Abstract
Aim
Aim of the study was to assess whether early surgery and other clinical and orthogeriatric parameters could affect mortality rate in hip fracture patients aged > 85.
Materials and methods
Data regarding a 42-month period were retrospectively obtained from the institutional medical records and registry data. Gender, age, fracture pattern, surgical technique, type of anesthesia, timing of surgical intervention (within 24, 48 or 72 h from admission), days of hospitalization, mortality rate divided in intra-hospital, at 30 days and at 1 year were collected for the whole population. Some additional data were collected for an orthogeriatric subgroup.
Results
941 patients were considered, with a mean age of 89 years. Surgery was performed within 24, 48 and 72 h in 24.4%, 54.5% and 66.1% of cases, respectively. Intra-hospital mortality rate resulted to be 3.4%, while mortality at 30 days and 1 year resulted to be 4.5% and 31%, respectively. Early surgery within 48 and 72 h were significantly associated with a lower intra-hospital and 30-day mortality rate. In the orthogeriatric subgroup (394 patients), a significant association with a higher mortality rate was found for general anesthesia, number of comorbidities, ADL (Activities of Daily Living) < 3, transfer to other departments.
Conclusions
In over-85 hip fracture patients, the threshold for early surgery might be moved to 72 h to allow patients pre-operative stabilization and medical optimization as intra-hospital and 30-day mortality rates remain significantly lower. Advanced age, male sex, number of comorbidities, pre-operative dependency in ADL, general anesthesia, length of hospitalization and transfer to other departments were significantly related to mortality rate.
Similar content being viewed by others
Introduction
Proximal femur fracture (PFF) is one of the most frequent fractures in the elderly population, with severe clinical and socio-economic implications.
Due to the localization of the fracture, and in order to prevent complications related to prolonged immobilization, surgery is performed in more than 90% of cases [1, 2].
Although only 2.5% of the Italian population exceeds the age of 85 years, over 40–50% of patients hospitalized for proximal femur fractures are included in this age group, defined as “oldest old,” according to the higher prevalence of osteoporosis [3,4,5]. Nevertheless, there are few studies that deal purely with the geriatric population, as most papers about PFF treatment consider patients aged over 65 years. Intra-hospital mortality appears to be around 5% [1, 6], while mortality at 30 days is reported to be between 5 and 10% [4, 5, 7, 8], with peaks up to 15% in the over 80-years old [9, 10]. Mortality 1 year after surgery stands around 20 to 30% in most studies [1, 11,12,13,14,15,16,17,18].
The timing of surgery still remains a high debated issue. Some literature reports state that surgical intervention must be carried out within 24 h of admission [19,20,21,22,23,24,25,26,27,28,29,30]. Many other authors report a reduced mortality in case of early intervention within 48 h, both in the short and in the long term [4, 19, 24, 25, 31,32,33,34]. The advantages of early surgery would reside in a better functional outcome, a reduced hospitalization, fewer complications, reduced pain and a reduced risk of death [28, 31, 33]. However, there is a part of the literature that does not find benefits in terms of mortality from early intervention [7, 34,35,36,37] These authors claim that unstable patients must be stabilized first, even at the expense of operative timing [6, 7].
Beside literature conflicting results, the value of early surgery is generally accepted. Thus, surgery realized within 48 h after PFF is one of the mostly used indicators of healthcare quality [2].
Aim of the study was to assess whether early surgery (within 24, 48 or 72 h) for PFF in patients aged > 85 affects intra-hospital, 30-days and 1-year mortality rate, in order to define the more accurate early surgery time threshold for these patients. Secondary aim was to assess which other variables, including clinical and orthogeriatric parameters, could influence the mortality rate in this age group.
Materials and methods
All patients surgically treated at a single trauma center for PFF between January 1, 2014, and June 30, 2017, were initially considered.
Exclusion criteria were: patients aged under 85, PFF in the antecedent 2 years, patients in critical conditions who were treated in intensive or semi-intensive care unit before surgery, polytrauma, patients deceased within 48 h from admission without undergoing surgery, oncologic patients with metastatic disease, pathologic fractures, patients treated conservatively, simultaneous bilateral fracture, patients with incomplete/lacking documentation.
Data were retrospectively obtained from the institutional medical records and registry data, and any death was taken from nationwide database until June 30, 2018.
