fixation. These results should be interpreted with care. The level of heterogeneity of effects across the studies was over 90% with large differences in mean operation time or blood loss (e.g. a range of 25.6–136 min for extramedullary fixation [18, 19]). This large variety may partly be explained by differences in surgery protocols, device used, experience of surgeons, the small number of inclusions, and inclusion or exclusion of anesthesia times across the included studies. The largest study by Matre et al. [28], with 7643 patients, and arguably the best sample size for this comparison, found no significant difference in operation time. The only other review reporting duration of surgery, by Parker et al. [46], included studies all conducted before the year 2005 and concluded that no definitive conclusion could be drawn because of limited data.
As current literature shows no differences between intra- and extramedullary fixation in functional outcomes or complications, it is tempting to conclude that surgeons could use either type of device. However, the difference in device costs should also be considered in this decision. Extramedullary fixation or more specifically dynamic/sliding hip screw is most likely the most cost-effective implant [47, 48]. Intramedullary devices can cost well over $1000 more than extramedullary options with, as demonstrated by this review, the same surgical and clinical results for stable fractures. More expensive devices, such as PFNA, should be avoided when enough surgical expertise with extramedullary devices exists. This financial argument is also used in the Dutch Guideline for treatment of proximal femoral fractures and NICE guideline, as an argument for usage of extramedullary devices when clear evidence for superiority is absent [23, 24].
Some limitations should be considered when interpreting the results of this study: First, in every meta-analysis, there is a chance of publication bias, however, the funnel plots show no clear indication for one-sided publication for the included variables. The large majority of patients (> 98%) included in this study came from observational studies resulting in a larger risk of selection bias. Many of the studied variables have a moderate-to-high level of heterogeneity between studies. Part of this could be explained by random chance and can be corrected for by using random effect models. Another part could be explained by the (small) differences in devices used, different moments in time studies were conducted, differences in study populations (e.g. age, fracture type prevalence, and inclusion of patients with concomitant injuries), and international differences between included studies. Most of the included RCTs and to a lesser degree, observational studies appear underpowered or only adequately powered for the total group of combined stable and unstable trochanteric femoral fractures. As many of the studied outcomes and complications are rare, and occur at rates of 1% or lower, studies are often not adequately powered to study these outcomes for a restricted group of stable fractures. A combination of heterogeneity and low power could conceal treatment effects that now seem insignificant. Although the clinical relevance of these effects may be questionable. Larger and adequately powered RCTs or high-quality prospective observational studies comparing extramedullary and intramedullary fixation in, specifically, stable trochanteric femoral fractures are needed to provide a definitive answer to the question of superiority for treatment for stable trochanteric fractures. Considering the low frequency of complications and sparsity of data on functional outcome and patient reported outcomes, future research should focus on both functional and quality of life data, and provide a large scale cost-effectiveness analysis.
Conclusion
There are no meaningful differences in complications, surgical-, or functional outcomes between intramedullary and extramedullary fixation of stable two-part trochanteric femoral (AO type 31-A1) fractures. Both treatment options result in good outcomes and few complications. As outcomes do not differ, costs should be taken into account when considering devices. Therefore, the use of extramedullary devices should be advised when enough surgical expertise with these devices is available. Future research should focus on (functional) outcomes for individual fracture AO type A1–A3 subgroups, and cost-effectivity of treatment and (medical) decision making for both techniques.
Data availability
All data used in this meta-analysis were published in previous literature. Specific information, on the data used or the analysis performed, is available upon request from the corresponding author.
