Abstract
Introduction
Focal cartilage defects are an increasingly relevant clinical problem especially in athletes. Cartilage regenerative surgery (CRS) including microfracture and autologous chondrocyte implantation (ACI) to treat such isolated cartilage defects in the knee joint has been well established in the last two decades. In contradiction to high-level evidence concerning the surgical technique, cell-related issues, and clinical results, the knowledge about the optimal rehabilitation process is still sparse although the importance of optimizing the rehabilitation process has recently led to new research focus in this field. The preoperative time frame may be used to start rehabilitation which may fasten the postoperative recovery and optimize clinical outcome (“Prehabilitation”—PREHAB). The aim of this article, therefore, was to review the available literature on prehabilitation concepts and to present a prehabilitation guideline for CRS patients based on the best evidence available.
Methods
A systemic literature research was conducted on rehabilitation for cartilage regenerative surgery as well as prehabilitation in knee joint procedures. From the available literature a prehabilitation concept was generated and tested in 10 ACI patients.
Results
As the literature search found no studies addressing prehabilitation in CRS patients, an evidence-based PREHAB program has been compiled based on the available evidence from (a) studies addressing postoperative rehabilitation in CRS patients and (b) PREHAB studies on other knee procedures including TKA. This presented prehabilitation guideline has been tested in > 50 CRS patients and was found to be feasible as all of the patients showed a good compliance and were able to perform the protocol as suggested.
Conclusion
The presented PREHAB regimen may serve clinicians as a guideline for early rehabilitation of their CRS patients. Obviously, further research is mandatory to quantify its clinical effect and to demonstrate its cost-effectiveness and benefits in surgically treated patients.
Similar content being viewed by others
References
Campbell AB, Pineda M, Harris JD, Flanigan DC (2016) Return to sport after articular cartilage repair in athletes’ knees: a systematic review. Arthroscopy 32(4):651–668 e651. https://doi.org/10.1016/j.arthro.2015.08.028
Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH (2010) Prevalence of chondral defects in athletes’ knees: a systematic review. Med Sci Sports Exerc 42(10):1795–1801. https://doi.org/10.1249/MSS.0b013e3181d9eea0
Niemeyer P, Lenz P, Kreuz PC, Salzmann GM, Suedkamp NP, Schmal H, Steinwachs M (2010) Chondrocyte—seeded collagen type I/III membrane (ACT-CS) for autologous chondrocyte transplantation: Prospective 2-year results in patients with cartilage defects of the knee joint. Arthroscopy (in print)
Peterson L, Brittberg M, Kiviranta I, Akerlund EL, Lindahl A (2002) Autologous chondrocyte transplantation. Biomechanics and long-term durability. Am J Sports Med 30(1):2–12
Peterson L, Vasiliadis HS, Brittberg M, Lindahl A (2010) Autologous chondrocyte implantation: a long-term follow-up. Am J Sports Med 38(6):1117–1124. https://doi.org/10.1177/0363546509357915
Saris DB, Vanlauwe J, Victor J, Almqvist KF, Verdonk R, Bellemans J, Luyten FP (2009) Treatment of symptomatic cartilage defects of the knee: characterized chondrocyte implantation results in better clinical outcome at 36 months in a randomized trial compared to microfracture. Am J Sports Med 37(Suppl 1):10S–19S. https://doi.org/10.1177/0363546509350694
DiBartola AC, Wright BM, Magnussen RA, Flanigan DC (2016) Clinical outcomes after autologous chondrocyte implantation in adolescents’ knees: a systematic review. Arthroscopy. https://doi.org/10.1016/j.arthro.2016.03.007
Krishnan SP, Skinner JA, Bartlett W, Carrington RW, Flanagan AM, Briggs TW, Bentley G (2006) Who is the ideal candidate for autologous chondrocyte implantation? J Bone Jt Surg Br 88(1):61–64. https://doi.org/10.1302/0301-620X.88B1.16796