The records collected for the whole population were: gender, age, fracture pattern (medial/intracapsular vs lateral/extracapsular), surgical technique (partial hip replacement vs osteosynthesis), type of anesthesia, timing of surgical intervention (within 24, 48 or 72 h from admission), days of hospitalization (from surgery to discharge and total), mortality rate divided in intra-hospital, at 30 days and at 1 year.
Since a PFF registry was introduced from January 2016 through the collaboration with the orthogeriatric service, some addictive data could be collected for patients admitted form January 2016 to June 2017 (orthogeriatric subgroup). These data included: number of drugs per day; type of drugs, divided in six subcategories (anticoagulant, antiaggregant, antidiabetics, drugs acting on the CNS, corticosteroids/immune-suppressive drugs and antiresorptive drugs); comorbidities, divided in six subcategories (non-complicated hypertension, cardiovascular diseases excluding non-complicated hypertension, respiratory and neurologic diseases excluding dementia, metabolic diseases including diabetes and renal failure); ADL (Activities of Daily Living) score pre-admission, dividing patients into dependent for ADL (score 0–3) and independent for ADL (score 4–6); post-operative delirium; discharge destination (home, retirement home, healthcare residences, rehabilitation facilities and other intra-hospital departments).
The statistical analysis was performed using the SPSS Statistics software. Mean and standard deviation were calculated for quantitative variables.
Correlation between timing of surgery and mortality at the three set end-points was calculated with the chi-square test on the whole population. A univariate binary logistic regression model was used to identify the correlation between the collected parameters and mortality at the three set end-points, setting mortality as dependent variable. Statistical significance was set for a p value < 0.05. The odds ratio was calculated in order to define the relative risk of mortality for each significant independent covariate.
Samples too small for meaningful statistical analysis were discarded.
Results
The population considered for the study counted 2342 patients admitted with a diagnosis of PFF.
The characteristics of our sample are summarized in Table 1.
Intra-hospital mortality rate of the whole population resulted to be 3.4%, while mortality at 30 days and 1 year resulted to be 4.5% and 31%, respectively.
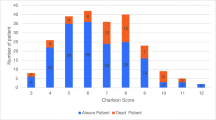
The orthogeriatric subgroup counted 394 patients. Demographic data and additional information as type and number of drugs, comorbidities and discharge destination are resumed in Table 2.
Statistical analysis of retrieved data for the whole population is reported in Tables 3 and 4.
Early surgery within 48 and 72 h was significantly associated with a lower intra-hospital (p 0.001; OR 0.223; CI 0.095–0.521 and p 0.012 OR 0.294; CI 0.142–0.610, respectively) and 30-day mortality rate (p 0.014 OR 0.447; CI 0.235–0.852 and p 0.011 OR 0.449; CI 0.241–0.835, respectively). The possible correlation between surgery within 24 h and intra-hospital mortality (p 0.044) was not confirmed at the univariate analysis (p 0.056). No significant association was found for surgery within 24 h and 30-day mortality, as well as for early surgery (within 24, 48 or 72 h) and 1-year mortality rate (Table 3).
At univariate analysis, a significant association with a lower intra-hospital mortality rate was found for female sex (p 0.001; OR 0.303; CI 0.146–0.626). Conversely, length of hospital stay was associated with a significantly higher intra-hospital mortality rate (p 0.001; OR 1.034; CI 1.013–1.055). Regarding mortality at 30 days, a significant association with a lower mortality rate was found for female sex (p < 0.001; OR 0.299; CI 0.158–0.565), instead an association with higher mortality rate was found for general anesthesia (p 0.006; OR 3.144; CI 1.393–7.094) and intracapsular fracture pattern (p 0.023; OR 2.443; CI 1.134–5.266). Finally, a significant association with a lower 1-year mortality rate was found for female sex (p < 0.001; OR 0.351; CI 0.250–0.494), while age (p < 0.001; OR 1.091; CI 1.049–1.135) and length of hospital stay (p 0.021 OR 1.016; CI 1.002–1.030) resulted to be associated with a significantly higher 1-year mortality rate (Table 4).
Statistical analysis of retrieved data for the orthogeriatric subgroup is reported in Table 5.
