Abstract
Introduction
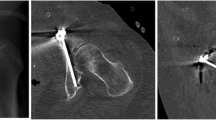
The supraacetabular (SA) corridor extends from the anterior inferior iliac spine to the posterior ilium and can safely accommodate implants to stabilize pelvic and acetabular fractures. However, quantitative analysis of its dimensions and characteristics have not been thoroughly described. This study seeks to define the dimensions, common constriction points, and any alternative trajectories that would maximize the corridor diameter.
Methods
Computed tomography of 100 male and 100 female hemipelves without osseous trauma were evaluated. The corridor boundaries were determined through manual best-fit analysis. The largest intercortical cylinder within the pathway was created and measured. Alternative trajectories were tested within the SA boundaries to identify another orientation that maximized the diameter of the intercortical cylinder.
Results
The traditional SA corridor had a mean diameter of 8.3 mm in men and 6.2 mm in women. This difference in diameter is due to a more S-shaped ilium in women. A larger alternative SA corridor was found that had a less limited path through the ilium and measured 11.3 mm in men and 9.9 mm in women. These dimensions are significantly different compared to those of the traditional SA corridor in both men and women.
Conclusions
In men, the SA corridor allows for the safe passage of most hardware used in pelvic and acetabular fractures. However, in women, the SA corridor is restricted by a more S-shaped ilium. An alternative trajectory was found that has a significantly larger mean diameter in both sexes. Ultimately, the trajectory of hardware will be dictated by the clinical scenario. When large implants are needed, especially in women, we recommend considering the alternative SA corridor.






Similar content being viewed by others
References
Haidukewych GJ, Kumar S, Prpa B (2003) Placement of half-pins for supra-acetabular external fixation: an anatomic study. Clin Orthop Relat Res. 411:269–273
Jung GH, Lee Y, Kim JW (2017) Computational analysis of the safe zone for the antegrade lag screw in posterior column fixation with the anterior approach in acetabular fracture: a cadaveric study. Injury 48:608–614
Mears DC, Fu FH (1980) Modern concepts of external skeletal fixation of the pelvis. Clin Orthop Relat Res. https://doi.org/10.1097/00003086-198009000-00010
Routt ML, Simonian PT, Mills WJ (1997) Iliosacral screw fixation: early complications of the percutaneous technique. J Orthop Trauma 11:584–589
Routt ML, Nork SE, Mills WJ (2000) Percutaneous fixation of pelvic ring disruptions. Clin Orthop Relat Res 375:15–29
Starr AJ, Jones AL, Reinert CM, Borer DS (2001) Preliminary results and complications following limited open reduction and percutaneous screw fixation of displaced fractures of the acetabulum. Injury 32(Suppl 1):SA45–SA50
Scherer J, Guy P, Lefaivre KA, Pape HC, Werner CML, Osterhoff G (2017) Guide wire insertion for percutaneous LC2 screws in acetabular and pelvic ring fixation using a transpedicular working cannula. Injury 48:2360–2364
Starr AJ, Walter JC, Harris RW, Reinert CM, Jones AL (2002) Percutaneous screw fixation of fractures of the iliac wing and fracture–dislocations of the sacro-iliac joint (OTA Types 61–B2.2 and 61–B2.3, or Young-Burgess “lateral compression type II” pelvic fractures). J Orthop Trauma 16:116–123
Gardner MJ, Nork SE (2007) Stabilization of unstable pelvic fractures with supraacetabular compression external fixation. J Orthop Trauma 21:269–273
Kellam JF, Meinberg EG, Agel J, Karam MD, Roberts CS (2018) Introduction: fracture and dislocation classification compendium-2018: international comprehensive classification of fractures and dislocations committee. J Orthop Trauma 32(Suppl 1):S1–S10
Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A (2012) Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma 26:1–8
Sen M, Harvey EJ, Steinitz D, Guy P, Reindl R (2005) Anatomical risks of using supra-acetabular screws in percutaneous internal fixation of the acetabulum and pelvis. Am J Orthop (Belle Mead NJ) 34:94–96
Gras F, Gottschling H, Schröder M, Marintschev I, Reimers N, Burgkart R (2015) Sex-specific differences of the infraacetabular corridor: a biomorphometric CT-based analysis on a database of 523 pelves. Clin Orthop Relat Res 473:361–369
Gras F, Gottschling H, Schröder M, Marintschev I, Hofmann GO, Burgkart R (2016) Transsacral osseous corridor anatomy is more amenable to screw insertion in males: a biomorphometric analysis of 280 pelves. Clin Orthop Relat Res 474:2304–2311
Kaiser SP, Gardner MJ, Liu J, Routt ML, Morshed S (2014) Anatomic determinants of sacral dysmorphism and implications for safe iliosacral screw placement. J Bone Joint Surg Am 96:e120
Wang, Miqi (2021) Supraacetabular corridor data. Mendeley Data v1. https://doi.org/10.17632/66xspychhw.2
Gardner MJ, Morshed S, Nork SE, Ricci WM, Chip Routt ML (2010) Quantification of the upper and second sacral segment safe zones in normal and dysmorphic sacra. J Orthop Trauma 24:622–629
Hasenboehler EA, Stahel PF, Williams A, Smith WR, Newman JT, Symonds DL et al (2011) Prevalence of sacral dysmorphia in a prospective trauma population: Implications for a “safe” surgical corridor for sacro-iliac screw placement. Patient Saf Surg 5:8
Matta JM, Tornetta P (1996) Internal fixation of unstable pelvic ring injuries. Clin Orthop Relat Res 329:129–140
Bishop JA, Routt ML (2012) Osseous fixation pathways in pelvic and acetabular fracture surgery: osteology, radiology, and clinical applications. J Trauma Acute Care Surg 72:1502–1509
Tosounidis TH, Mauffrey C, Giannoudis PV (2018) Optimization of technique for insertion of implants at the supra-acetabular corridor in pelvis and acetabular surgery. Eur J Orthop Surg Traumatol 28:29–35
Chen KN, Wang G, Cao LG, Zhang MC (2009) Differences of percutaneous retrograde screw fixation of anterior column acetabular fractures between male and female: a study of 164 virtual three-dimensional models. Injury 40:1067–1072
Kwan MK, Jeffry A, Chan CY, Saw LB (2012) A radiological evaluation of the morphometry and safety of S1, S2 and S2-ilium screws in the Asian population using three dimensional computed tomography scan: an analysis of 180 pelvis. Surg Radiol Anat 34:217–227
Schildhauer TA, McCulloch P, Chapman JR, Mann FA (2002) Anatomic and radiographic considerations for placement of transiliac screws in lumbopelvic fixations. J Spinal Disord Tech 15:199–205 (discussion)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Miqi Wang is a stockholder in Johnson and Johnson. Robert C. Jacobs declares that he has no conflicts of interest. Craig S. Bartlett has received teaching honoraria from AO Trauma and is a consultant for and stockholder in DePuy-Synthes, SI Bone, Pelvixx, and Summate Technology. Patrick C. Schottel is a paid consultant for Synthes.
Ethical review committee statement
This study was found to be exempt by our institution’s IRB committee. All the work was performed at University of Vermont Medical Center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Wang, M., Jacobs, R.C., Bartlett, C.S. et al. Supraacetabular osseous corridor: defining dimensions, sex differences, and alternatives. Arch Orthop Trauma Surg 142, 1429–1434 (2022). https://doi.org/10.1007/s00402-021-03786-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03786-3