Abstract
Introduction
Arthroscopic reconstruction techniques of the posterolateral corner (PLC) of the knee have been developed in recent years. Reconstruction techniques for higher-grade PLC injuries have not yet been validated in clinical studies. This study aimed to compare clinical outcomes of two different techniques and to present results of the first prospective randomized clinical trial of patients to undergo these novel procedures.
Materials and methods
19 patients with Fanelli Type B posterolateral corner injuries and additional posterior cruciate ligament ruptures were included in this prospective study. They were randomly assigned to one of two novel arthroscopic reconstruction techniques, based on open surgeries developed by Arciero (group A) and LaPrade (group B). Follow-up was conducted at 6 and 12 months postoperatively and included clinical examinations for lateral, rotational and posterior stability, range of motion and subjective clinical outcome scores (IKDC Subjective Score, Lysholm Score, Tegner Activity Scale and Numeric Rating Scale for pain).
Results
At 6 and 12 months postoperative, all patients in both groups presented stable to varus, external rotational and posterior forces, there were no significant differences between the two groups. At 12-month follow-up, group A patients showed significantly higher maximum flexion angles (134.17° ± 3.76° vs. 126.60° ± 4.22°; p = 0.021) compared to patients of group B. Duration of surgery was significantly longer in Group B patients than in group A (121.88 ± 11.63 vs. 165.00 ± 35.65 min; p = 0.003). Posterior drawer (side-to-side difference) remained more reduced in group A (2.50 ± 0.69 mm vs. 3.27 ± 0.92 mm; p = 0.184). Subjective patient outcome scores showed no significant differences between groups (Lysholm Score 83.33 ± 7.79 vs. 86.40 ± 9.21; p = 0.621).
Conclusions
This study indicates sufficient restoration of posterolateral rotational instability, varus instability and posterior drawer after arthroscopic posterolateral corner reconstruction without neurovascular complications.
Increased postoperative range of motion and a shorter and less invasive surgical procedure could favor the arthroscopic reconstruction technique according to Arciero over LaPrade’s technique in future treatment considerations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The posterolateral corner of the knee consists of the lateral/fibular collateral ligament (LCL/FCL) and the popliteus complex (PTC). The popliteus complex itself contains the popliteus muscle tendon unit (PLT) and the arcuate complex (AC), which is formed by the popliteofibular ligament (PFL), the fabellofibular ligament and the popliteomeniscal fibers [1]. It has a highly complex stabilizing function against various forces to the knee. The popliteus complex serves as the most important static and dynamic stabilizer against external tibial rotation and posterior tibial translation [2,3,4] while the lateral collateral ligament provides stability against varus forces [5].
In recent years, arthroscopic reconstruction techniques have been developed to provide stability while utilizing the benefits of arthroscopic compared to open surgeries [6]. Advantages of arthroscopic procedures include a better visualization of anatomical landmarks for drill tunnel placements, minimal soft tissue damage, lower infection rates and especially a better protection of the common peroneal nerve since its preparation and visualization is obsolete [1].
For lower-grade instabilities (Fanelli Type A, PoLIS LI-A) [7], anatomic reconstruction of the popliteus complex (popliteus bypass) has shown promising results [8,9,10]. Novel arthroscopic techniques for anatomical reconstruction in higher-grade instabilities (Fanelli Type B or C, PoLIS LI-B or LI-C [7]), based on Arciero’s and LaPrade’s procedures, have recently been described by Frings et al., and Kolb et al. [11,12,13]. In a biomechanical evaluation of an arthroscopic reconstruction according to Arciero, a nearly normal stability of the knee could be restored [13].
So far, clinical results of these reconstruction techniques remained elusive. In this study, we aimed to detect differences in clinical outcomes of arthroscopic anatomical PLC reconstruction techniques described by Frings et al.. and Kolb et al.. and to present results of the first prospective randomized clinical trial of patients to undergo these procedures.
We hypothesized that both procedures can sufficiently restore posterior, lateral and external rotational stability in high-grade posterolateral corner injuries and that there would be no differences in clinical outcome between the two groups.