At univariate analysis, no parameter has proved to have a significant association with intra-hospital mortality. Conversely, a significant association with a higher 30-day mortality rate was found for transfer to other departments (p 0.009; OR11.050; CI 1.805–67.642), number of comorbidities (p 0.024; OR 1.603; CI 1.065–2.414) and renal failure (p 0.021; OR 3.432; CI 1.207–9.756).
Finally, a significantly lower 1-year mortality rate was found for antiresorptive drugs (p < 0.001; OR 0.223; 0.107–0.464), while a significantly higher 1-year mortality rate was found for transfer to other departments (p 0.015; OR 4.618; CI 1.345–15.853), number of comorbidities (p 0.001; OR 1.361; CI 1.143–1.620), cardiovascular diseases (p 0.001; OR 2.051; CI 1.336–3.148), renal failure (p < 0.001; OR 2.822; CI 1,719–4,632) and dependency in ADL (p 0.010; OR 1.774; CI 1.149–2.740).
A significant correlation between early surgery (48/72 h) and lower number of comorbidities (2 or less) was also found (p 0.002; OR 0.425; CI 0.250–0.723 and p 0.008 OR 0.431; CI 0.231–0.803, respectively). At multivariate analysis, no parameters were found to be statistically significant.
Discussion
Early surgery for PFF is a highly debated topic. The rationale of early surgery for PFF resides in expected lower complications rate, reduced pain, faster rehabilitation and shorter hospitalization. The main goal however is recognized to be the reduction of mortality rate. Most studies set the goal of early surgery within 48 h from admission, supported by highly significant associations with lower mortality rate at different end-points [2, 4, 8, 19, 23, 24, 31,32,33,34, 38, 39]. However, some studies identify the threshold at 24 h to be significantly related to better outcome, both at short and mid-term [4, 19,20,21,22,23,24,25,26,27,28,29,30, 40]. Conversely, some studies set 72 h as the limit for early surgery, with more conflicting results [8, 24, 33]. Nonetheless, the goal of early surgery might be particularly difficult to reach in elderly patients, especially aged over 85 years, who are often frail and affected by several comorbidities. Indeed, some literature studies were not able to find benefits in terms of mortality rate in early surgical intervention [7, 34,35,36,37]. These authors underline that unstable and frail patients must be stabilized and properly prepared before intervention, even at the expense of operative timing [6, 7, 41]. Therefore, whether every patient beyond age, comorbidities and clinical conditions at admittance may benefit from this approach, is especially controversial.
Most studies that relate early surgery to mortality rate in PFF include patients aged over-65 [1, 2, 24], or in some cases over-70/75 [8, 19, 39]. However, the percentage of geriatric patients over-85 in PFF populations is generally growing. This group of patients, despite being representative of a small percentage of the whole population, accounts for nearly half PFF in many studies. In the present study, over-85 patients represented 46.5% of the whole PFF population, which is consistent with other literature studies reporting 42–50% of cases being over-85 [3, 4].
Including younger patients might lower the percentage of complex cases, making the goal of early surgery easier to reach. Moreover, these studies might include more active patients, compliant to rehabilitation and willing to return to pre-trauma level of activity. In the present paper focusing on over-85 patients, surgery was carried out within 48 h in 54.5% of patients, raising to 66.1% when considering the 72 h threshold. Conversely, only 24.4% of interventions was performed within 24 h. These data are consistent with other literature studies reporting 50–67% of interventions performed within 48 h [6, 7]. However, the percentage of early surgeries raised dramatically in the last years, as demonstrated in the more recent orthogeriatric subgroup data, where surgery was performed within 24, 48 and 72 h in 42.6%, 80.7% and 87.5% of cases, respectively. In the authors experience, the creation of an orthogeriatric service was determinant to reach this goal. This is also consistent with other more recent studies [7, 42,43,44,45,46].
Despite the efforts to optimize patients medical and surgical assistance, mortality rate remained high in this age group throughout the study period. In particular, 1-year mortality for the whole population was 31%, which is in line with the literature [1, 11,12,13,14,15,16,17,18]. Nonetheless, advanced age is clearly recognized as a risk factor for mortality in most studies [2, 7, 17, 19, 34, 47,48,49]. In the present study, even if focusing on an already advanced age group, overaged patients demonstrated a significantly higher mortality rate at 1 year. Moreover, 1-year mortality was not affected by early surgery in the present study, whatever the threshold considered.
