Abstract
Purpose
The associations between dietary patterns and liver cancer risk have received much attention, but evidence among the Chinese population is scarce. This study aims to update the results of two cohort studies and provide the sex-specific associations in the Chinese population.
Methods
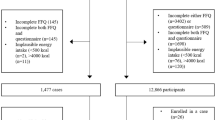
This study was based on two cohorts from the Shanghai Men’s Health Study (SMHS) and the Shanghai Women’s Health Study (SWHS). Diet information was collected by validated food frequency questionnaires. Dietary patterns were derived by factor analysis. Cox regression model was utilized to estimate the hazard ratio (HR) and 95% confidence interval (CI) for associations between dietary patterns and liver cancer risk.
Results
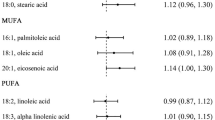
During median follow-up years of 11.2 (male) and 17.1 (female) years, 427 males and 252 females were identified as incident primary liver cancer cases. In males, vegetable-based dietary pattern was inversely associated with liver cancer (HRQ4-Q1: 0.67, 95%CI 0.51–0.88, Ptrend < 0.001). Interaction analysis indicated that in males lower vegetable-based dietary pattern score and older age/medical history of chronic hepatitis combined increase the hazard of liver cancer more than the sum of them, with a 114% and 1061% higher risk, respectively. In females, the fruit-based dietary pattern was associated with a reduced risk of liver cancer (HRQ4-Q1: 0.63, 95%CI 0.42–0.95, Ptrend = 0.03). In both males and females, null associations were observed between the meat-based dietary pattern and the risk of liver cancer.
Conclusion
A vegetable-based dietary pattern in males and a fruit-based dietary pattern in females tended to have a protective role on liver cancer risk. This study provided updated information that might be applied to guide public health action for the primary prevention of liver cancer.

Similar content being viewed by others
Availability of data and materials
Data will be available upon request pending application and approval by the scientific committee of the relevant institutes.
Abbreviations
- AP:
-
Attributable proportion due to interaction
- BMI:
-
Body mass index
- CI:
-
Confidence interval
- EPIC:
-
European Prospective Investigation into Cancer and Nutrition
- FFQ:
-
Food frequency questionnaires
- HBV:
-
Hepatitis B virus
- HCV:
-
Hepatitis C virus
- HR:
-
Hazard ratio
- PAQ:
-
Physical activity questionnaires
- RERI:
-
Relative excess risk due to interaction
- SI:
-
Synergy index
- SMHS:
-
Shanghai Men’s Health Study
- SWHS:
-
Shanghai Women’s Health Study
- WCRF/AICR:
-
World Cancer Research Fund/ American Institute for Cancer Research
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin 71(3):209–249. https://doi.org/10.3322/caac.21660
World Cancer Research Fund/American Institute for Cancer Research (2018) Diet, nutrition, physical activity and cancer: a global perspective. https://www.aicr.org/research/third-expert-report.
Ma Y, Yang W, Simon TG, Smith-Warner SA, Fung TT, Sui J, Chong D, VoPham T, Meyerhardt JA, Wen D, Giovannucci EL, Chan AT, Zhang X (2019) Dietary patterns and risk of hepatocellular carcinoma among U. S. men and women. Hepatology 70(2):577–586. https://doi.org/10.1002/hep.30362
Bogumil D, Park SY, Le Marchand L, Haiman CA, Wilkens LR, Boushey CJ, Setiawan VW (2019) High-quality diets are associated with reduced risk of hepatocellular carcinoma and chronic liver disease: the multiethnic cohort. Hepatol Commun 3(3):437–447. https://doi.org/10.1002/hep4.1313
Turati F, Trichopoulos D, Polesel J, Bravi F, Rossi M, Talamini R, Franceschi S, Montella M, Trichopoulou A, La Vecchia C, Lagiou P (2014) Mediterranean diet and hepatocellular carcinoma. J Hepatol 60(3):606–611. https://doi.org/10.1016/j.jhep.2013.10.034
Li WQ, Park Y, McGlynn KA, Hollenbeck AR, Taylor PR, Goldstein AM, Freedman ND (2014) Index-based dietary patterns and risk of incident hepatocellular carcinoma and mortality from chronic liver disease in a prospective study. Hepatology 60(2):588–597. https://doi.org/10.1002/hep.27160
Chen PY, Fang AP, Wang XY, Lan QY, Liao GC, Liu ZY, Zhang DM, Zhang YY, Chen YM, Zhu HL (2018) Adherence to the Chinese or American dietary guidelines is associated with a lower risk of primary liver cancer in China: a case-control study. Nutrients 10(8):1113. https://doi.org/10.3390/nu10081113