References
Amin S, Achenbach SJ, Atkinson EJ, Khosla S, Melton LJ 3rd (2014) Trends in fracture incidence: a population-based study over 20 years. J Bone Miner Res 29(3):581–589. https://doi.org/10.1002/jbmr.2072
Collaborators GBDF (2021) Global, regional, and national burden of bone fractures in 204 countries and territories, 1990–2019: a systematic analysis from the Global Burden of Disease Study 2019. Lancet Healthy Longev 2(9):e580–e592. https://doi.org/10.1016/S2666-7568(21)00172-0
Tsuda T (2017) Epidemiology of fragility fractures and fall prevention in the elderly: a systematic review of the literature. Curr Orthop Pract 28(6):580–585. https://doi.org/10.1097/BCO.0000000000000563
Adeyemi A, Delhougne G (2019) Incidence and economic burden of intertrochanteric fracture: a medicare claims database analysis. JB JS Open Access 4(1):e0045. https://doi.org/10.2106/JBJS.OA.18.00045
Kanters TA, van de Ree CLP, de Jongh MAC, Gosens T, Hakkaart-van RL (2020) Burden of illness of hip fractures in elderly Dutch patients. Arch Osteoporos 15(1):11. https://doi.org/10.1007/s11657-019-0678-y
Meinberg EG, Agel J, Roberts CS, Karam MD, Kellam JF (2018) Fracture and dislocation classification compendium-2018. J Orthop Trauma 32(Suppl 1):S1–S170. https://doi.org/10.1097/BOT.0000000000001063
(DHFA) DHfA (2019) DHFA report 2019: Dutch Instute for Clinical Auditing (DICA). https://dica.nl/jaarrapportage-2019/dhfa
Kaplan K, Miyamoto R, Levine BR, Egol KA, Zuckerman JD (2008) Surgical management of hip fractures: an evidence-based review of the literature. II: intertrochanteric fractures. J Am Acad Orthop Surg 16(11):665–673. https://doi.org/10.5435/00124635-200811000-00007
Zhang WQ, Sun J, Liu CY, Zhao HY, Sun YF (2018) Comparing the intramedullary nail and extramedullary fixation in treatment of unstable intertrochanteric fractures. Sci Rep 8(1):2321. https://doi.org/10.1038/s41598-018-20717-2
Schipper IB, Marti RK, van der Werken C (2004) Unstable trochanteric femoral fractures: extramedullary or intramedullary fixation. Review of literature. Injury 35(2):142–151. https://doi.org/10.1016/s0020-1383(03)00287-0
Forte ML, Virnig BA, Eberly LE, Swiontkowski MF, Feldman R, Bhandari M et al (2010) Provider factors associated with intramedullary nail use for intertrochanteric hip fractures. J Bone Jt Surg Am 92(5):1105–1114. https://doi.org/10.2106/JBJS.I.00295
Anglen JO, Weinstein JN, American Board of Orthopaedic Surgery Research C (2008) Nail or plate fixation of intertrochanteric hip fractures: changing pattern of practice. A review of the American Board of Orthopaedic Surgery Database. J Bone Jt Surg Am. 90(4):700–707. https://doi.org/10.2106/JBJS.G.00517
Rogmark C, Spetz CL, Garellick G (2010) More intramedullary nails and arthroplasties for treatment of hip fractures in Sweden. Acta Orthop 81(5):588–592. https://doi.org/10.3109/17453674.2010.506631
Jones HW, Johnston P, Parker M (2006) Are short femoral nails superior to the sliding hip screw? A meta-analysis of 24 studies involving 3,279 fractures. Int Orthop 30(2):69–78. https://doi.org/10.1007/s00264-005-0028-0
Parker MJ, Handoll HH, Bhonsle S, Gillespie WJ (2000) Condylocephalic nails versus extramedullary implants for extracapsular hip fractures. Cochrane Database Syst Rev (2):CD000338. https://doi.org/10.1002/14651858.CD000338
Parker MJ, Handoll HH, Chinoy MA (2001) Extramedullary fixation implants for extracapsular hip fractures. Cochrane Database Syst Rev (2):CD000339. https://doi.org/10.1002/14651858.CD000339
Parker MJ (2017) Sliding hip screw versus intramedullary nail for trochanteric hip fractures; a randomised trial of 1000 patients with presentation of results related to fracture stability. Injury 48(12):2762–2767. https://doi.org/10.1016/j.injury.2017.10.029
Mohan H, Kumar P (2019) Surgical treatment of type 31–A1 two-part intertrochanteric femur fractures: is proximal femoral nail superior to dynamic hip screw fixation? Cureus 11(2):e4110. https://doi.org/10.7759/cureus.4110
Talmac MA, Gorgel MA, Armagan R, Sonmez MM, Ozdemir HM (2019) Examining implant superiority in the treatment of simple pertrochanteric fractures of the proximal femur in elderly patients. Yasli hastalarda proksimal femur basit pertrokanterik kiriklarin tedavisinde hangi implant ustundur? Ulus Travma Acil Cerrahi Derg 25(4):410–6. https://doi.org/10.14744/tjtes.2019.21270
