Abstract
Introduction
Although the practice of metaphyseal reconstruction has obtained successful clinical and radiological results in revision total knee surgery, off-the-shelf devices aren’t an effective solution for all patients as they do not cover the full range of clinical possibilities. For this reason, during severe knee revisions, custom-made porous titanium cementless metaphyseal cones are nowadays employed as alternative to traditional surgeries. The aim of this study is to understand the benefits gained by the use of the custom-made cones against the performance of more traditional techniques, such as the use of cemented or cementless stems. Thus, a retrospective study on eleven patients and a biomechanical finite element analysis (FEA) was developed, based upon three clinical cases of the clinical analyzed cohort.
Materials and methods
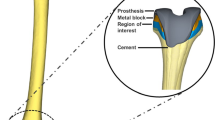
Eleven patients underwent staged total knee arthroplasty revision with the use of 16 custom-made cones to correct severe femoral and tibial meta-diaphyseal bone defects. Clinical scores and range of movement were observed during the follow-up period (mean follow-up 26 ± 9.4 months). Reason for surgery was periprosthetic joint infection (PJI) in eight patients and post-traumatic osteomyelitis in the other three patients. Three patients previously affected by PJI were selected among the eleven patients of the clinical population. For those patients, bone geometries and implants during surgery were replicated in silico and analyzed during different daily activities. For the same patients, as alternative solution for surgery, the use of cemented or cementless stems was also simulated by FEA. Stress patterns in different region of interest and risk of fracture in the bone were calculated and compared.
Results
No loosening, component migration, or mismatches between preoperative planning and intraoperative findings were clinically registered. Biomechanical results demonstrated that the use of custom-made cones induces a more homogeneously distributed bone stress than the other two techniques that concentrate the stress in spotted regions. The risk of fracture is comparable between the use of custom-made cones and cemented technique, while press-fit configurations increase the risk of fracture (more than 35%).
Conclusions
Based upon the clinical evidence and the findings after the FEAs, the practice of porous custom-made metaphyseal cones in severe revisions of knee arthroplasties is showing promising biomechanical results. The homogeneous stresses distributions and the lower bone stress gradient could justify a reduction of bone fractures and the risk of implant loosening which could be the explanation to the successful clinical outcomes.










Similar content being viewed by others
References
Burastero G, Cavagnaro L, Chiarlone F, Innocenti B, Felli L (2018) A case report: custom made porous titanium implants in revision: a new option for complex issues. Open Orthop J. https://doi.org/10.2174/1874325001812010525
American Joint Replacement Registry. Annual Report 2017. https://www.ajrr.net/images/annual_reports/AJRR_2017_Annual_Report_final.pdf
Australian Orthopaedic Association. National Joint Replacement Registry Hip, Knee and Shoulder Arthroplasty Annual Report 2019 https://aoanjrr.sahmri.com/documents/10180/668596/Hip%2C+Knee+%26+Shoulder+Arthroplasty/c287d2a3-22df-a3bb-37a2-91e6c00bfcf0
National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. 16th Annual report 2019 https://reports.njrcentre.org.uk/Portals/0/PDFdownloads/NJR%2016th%20Annual%20Report%202019.pdf
Swedish Knee Arthroplasty Register. Annual Report 2017. https://www.myknee.se/pdf/SVK_2017_Eng_1.0.pdf
Kurtz SM, Lau E, Ong K et al (2009) Future young patient demand for primary and revision joint replacement: National projections from 2010 to 2030. Clin OrthopRelat Res. https://doi.org/10.1007/s11999-009-0834-6
Kurtz S, Ong K, Lau E, Mowat F, Halpern M (2007) Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone JtSurg Am. https://doi.org/10.2106/JBJS.F.00222
Mortazavi SM, Molligan J, Austin MS et al (2011) Failure following revision total knee arthroplasty: infection is the major cause. Int Orthop. https://doi.org/10.1007/s00264-010-1134-1
Kasahara Y, Majima T, Kimura S, Nishiike O, Uchida J (2013) What are the causes of revision total knee arthroplasty in Japan? Clin OrthopRelat Res. https://doi.org/10.1007/s11999-013-2820-2