Lan QY, Liao GC, Zhou RF, Chen PY, Wang XY, Chen MS, Chen YM, Zhu HL (2018) Dietary patterns and primary liver cancer in Chinese adults: a case-control study. Oncotarget 9(45):27872–27881. https://doi.org/10.18632/oncotarget.23910
Moussa I, Day RS, Li R, Du XL, Kaseb AO, Jalal PK, Daniel-MacDougall C, Hatia RI, Abdelhakeem A, Rashid A, Chun YS, Li D, Hassan MM (2021) Dietary patterns and hepatocellular carcinoma risk among us adults. Nutrients 13(6):2011. https://doi.org/10.3390/nu13062011
Zhang W, Xiang YB, Li HL, Yang G, Cai H, Ji BT, Gao YT, Zheng W, Shu XO (2013) Vegetable-based dietary pattern and liver cancer risk: results from the Shanghai women’s and men’s health studies. Cancer Sci 104(10):1353–1361. https://doi.org/10.1111/cas.12231
Guo W, Ge X, Lu J, Xu X, Gao J, Wang Q, Song C, Zhang Q, Yu C (2022) Diet and risk of non-alcoholic fatty liver disease, cirrhosis, and liver cancer: a large prospective cohort study in UK Biobank. Nutrients 14(24):5335. https://doi.org/10.3390/nu14245335
Shu XO, Li H, Yang G, Gao J, Cai H, Takata Y, Zheng W, Xiang YB (2015) Cohort profile: The Shanghai Men’s health study. Int J Epidemiol 44(3):810–818. https://doi.org/10.1093/ije/dyv013
Zheng W, Chow WH, Yang G, Jin F, Rothman N, Blair A, Li HL, Wen W, Ji BT, Li Q, Shu XO, Gao YT (2005) The Shanghai Women’s Health Study: rationale, study design, and baseline characteristics. Am J Epidemiol 162(11):1123–1131. https://doi.org/10.1093/aje/kwi322
Shu XO, Yang G, Jin F, Liu D, Kushi L, Wen W, Gao YT, Zheng W (2004) Validity and reproducibility of the food frequency questionnaire used in the Shanghai Women’s Health Study. Eur J Clin Nutr 58(1):17–23. https://doi.org/10.1038/sj.ejcn.1601738
Villegas R, Yang G, Liu D, Xiang YB, Cai H, Zheng W, Shu XO (2007) Validity and reproducibility of the food-frequency questionnaire used in the Shanghai Men’s Health Study. Br J Nutr 97(5):993–1000. https://doi.org/10.1017/s0007114507669189
Wang GY, Shen ZP (1991) Chinese Food Composition Tables. People’s Health Publishing House, Beijin
Jurj AL, Wen W, Xiang YB, Matthews CE, Liu D, Zheng W, Shu XO (2007) Reproducibility and validity of the Shanghai Men’s Health Study physical activity questionnaire. Am J Epidemiol 165(10):1124–1133. https://doi.org/10.1093/aje/kwk119
Matthews CE, Shu XO, Yang G, Jin F, Ainsworth BE, Liu D, Gao YT, Zheng W (2003) Reproducibility and validity of the Shanghai Women’s Health Study physical activity questionnaire. Am J Epidemiol 158(11):1114–1122. https://doi.org/10.1093/aje/kwg255
Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, O’Brien WL, Bassett DR Jr, Schmitz KH, Emplaincourt PO, Jacobs DR Jr, Leon AS (2000) Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc 32(9 Suppl):S498-504. https://doi.org/10.1097/00005768-200009001-00009
World Health Organization (2010) Global recommendations on physical activity for health. WHO Press, Geneva
Wang H, Zhai F (2013) Programme and policy options for preventing obesity in China. Obes Rev 14(Suppl 2):134–140. https://doi.org/10.1111/obr.12106
Cai H, Zheng W, Xiang YB, Xu WH, Yang G, Li H, Shu XO (2007) Dietary patterns and their correlates among middle-aged and elderly Chinese men: a report from the Shanghai Men’s Health Study. Br J Nutr 98(5):1006–1013. https://doi.org/10.1017/S0007114507750900
Rothman KJ, Greenland S, Lash TL (2011) Modern epidemiology, 3rd edn. Wolters Kluwer Health/ Lippincott Williams & Wilkins, New York
Bamia C, Lagiou P, Jenab M, Aleksandrova K, Fedirko V, Trichopoulos D, Overvad K, Tjonneland A, Olsen A, Clavel-Chapelon F, Boutron-Ruault MC, Kvaskoff M, Katzke VA, Kuhn T, Boeing H, Nothlings U, Palli D, Sieri S, Panico S, Tumino R, Naccarati A, Bueno-de-Mesquita HB, Peeters PH, Weiderpass E, Skeie G, Quiros JR, Agudo A, Chirlaque MD, Sanchez MJ, Ardanaz E, Dorronsoro M, Ericson U, Nilsson LM, Wennberg M, Khaw KT, Wareham N, Key TJ, Travis RC, Ferrari P, Stepien M, Duarte-Salles T, Norat T, Murphy N, Riboli E, Trichopoulou A (2015) Fruit and vegetable consumption in relation to hepatocellular carcinoma in a multi-centre. Eur Cohort Study Br J Cancer 112(7):1273–1282. https://doi.org/10.1038/bjc.2014.654