Material and methods
This study was approved by the local ethics committee of the regional medical association (PV7212). Informed consent was obtained by each patient in this study.
Preoperative assessment
Patients who presented to our clinic between years 2018–2020 with high-grade injuries (Fanelli Type B, PoLIS LI-B [7]) to the posterolateral corner and consent to participate were included in this study. Inclusion criteria were chronic injuries (> 3 weeks) with a combined varus and posterolateral rotational instability and additional posterior instability due to injury to the posterior cruciate ligament. Patients with higher-grade posterolateral corner injuries and additional affected structures (biceps femoris muscle tendon rupture, iliotibial band injury, fracture of the fibular head, etc.) were excluded from this study, as they required additional open surgery to address these specific structures. Fanelli type A injuries were excluded as well.
Preoperative clinical evaluation was performed by an experienced and fellowship trained orthopedic surgeon and included the posterior drawer test in neutral, internal, and external rotation in 30° and 90° of knee flexion (dial test); lateral and medial gapping under varus and valgus stress opening in full extension and 20°–30° of flexion. Stress radiographs in 90° of flexion and neutral rotation were performed on the injured and non-injured knee to objectify the side-to-side difference of the posterior translation. Additionally, all patients underwent magnetic resonance imaging of the knee.
Surgical procedure
The type of surgical procedure was determined by block randomization, dividing patients into two subgroups. Surgeries were conducted strictly according to arthroscopic posterolateral corner reconstruction techniques described by Frings et al. [11] (Arciero’s technique, group A) and Kolb et al. [12] (LaPrade’s technique, Group B) (Fig. 1). Surgeries were all performed by the same surgeon with high expertise in arthroscopic knee surgery. Additional PCL reconstruction was performed arthroscopically during the same procedure [14]. The duration of the surgery was evaluated (starting from skin incision, including tendon harvest and all arthroscopic procedures until skin closure). Furthermore, length of stay as a hospital inpatient and surgery-related complications were investigated.
Schematic drawings of the two different techniques for posterolateral corner reconstruction in posterior (left) and lateral view (right). a Fibula-based, single-graft reconstruction technique based on Arciero’s technique for open PLC reconstruction (group A). b Tibio-fibular-based, double-graft technique according to LaPrade’s procedure (group B)
Rehabilitation
The first 2 weeks after surgery patients wore a PCL brace (Jack PCL Brace; Albrecht, Bernau am Chiemsee, Germany) with a maximum flexion of the knee of 20°. Passive flexion of the knee was performed up to 40° of flexion in prone position by physical therapists after drain removal. Patients were allowed partial weight bearing of 20 kg on crutches for 6 weeks.
In weeks 3 and 4, patients were passively mobilized up to 60° of flexion and then to 90° in weeks 5 and 6 while increasing weight bearing to half of their body weight. The brace was recommended with limited range-of-motion for 6 weeks (day and night) and for another 6 weeks without limited range-of-motion.
After 6 weeks, patients were allowed full range of motion and started full weight bearing. Additionally, active flexion of the knee against gravity and cycling was allowed.
Forced flexion against resistance was allowed after 12 weeks, simultaneously jogging was permitted. Stop-and-go sports were allowed depending on individual return-to-play and return-to-competition tests after 6–9 months.
Follow-up
Follow-up was conducted at 6 and 12 months after surgery by a single author, who was blinded to the type of surgical procedure to avoid bias. Clinical examination of range of motion and external rotation in 30° and 90° of flexion was performed with the use of a HALO Goniometer® (HALO, model HG1, HALO Medical Devices, Australia) [15]. Posterior drawer tests were measured with a Rolimeter® in the technique according to Höher et al. [16]. Varus instabilities were examined in 30° of knee flexion. All examinations were also performed on the contralateral knee and parameters were evaluated as side-to-side differences.
Subjective scores included the IKDC subjective score, the Lysholm Score and Tegner Activity Scale (TAS) as well as a Numeric Rating Scale (NRS) for current pain at time of follow-up. All of the above subjective scores are validated and were presented in the German version, as it was the native language of all included patients [17,18,19].