Engh GA, Ammeen DJ (1999) Bone loss with revision total knee arthroplasty: defect classification and alternatives for reconstruction. Instr Course Lect 48:167
Engh GA, Ammeen DJ (1998) Classification and preoperative radiographic evaluation: knee. Orthop Clin N Am. https://doi.org/10.1016/S0030-5898(05)70319-9
Radnay CS, Scuderi GR (2006) Management of bone loss: augments, cones, offset stems. Clin OrthopRelat Res. https://doi.org/10.1097/01.blo.0000214437.57151.41
Innocenti B, Fekete G, Pianigiani S (2018) Biomechanical analysis of augments in revision total knee arthroplasty. J BiomechEng 10(1115/1):4040966
Hockman DE, Ammeen D, Engh GA (2005) Augments and allografts in revision total knee arthroplasty: usage and outcome using one modular revision prosthesis. J Arthroplasty. https://doi.org/10.1016/j.arth.2004.09.059
Panni AS, Vasso M, Cerciello S (2013) Modular augmentation in revision total knee arthroplasty. Knee Surg Sports TraumatolArthrosc. https://doi.org/10.1007/s00167-012-2258-1
Stulberg SD (2003) Bone loss in revision total knee arthroplasty: graft options and adjucts. J Arthroplasty 18(3 Suppl 1):48–50
Toms AD, Barker RL, McClelland D et al (2009) Repair of defects and containment in revision total knee replacement: a comparative biomechanical analysis. J Bone JtSurg Br. https://doi.org/10.1302/0301-620X.91B2.21415
Chalmers BP, Desy NM, Pagnano MW, Trousdale RT, Taunton MJ (2017) Survivorship of metaphyseal sleeves in revision total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2016.12.004
Kim EG, Patel NK, Chughtai M et al (2016) Tantalum cones in revision total knee arthroplasty. J Knee Surg. https://doi.org/10.1055/s-0036-1593370
Calori GM, Colombo M, Ripamonti C et al (2014) Megaprosthesis in large bone defects: opportunity or chimaera? Injury. https://doi.org/10.1016/j.injury.2013.09.015
Zanirato A, Formica M, Cavagnaro L, Divano S, Burastero G, Felli L (2019) Metaphyseal cones and sleeves in revision total knee arthroplasty: two sides of the same coin? Complications, clinical and radiological results—systematic review of the literature. MusculoskeletSurg. https://doi.org/10.1007/s12306-019-00598-y
Divano S, Cavagnaro L, Zanirato A, Basso M, Felli L, Formica M (2018) Porous metal cones: gold standard for massive bone loss in complex revision knee arthroplasty? A systematic review of current literature. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-018-2936-7
Cherny AA, Kovalenko AN, Bilyk SS, Denisov AO, Kazemirskiy AV, Kulyaba TA, Kornilov NN (2019) Early outcomes of patient-specific modular cones for substitution of methaphysial and diaphysial bone defects in revision knee arthroplasty. Travmatologiya i ortopediyaRossii Traumatology and Orthopedics of Russia. https://doi.org/10.21823/2311-2905-2019-25-2-9-18
Ohlmeier M, Lausmann C, Wolff M et al (2020) Preliminary clinical results of coated porous tibia cones in septic and aseptic revision knee arthroplasty. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-020-03434-2
Zanirato A, Cavagnaro L, Basso M, Divano S, Felli L, Formica M (2018) Metaphyseal sleeves in total knee arthroplasty revision: complications, clinical and radiological results. A systematic review of the literature. Arch Orthop Trauma Surg 138(7):993–1001
Cavagnaro L, Burastero G, Chiarlone F, Felli L (2019) A new custom-made porous titanium device in knee revision surgery: early results and technical notes. OrthopProc. https://doi.org/10.1302/1358-992x.2019.4.009
Pianigiani S, Innocenti B (2015) The use of finite element modeling to improve biomechanical research on knee prosthesis. In: Stewart J (ed) New developments in knee prosthesis research. Nova Science Publishers, Hauppauge, NY, pp 113–126
El-Zayat BF, Heyse TJ, Fanciullacci N, Labey L, Fuchs-Winkelmann S, Innocenti B (2016) Fixation techniques and stem dimensions in hinged total knee arthroplasty: a finite element study. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-016-2571-0
Andreani L, Pianigiani S, Bori E, Lisanti M, Innocenti B (2020) Analysis of biomechanical differences between condylar constrained knee and rotating hinged implants: a numerical study. J Arthroplasty. https://doi.org/10.1016/j.arth.2019.08.005
Innocenti B (2019) High congruency MB insert design: stabilizing knee joint even with PCL deficiency. Knee Surg Sports Traumatol Arthrosc. 28(9):3040–3047. https://doi.org/10.1007/s00167-019-05764-0