Mithofer K, Minas T, Peterson L, Yeon H, Micheli LJ (2005) Functional outcome of knee articular cartilage repair in adolescent athletes. Am J Sports Med 33(8):1147–1153. https://doi.org/10.1177/0363546504274146
Hambly K, Bobic V, Wondrasch B, Van Assche D, Marlovits S (2006) Autologous chondrocyte implantation postoperative care and rehabilitation: science and practice. Am J Sports Med 34(6):1020–1038. https://doi.org/10.1177/0363546505281918
Ebert JR, Ackland TR, Lloyd DG, Wood DJ (2008) Accuracy of partial weight bearing after autologous chondrocyte implantation. Arch Phys Med Rehabil 89(8):1528–1534. https://doi.org/10.1016/j.apmr.2008.02.019
Della Villa S, Kon E, Filardo G, Ricci M, Vincentelli F, Delcogliano M, Marcacci M (2010) Does intensive rehabilitation permit early return to sport without compromising the clinical outcome after arthroscopic autologous chondrocyte implantation in highly competitive athletes? Am J Sports Med 38(1):68–77. https://doi.org/10.1177/0363546509348490
Wondrasch B, Aroen A, Rotterud JH, Hoysveen T, Bolstad K, Risberg MA (2013) The feasibility of a 3-month active rehabilitation program for patients with knee full-thickness articular cartilage lesions: the Oslo Cartilage Active Rehabilitation and Education Study. J Orthop Sports Phys Ther 43(5):310–324. https://doi.org/10.2519/jospt.2013.4354
Ebert JR, Lloyd DG, Wood DJ, Ackland TR (2012) Isokinetic knee extensor strength deficit following matrix-induced autologous chondrocyte implantation. Clin Biomech 27(6):588–594. https://doi.org/10.1016/j.clinbiomech.2012.01.006
Loken S, Ludvigsen TC, Hoysveen T, Holm I, Engebretsen L, Reinholt FP (2009) Autologous chondrocyte implantation to repair knee cartilage injury: ultrastructural evaluation at 2 years and long-term follow-up including muscle strength measurements. Knee Surg Sports Traumatol Arthrosc 17(11):1278–1288. https://doi.org/10.1007/s00167-009-0854-5
Kreuz PC, Muller S, Erggelet C, von Keudell A, Tischer T, Kaps C, Niemeyer P, Hirschmuller A (2014) Is gender influencing the biomechanical results after autologous chondrocyte implantation? Knee Surg Sports Traumatol Arthrosc 22(1):72–79. https://doi.org/10.1007/s00167-012-2280-3
Kreuz PC, Muller S, Freymann U, Erggelet C, Niemeyer P, Kaps C, Hirschmuller A (2011) Repair of focal cartilage defects with scaffold-assisted autologous chondrocyte grafts: clinical and biomechanical results 48 months after transplantation. Am J Sports Med 39(8):1697–1705. https://doi.org/10.1177/0363546511403279
Kreuz PC, Steinwachs M, Erggelet C, Lahm A, Krause S, Ossendorf C, Meier D, Ghanem N, Uhl M (2007) Importance of sports in cartilage regeneration after autologous chondrocyte implantation: a prospective study with a 3-year follow-up. Am J Sports Med 35(8):1261–1268. https://doi.org/10.1177/0363546507300693
Slemenda C, Brandt KD, Heilman DK, Mazzuca S, Braunstein EM, Katz BP, Wolinsky FD (1997) Quadriceps weakness and osteoarthritis of the knee. Ann Intern Med 127(2):97–104
Slemenda C, Heilman DK, Brandt KD, Katz BP, Mazzuca SA, Braunstein EM, Byrd D (1998) Reduced quadriceps strength relative to body weight: a risk factor for knee osteoarthritis in women? Arthritis Rheum 41 (11):1951–1959. https://doi.org/10.1002/1529-0131(199811)41:11%3C1951::AID-ART9%3E3.0.CO;2-9
Bennell K, Hinman RS, Wrigley TV, Creaby MW, Hodges P (2011) Exercise and osteoarthritis: cause and effects. Compr Physiol 1(4):1943–2008. https://doi.org/10.1002/cphy.c100057
Jackson BD, Wluka AE, Teichtahl AJ, Morris ME, Cicuttini FM (2004) Reviewing knee osteoarthritis—a biomechanical perspective. J Sci Med Sport 7(3):347–357
Jan MH, Lin DH, Lin JJ, Lin CH, Cheng CK, Lin YF (2009) Differences in sonographic characteristics of the vastus medialis obliquus between patients with patellofemoral pain syndrome and healthy adults. Am J Sports Med 37(9):1743–1749. https://doi.org/10.1177/0363546509333483