Statistical analysis
Statistical analysis was performed using SPSS 26.0 (SPSS Inc, Chicago, IL). Mean values ± standard deviations were reported for all parameters. Statistical tests were performed as Mann–Whitney test, all tests were non-parametric test and statistical significance was set at p < 0.05. As this study was designated as a pilot study of rare injuries, power analysis was not applicable.
Results
19 patients were included in this study, four patients were lost to follow-up for geographical reasons.
All patients in both groups initially presented with chronic Fanelli Type B injuries with varus opening up to 10 mm, an increased external rotational instability in dial test compared to the contralateral knee and subjective instability. There were not relevant comorbidities in patients of either group which would have influenced patient outcomes, as higher-grade instabilities were not included and there was no preexistence of arthrofibrosis. There was no significant difference in patient age at the time of surgery (p = 0.356) or the extent of preoperative posterior drawer as side-to-side difference between groups A and B. Duration of surgery was significantly longer in Group B patients than in group A (165.00 ± 35.65 vs. 121.88 ± 11.63 min; p = 0.003). There was no significant difference in the duration of in-hospital stay and one surgery-related complication was present in each group (Table 1). There were no neurovascular complications of the surgical procedures.
All patients in both groups received additional PCL reconstruction during the same surgical procedure.
At 6-month follow-up, patients of group A showed similar flexion angles as group B, a slightly reduced remaining posterior drawer, a larger external rotation deficit at 30° of knee flexion and a smaller external rotation deficit at 90° of knee flexion compared to group B, all measured as side-to-side differences.
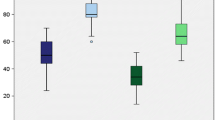
At 12 month follow-up, group A patients showed significantly better maximum flexion angles (134.17° ± 3.76° vs. 126.60° ± 4.22°; p = 0.021) compared to patients of group B. Posterior drawer (side-to-side difference) remained more reduced in group A compared to the preoperative state (2.50 ± 0.69 mm vs. 3.27 ± 0.92; p = 0.184). Group B showed less restraints in external rotation at 30° of flexion and slightly more restraints at 90° of flexion (Fig. 2). The patient of group B who showed arthrofibrosis had a preoperative range-of-motion of 130° (extension/flexion: 0–0–130°) and postoperative range-of-motion of 105° (extension/flexion: 0–5–110°) and was the only patient to present with an extension deficit.
Clinical results at 6- and 12-month follow-up. a Maximum flexion angles of the injured knees. Flexion angles at 12 months postoperative were significantly higher in group A (indicated by asterisk, p = 0.021). b Posterior drawer measured via Rolimeter ® as side-to-side difference to the contralateral knee. c External rotation at 30° of knee flexion, measured as a side-to-side-difference. d External rotation at 90° of knee flexion, measured as a side-to-side-difference. No other parameter showed statistically significant differences between the two groups at any given time point. Graphs are drawn as mean values ± standard deviation
All patients of both groups presented stable under varus stress at 6- and 12-month follow-up.
Aside from maximum flexion angles at 12 months, none of the above listed differences between the two groups showed statistical significance (Table 2).
Subjective scores showed a higher IKDC Subjective Score and Lysholm Score, as well as lower average pain in the injured knee at 6-month follow-up in Group A. None of these differences proved to be statistically significant (Fig. 3).
Clinical subjective scores at 6- and 12-month follow-up. a IKDC subjective score (range 0–100). b Lysholm score (range 0–100). c Tegner Activity Scale (range 0–10). d Numeric Rating Scale (range 0–10), describing current average pain in the injured knee at time of follow-up. No parameter showed statistically significant differences between the two groups at any given time point. Graphs are drawn as mean values ± standard deviation
All other subjective parameters only showed minor differences between groups (Table 3). Only one patient in each group reported intermittent subjective instability, all other patients described their knee as subjectively stable.
