Abstract
Introduction
The anterior cervical spine approach is safe and effective in many cervical spine pathologies. It is considered one of the most common approaches in spine surgery. Postoperative infections after anterior cervical surgery are rare but serious.
Materials and methods
This study is a retrospective database analysis. In this study, the incidence, and the local risk factors of postoperative infection after anterior-only sub-axial cervical spine surgery in a high-volume spine center were analyzed. The data of patients operated in a teaching hospital is electronically stored in a comprehensive medical database program. Postoperative infection after anterior cervical surgery from C2 to C7 was calculated and analyzed. In the study period, 4897 patients were operated. Twenty-four infections after a primary aseptic operation were detected. Independent local risk factors were estimated.
Results
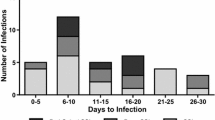
Postoperative infection occurred in 24/4897 patients (0.49%). The incidence of infection after cervical trauma was 3% (7/229), after spinal cord injury 4.3% (2/46), with myelopathy 1.98% (11/556), and after revision surgery 1.25% (7/560). The incidence showed a significant increase (p = 0.00, 0.01, 0.02). In 14 of the postoperatively infected patients (58.3%) an oesophageal injury was diagnosed. Odds ratios (OR) with a confidence interval (CI) of 95% was calculated. Independent risk factors for the postoperative infections were: Cervical trauma (OR 8.59, 95% CI 3.52–20.93), revision surgery (OR 3.22, 95% CI 1.33–7.82), The presence of cervical myelopathy (OR 6.71, 95% CI 2.99–15.06), and spinal cord injury (OR 9.33, 95% CI 2.13–40.83).
Conclusions
Postoperative infection after anterior cervical surgery is low (0.49%). In addition to the general risk factor for infection, the local risk factors are trauma, myelopathy, spinal cord injury, and revision surgeries. In the case of postoperative infection, an oesophageal injury should be excluded.

Similar content being viewed by others
References
Park SA, Lee JH, Nam YS, An X, Han SH, Ha KY (2013) Topographical anatomy of the anterior cervical approach for c2–3 level. Eur Spine J 22(7):1497–1503
Lu J, Ebraheim NA, Nadim Y, Huntoon M (2000) Anterior approach to the cervical spine: surgical anatomy. Orthopedics 23:841–845
Cloward RB. (1958) The Anterior Approach for Removal of Ruptured Cervical Disks. J Neurosurg [Internet]. 15(6):602–17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/13599052
Khalid SI, Kelly R, Wu R, Peta A, Carlton A, Adogwa O (2019) A comparison of readmission and complication rates and charges of inpatient and outpatient multiple-level anterior cervical discectomy and fusion surgeries in the medicare population. J Neurosurg Spine 31(4):486–492
McClelland S, Oren JH, Protopsaltis TS, Passias PG (2016) Outpatient anterior cervical discectomy and fusion: a meta-analysis. J Clin Neurosci 34:166–168
Ban, D., Liu, Y., Cao, T. et al. Safety of outpatient anterior cervical discectomy and fusion: a systematic review and meta-analysis. Eur J Med Res 21, 34 (2016). https://doi.org/10.1186/s40001-016-0229-6
Tasiou A, Giannis T, Brotis AG, Siasios I, Georgiadis I, Gatos H et al (2017) Anterior cervical spine surgery-associated complications in a retrospective case-control study. J Spine Surg 3:444–459
Halani SH, Baum GR, Riley JP, Pradilla G, Refai D, Rodts GE et al (2016) Esophageal perforation after anterior cervical spine surgery: a systematic review of the literature. J Neurosur Spine 25:285–291
Yee TJ, Swong K, Park P (2020) Complications of anterior cervical spine surgery: a systematic review of the literature. J Spine Surg 6(1):302–322