Bennell KL, Kyriakides M, Metcalf B, Egerton T, Wrigley TV, Hodges PW, Hunt MA, Roos EM, Forbes A, Ageberg E, Hinman RS (2014) Neuromuscular versus quadriceps strengthening exercise in patients with medial knee osteoarthritis and varus malalignment: a randomized controlled trial. Arthritis Rheumatol 66(4):950–959. https://doi.org/10.1002/art.38317
Cashman GE (2012) The effect of weak hip abductors or external rotators on knee valgus kinematics in healthy subjects: a systematic review. J Sport Rehabil 21(3):273–284
Kean CO, Hinman RS, Wrigley TV, Lim BW, Bennell KL (2017) Impact loading following quadriceps strength training in individuals with medial knee osteoarthritis and varus alignment. Clin Biomech 42:20–24. https://doi.org/10.1016/j.clinbiomech.2017.01.002
Kean CO, Bennell KL, Wrigley TV, Hinman RS (2015) Relationship between hip abductor strength and external hip and knee adduction moments in medial knee osteoarthritis. Clin Biomech (Bristol Avon) 30(3):226–230. https://doi.org/10.1016/j.clinbiomech.2015.01.008
Cronin B, Johnson ST, Chang E, Pollard CD, Norcross MF (2016) Greater Hip extension but not hip abduction explosive strength is associated with lesser hip adduction and knee valgus motion during a single-leg jump-cut. Orthop J Sports Med 4(4):2325967116639578. https://doi.org/10.1177/2325967116639578
Costa RA, Oliveira LM, Watanabe SH, Jones A, Natour J (2010) Isokinetic assessment of the hip muscles in patients with osteoarthritis of the knee. Clinics 65(12):1253–1259
van Gool CH, Penninx BW, Kempen GI, Rejeski WJ, Miller GD, van Eijk JT, Pahor M, Messier SP (2005) Effects of exercise adherence on physical function among overweight older adults with knee osteoarthritis. Arthritis Rheum 53(1):24–32. https://doi.org/10.1002/art.20902
Mazieres B, Thevenon A, Coudeyre E, Chevalier X, Revel M, Rannou F (2008) Adherence to, and results of, physical therapy programs in patients with hip or knee osteoarthritis. Development of French clinical practice guidelines. Jt Bone Spine 75(5):589–596. https://doi.org/10.1016/j.jbspin.2008.02.016
Ibrahim MS, Khan MA, Nizam I, Haddad FS (2013) Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: an evidence-based review. BMC Med 11:37. https://doi.org/10.1186/1741-7015-11-37
Santa Mina D, Clarke H, Ritvo P, Leung YW, Matthew AG, Katz J, Trachtenberg J, Alibhai SM (2014) Effect of total-body prehabilitation on postoperative outcomes: a systematic review and meta-analysis. Physiotherapy 100(3):196–207. https://doi.org/10.1016/j.physio.2013.08.008
Jaggers JR, Simpson CD, Frost KL, Quesada PM, Topp RV, Swank AM, Nyland JA (2007) Prehabilitation before knee arthroplasty increases postsurgical function: a case study. J Strength Condition Res Natl Strength Condition Assoc 21(2):632–634. https://doi.org/10.1519/R-19465.1
Topp R, Swank AM, Quesada PM, Nyland J, Malkani A (2009) The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. J Injury Funct Rehabil 1(8):729–735. https://doi.org/10.1016/j.pmrj.2009.06.003
Santa Mina D, Scheede-Bergdahl C, Gillis C, Carli F (2015) Optimization of surgical outcomes with prehabilitation. Appl Physiol Nutr Metab 40 (9):966–969. https://doi.org/10.1139/apnm-2015-0084
Ackerman IN, Bennell KL (2004) Does pre-operative physiotherapy improve outcomes from lower limb joint replacement surgery? A systematic review. Aust J Physiother 50(1):25–30
Gill SD, McBurney H (2013) Does exercise reduce pain and improve physical function before hip or knee replacement surgery? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil 94(1):164–176. https://doi.org/10.1016/j.apmr.2012.08.211
Fransen M, McConnell S, Harmer AR, Van der Esch M, Simic M, Bennell KL (2015) Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med 49(24):1554–1557. https://doi.org/10.1136/bjsports-2015-095424