Conversely, surgery within 48 and also 72 h was significantly related to lower intra-hospital and 30-day mortality rate in the present study. Correlation between surgery within 24 h and lower intra-hospital and 30-day mortality rate, although close to significance (p 0.056), was not confirmed at univariate analysis. This might be due to sample dimensions and deserves further investigations. Nonetheless, some recent literature reports question the value of the 24-h threshold for early surgery in geriatric patients [55,56,57]. First of all, as already suggested by some authors, benefits of early surgery in advanced age might not be as relevant as in younger patients [7, 23, 28, 34, 50]. Beside the already stated characteristics of elderly patients, the number of comorbidities might be a relevant issue to explain these findings. Complex patients with many comorbidities might develop post-operative complications despite early surgery [19, 47, 48, 51]. Likely, these patients might need time and clinical effort to reach acceptable pre-operative conditions [6, 7, 48, 52, 53]. One study in particular suggests that waiting more than two days for hip fracture surgery was not associated with higher complications or mortality rate if delay was due to stabilize patients with active comorbidities at admission [41]. In the present study, most patients had a relevant number of comorbidities, with very few having one or none. Despite studies are difficult to compare because of heterogeneous methods to categorize comorbidities and age cut-offs, these data compare negatively with other literature reports [1, 6, 8, 9, 17]. Moreover, the number of comorbidities in the present study were significantly associated to a higher mortality rate at 1 year. Likely, cardiovascular diseases and renal failure, which constitute the more common comorbidities in the study population, were both significantly associated with 1-year mortality. Some literature studies already recognized these associations [6, 46, 49, 54]. However, the reduced intra-hospital and 30-day mortality might be relevant enough to maintain the effort to perform surgery for PFF within 48 h also for advanced age patients. Moreover, differently from other studies [8], intra-hospital and 30-day mortality rates were significantly reduced also for surgery within 72 h. Despite there is general evidence against this delay in general PFF populations [22, 48, 53], it might be considered an acceptable goal in elderly patients with severe comorbidities that require some more corrective medical interventions to safely face the surgical procedure [23, 28]. Moreover, timing in the present study was significantly affected by number of comorbidities. Compromised patients (3 or more comorbidities) had surgery after 48 and 72 h in a significantly higher percentage of cases. Despite multivariate analysis could not identify the independent role of timing and comorbidities in influencing mortality, the present study results question timing to be the main variable in influencing mortality.
Nonetheless, when analyzing risk factors for mortality after PFF in this overaged population, number and type of comorbidities resulted to have a significant correlation with mortality, together with other parameters clearly recognized by the literature as risk factors as age and male sex [7, 17, 19, 34, 47, 48, 58]. Longer hospitalization, as well as transfer to other departments, showed a significant association with mortality at different end-points. These findings are not always recognized in the literature and may reflect the higher complexity of overaged patients. Surprisingly, a recent study by Nordström et al. reported that longer hospitalization seems to reduce early mortality rate [59]. Likely, being dependent in ADL at admission was associated to a higher 1-year mortality rate, which is consistent to some other recent studies [38, 39, 54, 60,61,62,63,64]. General anesthesia was associated to a higher 30-day mortality rate. This finding is not new, as many previous studies showed this association [65,66,67], while two recent meta-analysis reported contrasting results. Guay et al. did not show any difference between the two techniques, while Van Waesberghe et al. found a reduced intra-hospital mortality with spinal anesthesia but no difference at 30 days [68, 69]. However, whether type of anesthesia directly or indirectly affects mortality is still matter of debate [34], although its usefulness in controlling perioperative pain is well known [67]. In the literature, there are conflicting results about mortality according to fracture patterns. Gundel et al. and Holt et al. reported a higher mortality for extracapsular fractures, but they included in the study patients older than 18 and 50 years, respectively [34, 70]. Cornwall et al. also considered patients older than 50 years, but they divided hip fractures in four subgroups (nondisplaced femoral neck fractures, displaced femoral neck fractures, stable intertrochanteric fractures and unstable intertrochanteric fractures) and showed that displaced femoral neck fractures have the highest mortality rate [71]. We found a similar result, reporting that intracapsular fractures have globally higher mortality than extracapsular fractures, especially at 30 days.