John McLellan Tew, Jr., M.D., F.A.C.S., Frank H. Mayfield, M.D., F.A.C.S., (1976) Complications of Surgery of the Anterior Cervical Spine, Neurosurgery, 23(1):424–434, https://doi.org/10.1093/neurosurgery/23.CN_suppl_1.424
Epstein NE (2019) A review of complication rates for anterior cervical diskectomy and fusion (ACDF). Surg Neurol Int 7(10):100
Gamain R, Coulomb R, Houzir K, Molinari N, Kouyoumdjian P, Lonjon N (2019) Anterior cervical spine surgical site infection and pharyngoesophageal perforation. Ten-year incidence in 1475 patients. Orthop Traumatol Surg Res 105(4):697–702
Wimmer C, Gluch H, Franzreb M, Ogon M (1998) Predisposing factors for infection in spine surgery: a survey of 850 spinal procedures. J Spinal Disord 11(2):124–128
Tubaki VR, Rajasekaran S, Shetty AP. (2013) Effects of using intravenous antibiotic only versus local intrawound vancomycin antibiotic powder application in addition to intravenous antibiotics on postoperative infection in spine surgery in 907 patients. Spine (Phila Pa 1976) . 38(25):2149–55. Available from: http://journals.lww.com/00007632-201312010-00003
Dowdell J, Brochin R, Kim J, Overley S, Oren J, Freedman B et al (2018) Postoperative spine infection: diagnosis and management. Glob Spine J 8(4):37S-43S
Yao R, Zhou H, Choma TJ, Kwon BK, Street J (2018) Surgical site infection in spine surgery: Who is at risk? Glob Spine J 8(4_suppl):5S-30S
Kwon BK, Fisher CG, Boyd MC, Cobb J, Jebson H, Noonan V et al (2007) A prospective randomized controlled trial of anterior compared with posterior stabilization for unilateral facet injuries of the cervical spine. J Neurosurg Spine 7(1):1–12
Gruskay J, Kepler C, Smith J, Radcliff K, Vaccaro A. (2012) Is Surgical Case Order Associated With Increased Infection Rate After Spine Surgery? Spine (Phila Pa 1976). 37(13):1170–4. Available from: http://journals.lww.com/00007632-201206010-00012
Vakhitova ZI, Alston-Knox CL (2018) Non-significant p-values? Strategies to understand and better determine the importance of effects and interactions in logistic regression. PLoS ONE 13(11):e0205076. https://doi.org/10.1371/journal.pone.0205076
Fountas KN, Kapsalaki EZ, Nikolakakos LG, Smisson HF, Johnston KW, Grigorian AA, et al. (2007) Anterior Cervical Discectomy and Fusion Associated Complications. Spine (Phila Pa 1976) 32(21):2310–7. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00007632-200710010-00006
Bertalanffy H, Eggert HR (1989) Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien) 99(1–2):41–50
Christiano LD, Goldstein IM. (2011) Late Prevertebral Abscess After Anterior Cervical Fusion. Spine (Phila Pa 1976). 36(12):E798–802. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21289574
Chen YC, Zhang L, Li EN, Ding LX, Zhang GA, Hou Y et al (2019) Late deep cervical infection after anterior cervical discectomy and fusion: a case report and literature review. BMC Musculoskelet Disord 20(1):437. https://doi.org/10.1186/s12891-019-2783-x
Cheng CW, Cizik AM, Dagal AHC, Lewis L, Lynch J, Bellabarba C et al (2019) Body mass index and the risk of deep surgical site infection following posterior cervical instrumented fusion. Spine J 19(4):602–609
Sebastian A, Huddleston P, Kakar S, Habermann E, Wagie A, Nassr A (2016) Risk factors for surgical site infection after posterior cervical spine surgery: an analysis of 5,441 patients from the ACS NSQIP 2005–2012. Spine J 16(4):504–509
Fehlings MG, Smith JS, Kopjar B, Arnold PM, Yoon ST, Vaccaro AR et al (2011) Perioperative and delayed complications associated with the surgical treatment of cervical spondylotic myelopathy based on 302 patients from the AOSpine North America Cervical Spondylotic Myelopathy Study: Presented at the 2011 Spine Section Meeting - Clinical article. J Neurosurg Spine 16(5):425–432