Discussion
The most important findings of the present study were that all patients in both groups showed sufficient restoration of posterior, rotational and lateral joint stability in clinical examinations at both follow-up time points, as it was hypothesized in the aim of this study. Only two patients reported intermittent subjective instability which was not confirmed in objective clinical examinations and may be contributed to remaining muscular deficits. As restoration of objective and subjective joint stability was the primary indication for surgical treatment, arthroscopic reconstruction of the posterolateral corner in both techniques can be interpreted as successful.
In chronic injuries with high grade posterolateral rotational instabilities (Fanelli Type B or C, PoLIS LI-B or LI-C [7]), reconstruction has shown superior results compared to repair of injured structures [20,21,22,23]. While there are a variety of different surgical approaches to non-anatomic and anatomic reconstructions (fibular-/tibia-based, single-/multi-graft), anatomic reconstructions developed by Arciero et al. [24] and LaPrade et al. [25] have shown the most promising biomechanical and clinical results [26,27,28]. They are well established as open surgical procedures [29] and have shown equal restoration of joint stability in biomechanical studies [30].
As this study aimed to detect potential differences between the two surgical procedures, the only statistically significant outcome measure was the group A patients’ increased maximum flexion angle at 12 months postoperative as a relevant factor in judgement of functional outcomes. Aside from range of motion, only minor differences without statistical significance in objective and subjective outcome measures were found. Yet, further non-significant tendencies seemed to also show slightly better functional results in group A, displayed in postoperative posterior drawer and higher subjective outcome scores (IKDC, Lysholm, Tegner Activity Scale, NRS) after 6 months. These findings are in line with biomechanical studies of Treme et al., and Vezeridis et al. [30, 31], who showed similar results in restoration of joint stability against varus and external rotation forces with both surgical procedures. Drenck et al. [10] showed that reconstruction of the posterolateral corner via popliteus bypass graft, as it is performed in LaPrade’s procedure (group B), provides sufficient stability against external rotational forces. Clinical results of arthroscopic reconstruction in low-grade (Fanelli Type A) PLC injuries showed similar outcomes to open procedures [9].
This is also confirmed by our study as patients (in both groups) showed sufficient restoration of rotational stability with even a slight overconstraint in external rotation compared to the contralateral knee, yet there were no significant differences between the two groups.
Additionally to their clinical outcomes, both procedures need to be evaluated with regard to their invasiveness and risk of complications.
The surgical procedure took significantly longer in group B compared to group A patients and therefore is accompanied by an increased risk for general surgical complications (e.g., postoperative infection, pain, deep vein thrombosis) [32, 33]. It has to be considered that all patients received additional PCL reconstruction during the same surgery. As the PCL reconstruction technique was identical in every surgery, longer duration of surgery has to be attributed to the inherent differences of the two procedures.
Arciero’s technique [11] (group A) is a fibular-based, single-graft technique, while LaPrade’s technique [12] (group B) is a tibio-fibular-based, double-graft technique. The tibial fixation aspect in LaPrade’s technique aims to provide a more anatomic reconstruction but has also to be seen as a more invasive procedure. Additional preparation and establishment of the tibial drill tunnel presents additional trauma (and risk of collision with a tibial drill tunnel of the PCL graft), while the larger number of grafts increases scar tissue formation and therefore risk of reduced flexibility and arthrofibrosis [34, 35]. This aspect is confirmed by the reduced maximum flexion angles of group B patients after 12 months (126.60° ± 4.22° vs. 134.17° ± 3.76°; p = 0.021). One patient of group B in our study presented with arthrofibrosis that required revision arthrolysis surgery. The number of needed grafts is also highly relevant if patient autografts are used, as risk of donor site morbidity is increased with additional tendon harvests [36, 37]. While some experts in the field of PLC reconstruction, especially in North America, favorably use allografts, autografts are still the most widely used type of tendon graft [29].
With the above-mentioned differences between the two procedures, the procedure described by Frings et al. (Arciero’s procedure) appears to be less invasive while providing similar clinical results. The procedure described by Kolb et al. (LaPrade’s procedure) has the benefit of providing additional stability in cases of tibiofibular joint injuries.