Number and type of pharmacotherapies were not recognized as risk factors, except for antiresorptive drugs that showed a significant association with a lower 1-year mortality rate. This finding is consistent with some recent literature studies [58, 72, 73]. Nonetheless, it is not clear whether this result should be considered as a confounder, as stated by some authors, or if vitamin D and antiresorptive drugs may be directly related to lower mortality. Data of the present study do not allow to answer this statement.
Limits of the present study are: the retrospective design, the presence of detailed data for a limited part of the population, the single-center data collection, and the lack of a multivariate analysis because of the small amount of events (intra-hospital and 30-day death). Strengths of the study are the large sample and the thorough statistical analysis.
Conclusions
In over-85 hip fracture patients, pre-operative stabilization and optimization of general conditions is mandatory together with surgery timing. In this age group, the threshold for early surgery might be moved to 72 h to allow medical optimization as intra-hospital and 30-day mortality rates remain significantly lower. Advanced age, male sex, number of comorbidities, pre-operative dependency in ADL, general anesthesia, length of hospitalization and transfer to other departments for medical conditions were all significantly related to mortality in over-85 patients. Number of comorbidities also significantly affected the timing of surgery. The possible protective role of antiresorptive drugs on mortality after PFF deserves more research and might be considered as confounding until different evidence.
References
Dettoni F, Peveraro A, Dettoni A, Rossi R, Castoldi F, Zareh A et al (2012) Epidemiology of hip fractures in northwestern Italy: a multicentric regional study on incidence of hip fractures and their outcome at 3-year follow-up. Musculoskelet Surg 96(1):41–46
Colais P, Di Martino M, Fusco D, Perucci CA, Davoli M (2015) The effect of early surgery after hip fracture on 1-year mortality. BMC Geriatr 15(1):141
Piscitelli P, Feola M, Rao C, Celi M, Gasbarra E, Neglia C et al (2014) Ten years of hip fractures in Italy: for the first time a decreasing trend in elderly women. World J Orthop 5(3):386–391
Casaletto JA, Gatt R (2004) Post-operative mortality related to waiting time for hip fracture surgery. Injury 35(2):114–120
Cooper C (1997) The crippling consequences of fractures and their impact on quality of life. Am J Med 103(2A):12S–7S (discussion 17S–9S)
Belmont PJ Jr, Garcia EJ, Romano D, Bader JO, Nelson KJ, Schoenfeld AJ (2014) Risk factors for complications and in-hospital mortality following hip fractures: a study using the National Trauma Data Bank. Arch Orthop Trauma Surg 134(5):597–604
Forni S, Pieralli F, Sergi A, Lorini C, Bonaccorsi G, Vannucci A (2016) Mortality after hip fracture in the elderly: the role of a multidisciplinary approach and time to surgery in a retrospective observational study on 23,973 patients. Arch Gerontol Geriatr 66(124):13–17
Rosso F, Dettoni F, Bonasia DE, Olivero F, Mattei L, Bruzzone M et al (2016) Prognostic factors for mortality after hip fracture: operation within 48 hours is mandatory. Injury 47:S91–S97
Clement ND, Aitken SA, Duckworth AD, McQueen MM, Court-Brown CM (2011) The outcome of fractures in very elderly patients. J Bone Joint Surg Br 93(6):806–810
Hu F, Jiang C, Shen J, Tang P, Wang Y (2012) Preoperative predictors for mortality following hip fracture surgery: a systematic review and meta-analysis. Injury 43(6):676–685
Lin C, Ou Y, Chen S, Liu Y, Lin J (2010) Comparison of artificial neural network and logistic regression models for predicting mortality in elderly patients with hip fracture. Injury 41(8):869–873
Cenzer IS, Tang V, Boscardin WJ, Smith AK, Ritchie C, Wallhagen MI et al (2016) One-year mortality after hip fracture: development and validation of a prognostic index. J Am Geriatr Soc 64(9):1863–1868
Haleem S, Lutchman L, Mayahi R, Grice JE, Parker MJ (2008) Mortality following hip fracture: trends and geographical variations over the last 40 years. Injury 39(10):1157–1163