McKay C, Prapavessis H, Doherty T (2012) The effect of a prehabilitation exercise program on quadriceps strength for patients undergoing total knee arthroplasty: a randomized controlled pilot study. J Injury Funct Rehabil 4(9):647–656. https://doi.org/10.1016/j.pmrj.2012.04.012
Kean CO, Birmingham TB, Garland SJ, Bryant DM, Giffin JR (2011) Preoperative strength training for patients undergoing high tibial osteotomy: a prospective cohort study with historical controls. J Orthop Sports Phys Ther 41(2):52–59. https://doi.org/10.2519/jospt.2011.3490
Heir S, Nerhus TK, Rotterud JH, Loken S, Ekeland A, Engebretsen L, Aroen A (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38(2):231–237. https://doi.org/10.1177/0363546509352157
Felson DT, Gross KD, Nevitt MC, Yang M, Lane NE, Torner JC, Lewis CE, Hurley MV (2009) The effects of impaired joint position sense on the development and progression of pain and structural damage in knee osteoarthritis. Arthritis Rheum 61(8):1070–1076. https://doi.org/10.1002/art.24606
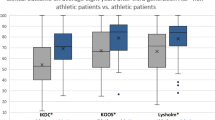
Hirschmuller A, Andres T, Schoch W, Baur H, Konstantinidis L, Sudkamp NP, Niemeyer P (2017) Quadriceps strength in patients with isolated cartilage defects of the knee: results of isokinetic strength measurements and their correlation with clinical and functional results. Orthop J Sports Med 5(5):2325967117703726. https://doi.org/10.1177/2325967117703726
Aagaard P (2003) Training-induced changes in neural function. Exerc Sport Sci Rev 31(2):61–67
Aagaard P, Andersen JL, Dyhre-Poulsen P, Leffers AM, Wagner A, Magnusson SP, Halkjaer-Kristensen J, Simonsen EB (2001) A mechanism for increased contractile strength of human pennate muscle in response to strength training: changes in muscle architecture. J Physiol 534(Pt. 2):613–623
American College of Sports Medicine Position Stand (2009) Progression models in resistance training for healthy adults. Med Sci Sports Exerc 41(3):687–708. https://doi.org/10.1249/MSS.0b013e3181915670
Ronnestad BR, Hansen J, Hollan I, Ellefsen S (2015) Strength training improves performance and pedaling characteristics in elite cyclists. Scand J Med Sci Sports 25(1):e89–e98. https://doi.org/10.1111/sms.12257
Daehlin TE, Haugen OC, Haugerud S, Hollan I, Raastad T, Ronnestad BR (2016) Combined plyometric and strength training improves Ice-Hockey players’ on-ice sprint. Int J Sports Physiol Perform. https://doi.org/10.1123/ijspp.2016-0262
Gruber M, Bruhn S, Gollhofer A (2006) Specific adaptations of neuromuscular control and knee joint stiffness following sensorimotor training. Int J Sports Med 27(8):636–641
Bruhn S, Kullmann N, Gollhofer A (2006) Combinatory effects of high-intensity-strength training and sensorimotor training on muscle strength. Int J Sports Med 27(5):401–406
Bruhn S, Kullmann N, Gollhofer A (2004) The effects of a sensorimotor training and a strength training on postural stabilisation, maximum isometric contraction and jump performance. Int J Sports Med 25(1):56–60
Behm D, Colado JC (2012) The effectiveness of resistance training using unstable surfaces and devices for rehabilitation. Int J Sports Phys Ther 7(2):226–241
Hirschmuller A, Baur H, Braun S, Kreuz PC, Sudkamp NP, Niemeyer P (2011) Rehabilitation after autologous chondrocyte implantation for isolated cartilage defects of the knee. Am J Sports Med 39(12):2686–2696. https://doi.org/10.1177/0363546511404204
Escamilla RF (2001) Knee biomechanics of the dynamic squat exercise. Med Sci Sports Exerc 33:127–141
Andersen LL, Magnusson SP, Nielsen M, Haleem J, Poulsen K, Aagaard P (2006) Neuromuscular activation in conventional therapeutic exercises and heavy resistance exercises: implications for rehabilitation. Phys Ther 86(5):683–697
Rutherford OM, Jones DA (1986) The role of learning and coordination in strength training. Eur J Appl Physiol Occup Physiol 55(1):100–105
Pollock ML, Gaesser GA, Butcher JD, Desprs J-P, Dishman RK, Franklin BA, Garber CE (1998) ACSM position stand: the recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sports Exerc 30(6):975–991