Arthroscopic reconstruction of the posterolateral corner requires profound knowledge of anatomic relations, but has the advantage of allowing visualization of all key structures including the posteromedial aspect of the fibular head to place a fibular drill tunnel under visual instead of palpatory control [38, 39]. Aside from general benefits of arthroscopic compared to open surgery such as lower infection rates, less scar tissue, faster rehabilitation and less pain, this allows for improved fibular tunnel placement. While some experts have raised concerns that arthroscopic PLC reconstructions bear a higher risk of tunnel misplacement and neurovascular injuries [40, 41], our clinical results showed no neurovascular or tunnel-related complications. Studies have shown that development of a transseptal portal and posterolateral arthroscopy can be performed safely at intraoperative knee flexion of 90° [38, 42,43,44]. The absence of postoperative common peroneal nerve damage symptoms in our study suggests that arthroscopic fibular drill tunnel placement does not cause neurovascular damage as commonly as recent studies have described [45]. While lack of intraoperative complications could be attributed to the small size of our study group, the common peroneal nerve injury rate of up to 57% in open fibular drill tunnel placement, as presented by Hohmann et al., in a cadaveric study, appears to be unlikely from our perspective and is not reflected in our clinical experience. Certainly, success of arthroscopic PLC reconstruction is strongly dependent on the surgeon’s experience in the field of arthroscopic reconstructive knee surgery.
Limitations
This study has several limitations. First of all, the size of our study group is limited, due to the rare nature of these injuries especially in the pandemic situation of the last 18 months. Differences between the groups have a higher risk of being coincidental, as statistical evaluation showed no significant differences in most outcome measures.
Furthermore, while inclusion and exclusion criteria were very precise, time between injury and surgery showed variability, but was always > 3 weeks and therefore considered as a chronic injury.
Follow-up clinical examinations were performed via Rolimeter® instead of stress radiographs. While evaluation of posterior drawer and lateral instability in the injured state is commonly performed with stress radiographs, follow-up examinations have shown equally reliable results with these devices [16].
Conclusion
This study indicates sufficient restoration of posterolateral rotational instability, varus instability and posterior drawer after arthroscopic posterolateral corner reconstruction without neurovascular complications with an excellent radiographic and clinical outcome.
Increased postoperative range of motion and a shorter and less invasive surgical procedure could favor the arthroscopic reconstruction technique according to Arciero over LaPrade’s technique in future treatment considerations.
References
Frosch KH, Akoto R, Heitmann M, Enderle E, Giannakos A, Preiss A (2015) Arthroscopic reconstruction of the popliteus complex: accuracy and reproducibility of a new surgical technique. Knee Surg Sports Traumatol Arthrosc 23(10):3114–3120. https://doi.org/10.1007/s00167-014-3000-y
LaPrade RF, Johansen S, Agel J, Risberg MA, Moksnes H, Engebretsen L (2010) Outcomes of an anatomic posterolateral knee reconstruction. J Bone Joint Surg Am 92(1):16–22. https://doi.org/10.2106/JBJS.I.00474
Domnick C, Frosch KH, Raschke MJ, Vogel N, Schulze M, von Glahn M et al (2017) Kinematics of different components of the posterolateral corner of the knee in the lateral collateral ligament-intact state: a human cadaveric study. Arthroscopy 33(10):1821–1830. https://doi.org/10.1016/j.arthro.2017.03.035