Haentjens P, Magaziner J, Colón-Emeric CS, Vanderschueren D, Milisen K, Velkeniers B et al (2010) Meta-analysis: excess mortality after hip fracture among older women and men. Ann Intern Med 152(6):380
Moran CG, Wenn RT, Sikand M, Taylor AM (2005) Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am 87(3):483–489
Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ (2003) Mortality risk after hip fracture. J Orthop Trauma 17(8 Suppl):S2–S5
Roche JJW, Wenn RT, Sahota O, Moran CG (2005) Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ 331(7529):1374
Rosell PAE, Parker MJ (2003) Functional outcome after hip fracture. A 1-year prospective outcome study of 275 patients. Injury 34(7):529–532
Meessen JMTA, Pisani S, Gambino ML, Bonarrigo D, van Schoor NM, Fozzato S et al (2014) Assessment of mortality risk in elderly patients after proximal femoral fracture. Orthopedics 37(2):e194–e200
Ribeiro TA, Premaor MO, Larangeira JA, Brito LG, Luft M, Guterres LW et al (2014) Predictors of hip fracture mortality at a general hospital in South Brazil: an unacceptable surgical delay. Clinics (Sao Paulo) 69(4):253–258
Shiga T, Wajima Z, Ohe Y (2008) Is operative delay associated with increased mortality of hip fracture patients? Systematic review, meta-analysis, and meta-regression. Can J Anaesth 55(3):146–154
Villar RN, Allen SM, Barnes SJ (1986) Hip fractures in healthy patients: operative delay versus prognosis. Br Med J (Clin Res Ed) 293(6556):1203–1204
Yonezawa T, Yamazaki K, Atsumi T, Obara S (2009) Influence of the timing of surgery on mortality and activity of hip fracture in elderly patients. J Orthop Sci 14(5):566–573
Simunovic N, Devereaux PJ, Sprague S, Guyatt GH, Schemitsch E, Debeer J et al (2010) Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ 182(15):1609–1616
Bottle A, Aylin P (2006) Mortality associated with delay in operation after hip fracture: observational study. BMJ 332(7547):947–951
Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL (2002) The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med 112(9):702–709
Manninger J, Kazar G, Fekete G, Fekete K, Frenyo S, Gyarfas F et al (1989) Significance of urgent (within 6h) internal fixation in the management of fractures of the neck of the femur. Injury 20(2):101–105
Orosz GM, Magaziner J, Hannan EL, Morrison RS, Koval K, Gilbert M et al (2004) Association of timing of surgery for hip fracture and patient outcomes. JAMA 291(14):1738–1743
Perez JV, Warwick DJ, Case CP, Bannister GC (1995) Death after proximal femoral fracture—an autopsy study. Injury 26(4):237–240
Rogers FB, Shackford SR, Keller MS (1995) Early fixation reduces morbidity and mortality in elderly patients with hip fractures from low-impact falls. J Trauma 39(2):261–265
Carretta E, Bochicchio V, Rucci P, Fabbri G, Laus M, Fantini MP (2011) Hip fracture: effectiveness of early surgery to prevent 30-day mortality. Int Orthop 35(3):419–424
McGuire KJ, Bernstein J, Polsky D, Silber JH (2004) The 2004 Marshall Urist award: delays until surgery after hip fracture increases mortality. Clin Orthop Relat Res 428:294–301
Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH (1995) Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am 77(10):1551–1556
Holt G, Smith R, Duncan K, Finlayson DF, Gregori A (2008) Early mortality after surgical fixation of hip fractures in the elderly: an analysis of data from the Scottish hip fracture audit. J Bone Joint Surg Br 90(10):1357–1363
Sund R, Liski A (2005) Quality effects of operative delay on mortality in hip fracture treatment. Qual Saf Health Care 14(5):371–377
Rodriguez-Fernandez P, Adarraga-Cansino D, Carpintero P (2011) Effects of delayed hip fracture surgery on mortality and morbidity in elderly patients. Clin Orthop Relat Res 469(11):3218–3221
Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ (2009) Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury 40(7):692–697
Ram GG, Govardhan P (2019) In-hospital mortality following proximal femur fractures in elderly population. Surg J (N Y) 5(2):e53–e56