Bhise SD, Mathesul AA, Deokate P, Chandanwale AS, Bartakke GD. (2015) Late prevertebral abscess with sinus following anterior cervical corpectomy and fusion. Asian J Neurosurg 10(3):272–6. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26396628
Daniels AH, Riew KD, Yoo JU, Ching A, Birchard KR, Kranenburg AJ, et al. (2008) Adverse events associated with anterior cervical spine surgery. J Am Acad Orthop Surg 16(12):729–38. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19056921
Haddad S, Millhouse PW, Maltenfort M, Restrepo C, Kepler CK, Vaccaro AR (2016) Diagnosis and neurologic status as predictors of surgical site infection in primary cervical spinal surgery. Spine J 16(5):632–642
Shamji MF, Cook C, Tackett S, Brown C, Isaacs RE (2008) Impact of preoperative neurological status on perioperative morbidity associated with anterior and posterior cervical fusion. J Neurosurg Spine 9(1):10–16
Boakye M, Patil CG, Santarelli J, Ho C, Tian W, Lad SP (2008) Cervical spondylotic myelopathy: complications and outcomes after spinal fusion. Neurosurgery 62(2):455–461
Harris OA, Runnels JB, Matz PG (2001) Clinical factors associated with unexpected critical care management and prolonged hospitalization after elective cervical spine surgery. Crit Care Med 29(10):1898–1902
Jalai CM, Worley N, Poorman GW, Cruz DL, Vira S, Passias PG (2016) Surgical site infections following operative management of cervical spondylotic myelopathy: prevalence, predictors of occurence, and influence on peri-operative outcomes. Eur Spine J 25(6):1891–1896. https://doi.org/10.1007/s00586-016-4501-9
Lonjon G, Dauzac C, Fourniols E, Guigui P, Bonnomet F, Bonnevialle P (2012) Early surgical site infections in adult spinal trauma: a prospective, multicentre study of infection rates and risk factors. Orthop Traumatol Surg Res 98(7):788–794
Pull Ter Gunne AF, Cohen DB. (2009) Incidence, prevalence, and analysis of risk factors for surgical site infection following adult spinal surgery. Spine (Phila Pa 1976). 34(13):1422–8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19478664
Rechtine GR, Bono PL, Cahill D, Bolesta MJ, Chrin AM (2001) Postoperative wound infection after instrumentation of thoracic and lumbar fractures. J Orthop Trauma 15(8):566–569
Thornton FJ, Schäffer MR, Barbul A (1997) Wound healing in sepsis and trauma. Shock 8(6):391–401
Pories SE, Gamelli RL, Mead PB, Goodwin G, Harris F, Vacek P (1991) The epidemiologic features of nosocomial infections in patients with trauma. Arch Surg 126(1):97–99
Papavero L, Lepori P, Schmeiser G (2020) Revision surgery in cervical spine. Eur Spine J 29(1):47–56
Bible JE, Rihn JA, Lim MR, Brodke DS, Lee JY. (2015) Avoiding and Managing Intraoperative Complications during Cervical Spine Surgery. In: Journal of the American Academy of Orthopaedic Surgeons. p. e81–90. Available from: http://content.wkhealth.com/linkback/openurl?sid=WKPTLP:landingpage&an=00124635-201512000-00014
Yoshihara H, Yoneoka D (2014) Understanding the statistics and limitations of large database analyses. Spine (Phila Pa 1976) 39(16):1311–1312
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical approval
Ethical approval was obtained from our institutional review board (132–2019).
Informed consent
All patients signed an informed consent before the surgical intervention.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alhashash, M., Alkharsawi, M. & Shousha, M. Incidence and local risk factors of infection after anterior sub-axial cervical spine surgery: retrospective database analysis of 4897 consecutive procedures. Arch Orthop Trauma Surg 143, 717–727 (2023). https://doi.org/10.1007/s00402-021-04133-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04133-2