Thaunat M, Pioger C, Chatellard R, Conteduca J, Khaleel A, Sonnery-Cottet B (2014) The arcuate ligament revisited: role of the posterolateral structures in providing static stability in the knee joint. Knee Surg Sports Traumatol Arthrosc 22(9):2121–2127. https://doi.org/10.1007/s00167-013-2643-4
Pache S, Aman ZS, Kennedy M, Nakama GY, Moatshe G, Ziegler C et al (2018) Posterior cruciate ligament: current concepts review. Arch Bone Joint Surg 6(1):8–18
Weiss S, Krause M, Frosch KH (2020) Posterolateral corner of the knee: a systematic literature review of current concepts of arthroscopic reconstruction. Arch Orthop Trauma Surg 140(12):2003–2012. https://doi.org/10.1007/s00402-020-03607-z
Weiler A, Frosch KH, Gwinner C, Strobel MJ, Lobenhoffer P (2021) The Posterolateral Instability Score (PoLIS) of the knee joint: a guideline for standardized documentation, classification, and surgical decision-making. Knee Surg Sports Traumatol Arthrosc 29(3):889–899. https://doi.org/10.1007/s00167-020-06044-y
Frosch KH, Akoto R, Drenck T, Heitmann M, Pahl C, Preiss A (2016) Arthroscopic popliteus bypass graft for posterolateral instabilities of the knee: a new surgical technique. Oper Orthop Traumatol 28(3):193–203. https://doi.org/10.1007/s00064-015-0432-6
Li Y, Zhang H, Zhang J, Li X, Zheng T, Zhang Z et al (2019) The Clinical outcome of arthroscopic versus open popliteal tendon reconstruction combined with posterior cruciate ligament reconstruction in patients with type a posterolateral rotational instability. Arthroscopy 35(8):2402–2409. https://doi.org/10.1016/j.arthro.2019.03.019
Drenck TC, Frings J, Preiss A, Muellner M, Akoto R, Alm L et al (2021) The treatment of posterolateral knee instability with combined arthroscopic popliteus bypass and PCL reconstruction provides good-to-excellent clinical results in the mid-term follow-up. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06590-z
Frings J, Kolb JP, Drenck TC, Krause M, Alm L, Akoto R et al (2019) Anatomic Reconstruction of the Posterolateral Corner: An All-Arthroscopic Technique. Arthrosc Tech 8(2):e153–e161. https://doi.org/10.1016/j.eats.2018.10.010
Kolb JPF, Krause JM, Frosch KH (2019) LaPrade’s procedure as an all-arthroscopic technique for posterolateral corner reconstruction. Arthrosc Tech 8:999
Liu P, Gong X, Zhang J, Ao Y (2020) Anatomic, all-arthroscopic reconstruction of posterolateral corner of the knee: a cadaveric biomechanical study. Arthroscopy 36(4):1121–1131. https://doi.org/10.1016/j.arthro.2019.10.035
Zorzi C, Alam M, Iacono V, Madonna V, Rosa D, Maffulli N (2013) Combined PCL and PLC reconstruction in chronic posterolateral instability. Knee Surg Sports Traumatol Arthrosc 21(5):1036–1042. https://doi.org/10.1007/s00167-011-1771-y
Correll S, Field J, Hutchinson H, Mickevicius G, Fitzsimmons A, Smoot B (2018) Reliability and validity of the halo digital goniometer for shoulder range of motion in healthy subjects. Int J Sports Phys Ther 13(4):707–714
Hoher J, Akoto R, Helm P, Shafizadeh S, Bouillon B, Balke M (2015) Rolimeter measurements are suitable as substitutes to stress radiographs in the evaluation of posterior knee laxity. Knee Surg Sports Traumatol Arthrosc 23(4):1107–1112. https://doi.org/10.1007/s00167-014-2901-0
Kummel D, Preiss S, Harder LP, Leunig M, Impellizzeri FM (2018) Measurement properties of the German version of the IKDC subjective knee form (IKDC-SKF). J Patient Rep Outcomes 2:31. https://doi.org/10.1186/s41687-018-0058-1
Wirth B, Liffert F, de Bruin ED (2011) Development and evaluation of a German version of the Lysholm score for measuring outcome after anterior cruciate ligament injuries. Sportverletz Sportschaden 25(1):37–43. https://doi.org/10.1055/s-0029-1245825