Ronnestad BR, Hansen J, Hollan I, Spencer M, Ellefsen S (2016) Impairment of Performance variables after in-season strength-training cessation in elite cyclists. Int J Sports Physiol Perform 11(6):727–735. https://doi.org/10.1123/ijspp.2015-0372
Wilkerson GB, Giles JL, Seibel DK (2012) Prediction of core and lower extremity strains and sprains in collegiate football players: a preliminary study. J Athl Train 47(3):264–272. https://doi.org/10.4085/1062-6050-47.3.17
Shi DL, Li JL, Zhai H, Wang HF, Meng H, Wang YB (2012) Specialized core stability exercise: a neglected component of anterior cruciate ligament rehabilitation programs. J Back Musculoskelet Rehabil 25(4):291–297. https://doi.org/10.3233/BMR-2012-0345
Leetun DT, Ireland ML, Willson JD, Ballantyne BT, Davis IM (2004) Core stability measures as risk factors for lower extremity injury in athletes. Med Sci Sports Exerc 36(6):926–934
Willson JD, Dougherty CP, Ireland ML, Davis IM (2005) Core stability and its relationship to lower extremity function and injury. J Am Acad Orthop Surg 13(5):316–325
Eckstein F, Hudelmaier M, Putz R (2006) The effects of exercise on human articular cartilage. J Anat 208(4):491–512. https://doi.org/10.1111/j.1469-7580.2006.00546.x
Eckstein F, Lemberger B, Gratzke C, Hudelmaier M, Glaser C, Englmeier KH, Reiser M (2005) In vivo cartilage deformation after different types of activity and its dependence on physical training status. Ann Rheum Dis 64(2):291–295. https://doi.org/10.1136/ard.2004.022400
Myer GD, Ford KR, McLean SG, Hewett TE (2006) The effects of plyometric versus dynamic stabilization and balance training on lower extremity biomechanics. Am J Sports Med 34(3):445–455. https://doi.org/10.1177/0363546505281241
Nagano Y, Ida H, Akai M, Fukubayashi T (2011) Effects of jump and balance training on knee kinematics and electromyography of female basketball athletes during a single limb drop landing: pre-post intervention study. Sports Med Arthrosc Rehabil Ther Technol 3(1):14. https://doi.org/10.1186/1758-2555-3-14
Steffen K, Emery CA, Romiti M, Kang J, Bizzini M, Dvorak J, Finch CF, Meeuwisse WH (2013) High adherence to a neuromuscular injury prevention programme (FIFA 11+) improves functional balance and reduces injury risk in Canadian youth female football players: a cluster randomised trial. Br J Sports Med 47(12):794–802. https://doi.org/10.1136/bjsports-2012-091886
Barengo NC, Meneses-Echavez JF, Ramirez-Velez R, Cohen DD, Tovar G, Bautista JE (2014) The impact of the FIFA 11 + training program on injury prevention in football players: a systematic review. Int J Environ Res Public Health 11(11):11986–12000. https://doi.org/10.3390/ijerph111111986
Pisters MF, Veenhof C, Schellevis FG, Twisk JW, Dekker J, De Bakker DH (2010) Exercise adherence improving long-term patient outcome in patients with osteoarthritis of the hip and/or knee. Arthritis Care Res 62(8):1087–1094. https://doi.org/10.1002/acr.20182
Ardern CL, Taylor NF, Feller JA, Whitehead TS, Webster KE (2013) Psychological responses matter in returning to preinjury level of sport after anterior cruciate ligament reconstruction surgery. Am J Sports Med 41(7):1549–1558. https://doi.org/10.1177/0363546513489284
Acknowledgements
The authors are grateful to the two professional translators Carole Cürten and Duncan Cummins for language support as well as to the medical students Tanja Papke and Tasja Andrees for their support in improving the program and collegiality.
Funding
There is no funding source.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Hirschmüller, A., Schoch, W., Baur, H. et al. Rehabilitation before regenerative cartilage knee surgery: a new prehabilitation guideline based on the best available evidence. Arch Orthop Trauma Surg 139, 217–230 (2019). https://doi.org/10.1007/s00402-018-3026-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-018-3026-6