Broos PL, Van Haaften KI, Stappaerts KH, Gruwez JA (1989) Hip fractures in the elderly. Mortality, functional results and social readaptation. Int Surg 74(3):191–194
Welford P, Jones CS, Davies G, Kunutsor SK, Costa ML, Sayers A, Whitehouse MR (2021) The association between surgical fixation of hip fractures within 24 hours and mortality: a systematic review and meta-analysis. Bone Joint J 103B(7):1176–1186
Lizaur-Utrilla A, Gonzalez-Navarro B, Vizcaya-Moreno MF, Miralles Muñoz FA, Gonzalez-Parreño S, Lopez-Prats FA (2019) Reasons for delaying surgery following hip fractures and its impact on one year mortality. Int Orthop 43(2):441–448
Folbert EC, Hegeman JH, Vermeer M, Regtuijt EM, van der Velde D, Ten Duis HJ et al (2017) Improved 1-year mortality in elderly patients with a hip fracture following integrated orthogeriatric treatment. Osteoporos Int 28(1):269–277
Keppler AM, Holzschuh J, Pfeufer D, Neuerburg C, Kammerlander C, Böcker W et al (2020) Postoperative physical activity in orthogeriatric patients—new insights with continuous monitoring. Injury 51(3):628–632
Gosch M, Hoffmann-Weltin Y, Roth T, Blauth M, Nicholas JA, Kammerlander C (2016) Orthogeriatric co-management improves the outcome of long-term care residents with fragility fractures. Arch Orthop Trauma Surg 136(10):1403–1409
Sabharwal S, Wilson H (2015) Orthogeriatrics in the management of frail older patients with a fragility fracture. Osteoporos Int 26(10):2387–2399
Abrahamsen C, Nørgaard B, Draborg E, Nielsen MF (2019) The impact of an orthogeriatric intervention in patients with fragility fractures: a cohort study. BMC Geriatr 19(1):268
Frost SA, Nguyen ND, Black DA, Eisman JA, Nguyen TV (2011) Risk factors for in-hospital post-hip fracture mortality. Bone 49(3):553–558
Henderson CY, Ryan JP (2015) Predicting mortality following hip fracture: an analysis of comorbidities and complications. Ir J Med Sci 184(3):667–671
Guzon-Illescas O, Perez Fernandez E, Crespí Villarias N, Quirós Donate FJ, Peña M, Alonso-Blas C et al (2019) Mortality after osteoporotic hip fracture: incidence, trends, and associated factors. J Orthop Surg Res 14(1):203
Moja L, Piatti A, Pecoraro V, Ricci C, Virgili G, Salanti G et al (2012) Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One 7(10):e46175
Menzies IB, Mendelson DA, Kates SL, Friedman SM (2012) The impact of comorbidity on perioperative outcomes of hip fractures in a geriatric fracture model. Geriatr Orthop Surg Rehabil 3(3):129–134
Holt G, Smith R, Duncan K, McKeown DW (2010) Does delay to theatre for medical reasons affect the peri-operative mortality in patients with a fracture of the hip? J Bone Joint Surg Br 92(6):835–841
Cha YH, Ha YC, Yoo JI, Min YS, Lee YK, Koo KH (2017) Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Arch Orthop Trauma Surg 137(5):625–630
Morri M, Ambrosi E, Chiari P, Orlandi Magli A, Gazineo D, D’Alessandro F, Forni C (2019) One-year mortality after hip fracture surgery and prognostic factors: a prospective cohort study. Sci Rep. 9(1):18718
Klestil T, Röder C, Stotter C, Winkler B, Nehrer S, Lutz M, Klerings I, Wagner G, Gartlehner G, Nussbaumer-Streit B (2018) Impact of timing of surgery in elderly hip fracture patients: a systematic review and meta-analysis. Sci Rep 8(1):13933
Kristiansson J, Hagberg E, Nellgård B (2020) The influence of time-to-surgery on mortality after a hip fracture. Acta Anaesthesiol Scand 64(3):347–353
Schoeneberg C, Aigner R, Pass B, Volland R, Eschbach D, Peiris SE, Ruchholtz S, Lendemans S, Alters Trauma Register DGU (2021) Effect of time-to-surgery on in-house mortality during orthogeriatric treatment following hip fracture: a retrospective analysis of prospectively collected data from 16,236 patients of the Alters Trauma Register DGU®. Injury 52(3):554–561
Kannegaard PN, van der Mark S, Eiken P, Abrahamsen B (2010) Excess mortality in men compared with women following a hip fracture. National analysis of comedications, comorbidity and survival. Age Ageing 39(2):203–209