Wirth B, Meier N, Koch PP, Swanenburg J (2013) Development and evaluation of a German version of the Tegner activity scale for measuring outcome after anterior cruciate ligament injury. Sportverletz Sportschaden 27(1):21–27. https://doi.org/10.1055/s-0032-1330752
Stannard JP, Stannard JT, Cook JL (2015) Repair or reconstruction in acute posterolateral instability of the knee: decision making and surgical technique introduction. J Knee Surg 28(6):450–454. https://doi.org/10.1055/s-0035-1563403
Kennedy MI, Bernhardson A, Moatshe G, Buckley PS, Engebretsen L, LaPrade RF (2019) Fibular collateral ligament/ posterolateral corner injury: when to repair, reconstruct, or both. Clin Sports Med 38(2):261–274. https://doi.org/10.1016/j.csm.2018.11.002
McCarthy M, Ridley TJ, Bollier M, Cook S, Wolf B, Amendola A (2015) Posterolateral knee reconstruction versus repair. Iowa Orthop J 35:20–25
Gormeli G, Gormeli CA, Elmali N, Karakaplan M, Ertem K, Ersoy Y (2015) Outcome of the treatment of chronic isolated and combined posterolateral corner knee injuries with 2- to 6-year follow-up. Arch Orthop Trauma Surg 135(10):1363–1368. https://doi.org/10.1007/s00402-015-2291-x
Arciero RA (2005) Anatomic posterolateral corner knee reconstruction. Arthroscopy 21(9):1147. https://doi.org/10.1016/j.arthro.2005.06.008
LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A (2004) An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med 32(6):1405–1414. https://doi.org/10.1177/0363546503262687
Moulton SG, Geeslin AG, LaPrade RF (2016) A systematic review of the outcomes of posterolateral corner knee injuries, part 2: surgical treatment of chronic injuries. Am J Sports Med 44(6):1616–1623. https://doi.org/10.1177/0363546515593950
LaPrade RF, Johansen S, Engebretsen L (2011) Outcomes of an anatomic posterolateral knee reconstruction: surgical technique. J Bone Joint Surg Am 93(Suppl 1):10–20. https://doi.org/10.2106/JBJS.J.01243
Rios CG, Leger RR, Cote MP, Yang C, Arciero RA (2010) Posterolateral corner reconstruction of the knee: evaluation of a technique with clinical outcomes and stress radiography. Am J Sports Med 38(8):1564–1574. https://doi.org/10.1177/0363546510363462
Gelber PE, Drager J, Maheshwer B, Leyes M, Barenius B, Robinson J et al (2020) Large variability exists in the management of posterolateral corner injuries in the global surgical community. Knee Surg Sports Traumatol Arthrosc 28(7):2116–2123. https://doi.org/10.1007/s00167-020-05922-9
Treme GP, Salas C, Ortiz G, Gill GK, Johnson PJ, Menzer H et al (2019) A biomechanical comparison of the arciero and laprade reconstruction for posterolateral corner knee injuries. Orthop J Sports Med 7(4):2325967119838251. https://doi.org/10.1177/2325967119838251
Vezeridis PS, Engler ID, Salzler MJ, Hosseini A, Gwathmey FW Jr, Li G et al (2020) Biomechanics following isolated posterolateral corner reconstruction comparing a fibular-based docking technique with a tibia and fibular-based anatomic technique show either technique is acceptable. Arthroscopy 36(5):1376–1385. https://doi.org/10.1016/j.arthro.2019.12.007
Salzler MJ, Lin A, Miller CD, Herold S, Irrgang JJ, Harner CD (2014) Complications after arthroscopic knee surgery. Am J Sports Med 42(2):292–296. https://doi.org/10.1177/0363546513510677
Friberger Pajalic K, Turkiewicz A, Englund M (2018) Update on the risks of complications after knee arthroscopy. BMC Musculoskelet Disord 19(1):179. https://doi.org/10.1186/s12891-018-2102-y
Patel NK, Lian J, Nickoli M, Vaswani R, Irrgang JJ, Lesniak BP et al (2021) Risk factors associated with complications after operative treatment of multiligament knee injury. Orthop J Sports Med 9(3):2325967121994203. https://doi.org/10.1177/2325967121994203
Lee JH, Cook JL, Wilson N, Rucinski K, Stannard JP (2020) Outcomes after multiligament knee injury reconstruction using novel graft constructs and techniques. J Knee Surg. https://doi.org/10.1055/s-0040-1716356