Singh NK, Sharma V, Trikha V, Gamanagatti S, Roy A, Balawat AS et al (2019) Is PFNA-II a better implant for stable intertrochanteric fractures in elderly population? A prospective randomized study. J Clin Orthop Trauma 10(Suppl 1):S71–S76. https://doi.org/10.1016/j.jcot.2019.02.004
Wessels JO, Bjarnesen MP, Erichsen JL, Palm H, Gundtoft PH, Viberg B (2022) Sliding hip screw vs intramedullary nail for AO/OTA31A1-A3: a systematic review and meta-analysis. Injury 53(3):1149–1159. https://doi.org/10.1016/j.injury.2021.12.034
Bhandari M, Schemitsch E, Jonsson A, Zlowodzki M, Haidukewych GJ (2009) Gamma nails revisited: gamma nails versus compression hip screws in the management of intertrochanteric fractures of the hip: a meta-analysis. J Orthop Trauma 23(6):460–464. https://doi.org/10.1097/BOT.0b013e318162f67f
Heelkunde MwNOVNVv (2016) Behandeling pertrochantere fracturen: Federatie Medisch Specialisten; [updated 1 september 2016]. https://richtlijnendatabase.nl/richtlijn/proximale_femurfracturen/pertrochantere_femurfractuur/behandeling_pertrochantere_fracturen.html
(NICE) NIfHaCE (2020) National Institute for Health and Care Excellence: Guidelines, Hip fracture management. ed2017. NBK553768 [bookaccession]
Mellema JJ, Janssen S, Schouten T, Haverkamp D, van den Bekerom MPJ, Ring D et al (2021) Intramedullary nailing versus sliding hip screw for A1 and A2 trochanteric hip fractures. Bone Jt J 103-B(4):775–781. https://doi.org/10.1302/0301-620X.103B.BJJ-2020-1490.R1
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Sevinc HF, Cirpar M, Canbeyli ID, Daglar B, Oktas B, Durusoy S (2020) Comparison of functional outcomes in patients fixed with dynamic hip screw and proximal femur nail-anti-rotation in A1 and A2 type intertrochanteric femur fractures A1 ve A2 tipi femur intertrokanterik kiriklarinda kayan kalca vidasi ve proksimal femur civisi-antirotasyon ile tespit sonrasi hastalarin fonksiyonel sonuclarinin karsilastirilmasi. Ulus Travma Acil Cerrahi Derg 26(5):811–7. https://doi.org/10.14744/tjtes.2020.39888.
Matre K, Havelin LI, Gjertsen JE, Espehaug B, Fevang JM (2013) Intramedullary nails result in more reoperations than sliding hip screws in two-part intertrochanteric fractures. Clin Orthop Relat Res 471(4):1379–1386. https://doi.org/10.1007/s11999-012-2728-2
Cho HM, Lee K (2016) Clinical and functional outcomes of treatment for type A1 intertrochanteric femoral fracture in elderly patients: comparison of dynamic hip screw and proximal femoral nail antirotation. Hip Pelvis 28(4):232–242. https://doi.org/10.5371/hp.2016.28.4.232
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I et al (2019) RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 366:l4898. https://doi.org/10.1136/bmj.l4898
Pajarinen J, Lindahl J, Michelsson O, Savolainen V, Hirvensalo E (2005) Pertrochanteric femoral fractures treated with a dynamic hip screw or a proximal femoral nail. A randomised study comparing post-operative rehabilitation. J Bone Jt Surg Br 87(1):76–81
Ovesen O, Andersen M, Poulsen T, Nymark T, Overgaard S, Rock ND (2006) The trochanteric gamma nail versus the dynamic hip screw: a prospective randomised study. One-year follow-up of 146 intertrochanteric fractures. Hip Int 16(4):293–298. https://doi.org/10.5301/hip.2008.2820
Zou J, Xu Y, Yang H (2009) A comparison of proximal femoral nail antirotation and dynamic hip screw devices in trochanteric fractures. J Int Med Res 37(4):1057–1064. https://doi.org/10.1177/147323000903700410
Tao R, Lu Y, Xu H, Zhou ZY, Wang YH, Liu F (2013) Internal fixation of intertrochanteric hip fractures: a clinical comparison of two implant designs. ScientificWorldJournal. 2013:834825. https://doi.org/10.1155/2013/834825
Andruszkow H, Frink M, Fromke C, Matityahu A, Zeckey C, Mommsen P et al (2012) Tip apex distance, hip screw placement, and neck shaft angle as potential risk factors for cut-out failure of hip screws after surgical treatment of intertrochanteric fractures. Int Orthop 36(11):2347–2354. https://doi.org/10.1007/s00264-012-1636-0
Crespo E, Galvez J, Tenias JM, Cano I, Crespo R, Palacios V (2012) A comparative study between gamma nail and percutaneous compression plating for the treatment of intertrochanteric hip fractures. Eur J Trauma Emerg Surg 38(4):443–449. https://doi.org/10.1007/s00068-012-0181-2
Yu W, Zhang X, Zhu X, Yu Z, Xu Y, Zha G et al (2016) Proximal femoral nails anti-rotation versus dynamic hip screws for treatment of stable intertrochanteric femur fractures: an outcome analyses with a minimum 4 years of follow-up. BMC Musculoskelet Disord 17:222. https://doi.org/10.1186/s12891-016-1079-7