Zhao L, Jin L, Petrick JL, Zeng H, Wang F, Tang L, Smith-Warner SA, Eliassen AH, Zhang FF, Campbell PT, Giovannucci E, Liao LM, McGlynn KA, Steck SE, Zhang X (2023) Specific botanical groups of fruit and vegetable consumption and liver cancer and chronic liver disease mortality: a prospective cohort study. Am J Clin Nutr 117(2):278–285. https://doi.org/10.1016/j.ajcnut.2022.12.004
Kurahashi N, Inoue M, Iwasaki M, Tanaka Y, Mizokami M, Tsugane S, Group JS (2009) Vegetable, fruit and antioxidant nutrient consumption and subsequent risk of hepatocellular carcinoma: a prospective cohort study in Japan. Br J Cancer 100(1):181–184. https://doi.org/10.1038/sj.bjc.6604843
George SM, Park Y, Leitzmann MF, Freedman ND, Dowling EC, Reedy J, Schatzkin A, Hollenbeck A, Subar AF (2009) Fruit and vegetable intake and risk of cancer: a prospective cohort study. Am J Clin Nutr 89(1):347–353. https://doi.org/10.3945/ajcn.2008.26722
Liu RH (2004) Potential synergy of phytochemicals in cancer prevention: mechanism of action. J Nutr 134(12 Suppl):3479S-3485S. https://doi.org/10.1093/jn/134.12.3479S
Liu RH (2013) Health-promoting components of fruits and vegetables in the diet. Adv Nutr 4(3):384S-392S. https://doi.org/10.3945/an.112.003517
Klurfeld DM (1997) Fiber and cancer protection–mechanisms. Adv Exp Med Biol 427:249–257. https://doi.org/10.1007/978-1-4615-5967-2_26
Fedirko V, Trichopolou A, Bamia C, Duarte-Salles T, Trepo E, Aleksandrova K, Nöthlings U, Lukanova A, Lagiou P, Boffetta P, Trichopoulos D, Katzke VA, Overvad K, Tjønneland A, Hansen L, Boutron-Ruault MC, Fagherazzi G, Bastide N, Panico S, Grioni S, Vineis P, Palli D, Tumino R, Bueno-de-Mesquita HB, Peeters PH, Skeie G, Engeset D, Parr CL, Jakszyn P, Sánchez MJ, Barricarte A, Amiano P, Chirlaque M, Quirós JR, Sund M, Werner M, Sonestedt E, Ericson U, Key TJ, Khaw KT, Ferrari P, Romieu I, Riboli E, Jenab M (2013) Consumption of fish and meats and risk of hepatocellular carcinoma: the European Prospective Investigation into Cancer and Nutrition (EPIC). Ann Oncol 24(8):2166–2173. https://doi.org/10.1093/annonc/mdt168
Freedman ND, Cross AJ, McGlynn KA, Abnet CC, Park Y, Hollenbeck AR, Schatzkin A, Everhart JE, Sinha R (2010) Association of meat and fat intake with liver disease and hepatocellular carcinoma in the NIH-AARP cohort. J Natl Cancer Inst 102(17):1354–1365. https://doi.org/10.1093/jnci/djq301
Ma Y, Yang W, Li T, Liu Y, Simon TG, Sui J, Wu K, Giovannucci EL, Chan AT, Zhang X (2019) Meat intake and risk of hepatocellular carcinoma in two large US prospective cohorts of women and men. Int J Epidemiol 48(6):1863–1871. https://doi.org/10.1093/ije/dyz146
International Coffee Council, 112th Session (2014) Coffee Consumption in East and Southeast Asia: 1990–2012. http://www.ico.org/news/icc-112-4e-consumption-asia.pdf
Qian GS, Ross RK, Yu MC, Yuan JM, Gao YT, Henderson BE, Wogan GN, Groopman JD (1994) A follow-up study of urinary markers of aflatoxin exposure and liver cancer risk in Shanghai, People’s Republic of China. Cancer Epidemiol Biomarkers Prev 3(1):3–10
Acknowledgements
We thank all participants for their contribution to this research.
Funding
This work was supported by the National Key Project of the Research and Development Program of China [2021YFC2500404, 2021YFC2500405]. and the parent cohort was supported by subcontracts from the grants of the US National Institutes of Health [UM1 CA173640, UM1 CA182910]. All funders had no role in the design, analysis, and writing of this article.
Author information
Authors and Affiliations
Contributions
Y-BX designed research and obtained funding; Q-MS, J-YT, Z-YL, J-F, Y-TT, W-Z, H-LL, and Y-BX conducted the study; Q-MS, Y-BX analyzed the data and interpreted the results; J-YT and Y-BX prepared and wrote the first draft; All authors reviewed and approved the final version of the paper; and Y-BX has primary responsibility for final content.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shen, QM., Tuo, JY., Li, ZY. et al. Sex-specific impact of dietary patterns on liver cancer incidence: updated results from two population-based cohort studies in China. Eur J Nutr (2024). https://doi.org/10.1007/s00394-024-03347-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00394-024-03347-5