Strauss MJ, Varatojo R, Boutefnouchet T, Condello V, Samuelsson K, Gelber PE et al (2019) The use of allograft tissue in posterior cruciate, collateral and multi-ligament knee reconstruction. Knee Surg Sports Traumatol Arthrosc 27(6):1791–1809. https://doi.org/10.1007/s00167-019-05426-1
Sun J, Wei XC, Li L, Cao XM, Li K, Guo L et al (2020) Autografts vs synthetics for cruciate ligament reconstruction: a systematic review and meta-analysis. Orthop Surg 12(2):378–387. https://doi.org/10.1111/os.12662
Frings J, Weiss S, Kolb J, Behrendt P, Frosch KH, Krause M (2021) Arthroscopic anatomy of the posterolateral corner of the knee: anatomic relations and arthroscopic approaches. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-021-03864-6
Krause M, Akoto R, Drenck TC, Frosch KH, Preiss A (2019) Posterolateral rotatory knee instability-mri evaluation of anatomic landmarks for tibial drill tunnel placement in open and arthroscopic popliteus tendon reconstruction. J Knee Surg 32(7):667–672. https://doi.org/10.1055/s-0038-1666832
Chahla J, Murray IR, Robinson J, Lagae K, Margheritini F, Fritsch B et al (2019) Posterolateral corner of the knee: an expert consensus statement on diagnosis, classification, treatment, and rehabilitation. Knee Surg Sports Traumatol Arthrosc 27(8):2520–2529. https://doi.org/10.1007/s00167-018-5260-4
Chahla J, Williams BT, LaPrade RF (2020) Editorial commentary: shedding light on the posterolateral corner of the knee: can we do it with the scope? is there a real benefit? Arthroscopy 36(4):1132–1134. https://doi.org/10.1016/j.arthro.2020.01.030
Ahn JH, Lee SH, Jung HJ, Koo KH, Kim SH (2011) The relationship of neural structures to arthroscopic posterior portals according to knee positioning. Knee Surg Sports Traumatol Arthrosc 19(4):646–652. https://doi.org/10.1007/s00167-010-1326-7
Makridis KG, Wajsfisz A, Agrawal N, Basdekis G, Djian P (2013) Neurovascular anatomic relationships to arthroscopic posterior and transseptal portals in different knee positions. Am J Sports Med 41(7):1559–1564. https://doi.org/10.1177/0363546513492704
Kim SJ, Song HT, Moon HK, Chun YM, Chang WH (2011) The safe establishment of a transseptal portal in the posterior knee. Knee Surg Sports Traumatol Arthrosc 19(8):1320–1325. https://doi.org/10.1007/s00167-011-1429-9
Hohmann E, Van Zyl R, Glatt V, Tetsworth K, Keough N (2021) The anatomical relationship of the common peroneal nerve to the proximal fibula and its clinical significance when performing fibular-based posterolateral reconstructions. Arch Orthop Trauma Surg 141(3):437–445. https://doi.org/10.1007/s00402-020-03708-9
Acknowledgements
None.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study received no external funding.
Author information
Authors and Affiliations
Contributions
SW, MK, KHF were involved in design and conceptualization of this study. SW was responsible for patient examinations, manuscript drafting and statistical analysis. MK and KHF critically revised the manuscript. Surgeries were performed by KHF. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest. The authors did not receive support from any organization for the submitted work.
Ethical approval
This study was approved by the local ethics committee of the regional medical association (PV7212).
Informed consent
Informed consent was obtained from all patients involved in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Weiss, S., Krause, M. & Frosch, KH. Clinical results after arthroscopic reconstruction of the posterolateral corner of the knee: A prospective randomized trial comparing two different surgical techniques. Arch Orthop Trauma Surg 143, 967–975 (2023). https://doi.org/10.1007/s00402-022-04403-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04403-7