Nordström P, Gustafson Y, Michaëlsson K, Nordström A (2015) Length of hospital stay after hip fracture and short term risk of death after discharge: a total cohort study in Sweden. BMJ 350:h696
Cree AK, Nade S (1999) How to predict return to the community after fractured proximal femur in the elderly. Aust N Z J Surg 69(10):723–725
González-Zabaleta J, Pita-Fernandez S, Seoane-Pillado T, López-Calviño B, Gonzalez-Zabaleta JL (2015) Dependence for basic and instrumental activities of daily living after hip fractures. Arch Gerontol Geriatr 60(1):66–70
Cummings SR, Kelsey JL, Nevitt MC, O’Dowd KJ (1985) Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev 7:178–208
Elmerson S, Zetterberg C, Andersson GB (1988) Ten-year survival after fractures of the proximal end of the femur. Gerontology 34(4):186–191
Holmberg S, Thorngren KG (1987) Statistical analysis of femoral neck fractures based on 3053 cases. Clin Orthop Relat Res 218:32–41
Gauthier JL, Hamelberg W (1963) Hip fractures. Influence of anesthesia on the patient’s hospital course. Anesth Analg 42:609–615
Sutcliffe AJ, Parker M (1994) Mortality after spinal and general anaesthesia for surgical fixation of hip fractures. Anaesthesia 49(3):237–240
Roberts KC, Brox WT, Jevsevar DS, Sevarino K (2015) Management of hip fractures in the elderly. J Am Acad Orthop Surg 23(2):131–137
Guay J, Parker MJ, Gajendragadkar PR, Kopp S (2016) Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev 2(2):CD000521
Van Waesberghe J, Stevanovic A, Rossaint R, Coburn M (2017) General vs. neuraxial anaesthesia in hip fracture patients: a systematic review and meta-analysis. BMC Anesthesiol 17(1):87
Gundel O, Thygesen LC, Gögenur I, Ekeloef S (2020) Postoperative mortality after a hip fracture over a 15-year period in Denmark: a national register study. Acta Orthop 91(1):58–62
Cornwall R, Gilbert MS, Koval KJ, Strauss E, Siu AL (2004) Functional outcomes and mortality vary among different types of hip fractures: a function of patient characteristics. Clin Orthop Relat Res 425:64–71
Kang H-Y, Yang K, Kim YN, Moon S, Choi W, Kang DR et al (2010) Incidence and mortality of hip fracture among the elderly population in South Korea: a population-based study using the national health insurance claims data. BMC Public Health 10(1):230
Lyles KW, Colón-Emeric CS, Magaziner JS, Adachi JD, Pieper CF, Mautalen C et al (2007) Zoledronic acid and clinical fractures and mortality after hip fracture. N Engl J Med 357(18):1799–1809
Acknowledgements
All authors have contributed significantly and that all authors are in agreement with the content of the manuscript.
Funding
Open access funding provided by Università degli Studi di Trieste within the CRUI-CARE Agreement. No funding was received to assist with the preparation of this manuscript. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Contributions
Study concept and design: LM; CR.; MZ. Acquisition of subjects and/or data: ADL; PDC. Analysis and interpretation of data: ADL; Preparation of manuscript: ADL, GC.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
Ethical approval was waived by the local Ethics Committee of University A in view of the retrospective nature of the study and all the procedures being performed were part of the routine care. Authors must state that the protocol for the research project has been approved by a suitably constituted Ethics Committee of the institution within which the work was undertaken and that it conforms to the provisions of the Declaration of Helsinki.
Informed consent
Informed consent was obtained from all individual participants included in the study. All investigations on human subjects must include a statement that the subject gave informed consent and patient anonymity should be preserved.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
De Luca, A., Murena, L., Zanetti, M. et al. Should the early surgery threshold be moved to 72 h in over-85 patients with hip fracture? A single-center retrospective evaluation on 941 patients. Arch Orthop Trauma Surg 143, 3091–3101 (2023). https://doi.org/10.1007/s00402-022-04509-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04509-y