Tian YYWZ (2018) Short-term follow-up of dynamic hip screw versus proximal femoral nail anti-rotation for type AO/OTA A1 intertrochanteric femoral fracture in older adults. Chin J Tissue Eng Res 23(12):1834–1839
van der Sijp MPL, de Groot M, Meylaerts SA, du Pre KJ, Verhage SM, Schipper IB et al (2021) High risks of failure observed for A1 trochanteric femoral fractures treated with a DHS compared to the PFNA in a prospective observational cohort study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03824-0
Alessio-Mazzola M, Traverso G, Coccarello F, Sanguineti F, Formica M (2022) Dynamic hip screw versus intramedullary nailing for the treatment of A1 intertrochanteric fractures: a retrospective, comparative study and cost analysis. Jt Dis Relat Surg 33(2):314–322. https://doi.org/10.52312/jdrs.2022.646
Gronhaug KML, Dybvik E, Matre K, Ostman B, Gjertsen JE (2022) Intramedullary nail versus sliding hip screw for stable and unstable trochanteric and subtrochanteric fractures : 17,341 patients from the Norwegian Hip Fracture Register. Bone Jt J 104-B(2):274–282. https://doi.org/10.1302/0301-620x.104b2.Bjj-2021-1078.R1
Pehlivanoglu T, Bayram S, Demirel M, Chodza M, Kocazeybek E, Salduz A et al (2021) Proximal femoral nailing versus dynamic hip screw in management of stable intertrochanteric femur fractures: a comparison of clinical and radiological outcomes. J Istanb Fac Med 84(4):514–520
Pyrhonen HS, Lagergren J, Wolf O, Bojan A, Mukka S, Moller M et al (2022) No difference in conversion rate to hip arthroplasty after intramedullary nail or sliding hip screw for extracapsular hip fractures: an observational cohort study of 19,604 individuals. J Bone Jt Surg Am. https://doi.org/10.2106/jbjs.22.00316
Lewis SR, Macey R, Gill JR, Parker MJ, Griffin XL (2022) Cephalomedullary nails versus extramedullary implants for extracapsular hip fractures in older adults. Cochrane Database Syst Rev 1:CD000093. https://doi.org/10.1002/14651858.CD000093.pub6
Parker MJ, Handoll HH (2010) Gamma and other cephalocondylic intramedullary nails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev (9):CD000093. https://doi.org/10.1002/14651858.CD000093.pub5
Swart E, Makhni EC, Macaulay W, Rosenwasser MP, Bozic KJ (2014) Cost-effectiveness analysis of fixation options for intertrochanteric hip fractures. J Bone Jt Surg Am 96(19):1612–1620. https://doi.org/10.2106/JBJS.M.00603
Bohl DD, Basques BA, Golinvaux NS, Miller CP, Baumgaertner MR, Grauer JN (2014) Extramedullary compared with intramedullary implants for intertrochanteric hip fractures: thirty-day outcomes of 4432 procedures from the ACS NSQIP database. J Bone Jt Surg Am 96(22):1871–1877. https://doi.org/10.2106/JBJS.N.00041
Acknowledgements
STABLE-HIP Study Group: Taco Gosens, MD PhD, Department of Orthopedics, Elisabeth-TweeSteden Hospital (ETZ), Tilburg, The Netherlands; Johannes H. Hegeman, MD PhD, Department of Surgery, Zorg Groep Twente (ZGT), Almelo, The Netherlands; Suzanne Polinder, PhD, Department of Public Health, Erasmuc MC, Rotterdam, The Netherlands; Rudolf W. Poolman, MD PhD, Department of Orthopedics, OLVG Hospital, Amsterdam, The Netherlands; Hanna C. Willems, MD PhD, Department of Geriatrics, Amsterdam University Medical Center, Amsterdam, The Netherlands; Rutger G. Zuurmond, MD PhD, Department of Orthopedics, Isala Hospital, Zwolle, The Netherlands
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Consortia
Contributions
The idea for this review and meta-analysis was conceived by PJ, MHJV, and EMML. Literature search and data collection was performed by LHTN and ACP, under supervision of MLZ, SAIL, and EMML. Statistical analysis was performed by MLZ, LHTN, and ACP, under supervision of EMML. The manuscript was drafted by MLZ, LHTN, and ACP. All authors critically revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
This systematic review and meta-analysis did not require approval from the local medical research ethics committee.
Informed consent
This systematic review and meta-analysis did not require informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
STABLE-HIP Study Group members are listed in the Acknowledgements section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zeelenberg, M.L., Nugteren, L.H.T., Plaisier, A.C. et al. Extramedullary versus intramedullary fixation of stable trochanteric femoral fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg 143, 5065–5083 (2023). https://doi.org/10.1007/s00402-023-04902-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04902-1