Castellarin G, Pianigiani S, Innocenti B (2019a) Asymmetric polyethylene inserts promote favorable kinematics and better clinical outcome compared to symmetric inserts in a mobile bearing total knee arthroplasty. Knee Surg Sports TraumatolArthrosc 27(4):1096–1105
Innocenti B, Bilgen OF, Labe L, van Lenth GH, Slote JV, Catani F (2014) Load sharing and ligament strains in balanced, overstuffed and understuffed UKA. A validated finite element analysis. J Arthroplasty. https://doi.org/10.1016/j.arth.2014.01.020
Innocenti B, Bellemans J, Catani F (2015) Deviations from optimal alignment in TKA: is there a biomechanical difference between femoral or tibial component alignment? J Arthroplasty. https://doi.org/10.1016/j.arth.2015.07.038
Innocenti B, Pianigiani S, Ramundo G, Thienpont E (2016) Biomechanical effects of different varus and valgus alignments in medial unicompartmental knee arthroplasty. J Arthroplasty 31(12):2685–2691
Belvedere C, Leardini A, Catani F, Pianigiani S, Innocenti B (2017) In vivo kinematics of knee replacement during daily living activities: condylar and post-cam contact assessment by three dimensional fluoroscopy and finite element analyses. J Orthop Res. https://doi.org/10.1002/jor.23405
Brihault J, Navacchia A, Pianigiani S, Labey L, De Corte R, Pascale V, Innocenti B (2016) All-polyethylene tibial components generate higher stress and micromotions than metal-backed tibial components in total knee arthroplasty. Knee Surg Sports TraumatolArthrosc. https://doi.org/10.1007/s00167-015-3630-8
Innocenti B, Robledo Yagüe H, AlarioBernabé R, Pianigiani S (2015) Investigation on the effects induced by TKA features on tibio-femoral mechanics part I: femoral component designs. J Mech Med Biol. https://doi.org/10.1142/S0219519415400345
Pianigiani S, AlarioBernabé R, Robledo Yagüe H, Innocenti B (2015) Investigation on the effects induced by TKA features on tibio-femoral mechanics part II: tibial insert designs. J Mech Med Biol. https://doi.org/10.1142/S0219519415400357
Soenen M, Baracchi M, De Corte R, Labey L, Innocenti B (2013) Stemmed TKA in a femur with a total hip arthroplasty: is there a safe distance between the stem tips? J Arthroplasty. https://doi.org/10.1016/j.arth.2013.01.010
Schileo E, Dall’Ara E, Taddei F, Malandrino A, Schotkamp T, Baleani M, Viceconti M (2008) An accurate estimation of bone density improves the accuracy of subject-specific finite element models. J Biomech. https://doi.org/10.1016/j.jbiomech.2008.05.017
Completo A, Talaia P, Fonseca F, Simões JA (2009) Relationship of design features of stemmed tibial knee prosthesis with stress shielding and end-of-stem pain. Mater Des. https://doi.org/10.1016/j.jbiomech.2007.10.006
Burastero G, Cavagnaro L, Chiarlone F, Alessio-Mazzola M, Carrega G, Felli L (2018) The use of tantalum metaphyseal cones for the management of severe bone defects in septic knee revision. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.08.026
Morgan-Jones R, Oussedik SIS, Graichen H, Haddad FS (2015) Zonal fixation in revision total knee arthroplasty. Bone Jt J. https://doi.org/10.1302/0301-620X.97B2.34144
Abraham R, Malkani AL, Lewis J, Beck D (2007) An anatomical study of tibial metaphyseal/diaphyseal mismatch during revision total knee arthroplasty. J Anthroplasty. https://doi.org/10.1016/j.arth.2006.06.001
Acknowledgements
The author would like to thank Mr. Edoardo Bori, Mr. Carlo Dottino and Prof. Lamberto Felli for their precious help during the writing of the study.
Funding
This work was supported by FNRS (Fonds National de la Recherche Scientifique, CDR 19545501 and CDR 29155446) and by FER ULB (Fonds d'Encouragement a la Recherche, FER 2017). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Giorgio Burastero has received research grants and has royalties from Adler Ortho (Milano, Italy). Silvia Pianigiani is a paid employee of Adler Ortho (Milano, Italy). Bernardo Innocenti has received research grants and speaker honorarium from Adler Ortho (Milano, Italy). Cristiana Zanvettor, Luca Cavagnaro and Francesco Chiarlone declare that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Burastero, G., Pianigiani, S., Zanvettor, C. et al. Use of porous custom-made cones for meta-diaphyseal bone defects reconstruction in knee revision surgery: a clinical and biomechanical analysis. Arch Orthop Trauma Surg 140, 2041–2055 (2020). https://doi.org/10.1007/s00402-020-03670-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-020-03670-6