Abstract
Purpose
Inflammation has been implicated in ovarian carcinogenesis. This study evaluated two dietary indices: the Dietary Inflammatory Index (DII®) and the Empirical Dietary Inflammatory Pattern (EDIP), in relation to risk of developing, and survival following, a diagnosis of ovarian cancer.
Methods
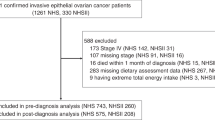
Data came from the Australian Ovarian Cancer Study (1375 cases, 1415 population controls). DII and EDIP scores were computed from dietary information obtained using a semiquantitative food-frequency questionnaire. Logistic regression was used to assess the association between DII and EDIP scores and risk of ovarian cancer and proportional hazards models were used for survival analysis.
Results
A high DII score, reflecting a more pro-inflammatory diet, was associated with a modest increased risk of ovarian cancer [odds ratio (OR) DII scoreQ4 vs.Q1 = 1.31, 95% CI 1.06–1.63, ptrend = 0.014]. Likewise a high EDIP score was associated with an increase in risk of ovarian cancer [OR EDIP scoreQ4 vs.Q1 = 1.39, 95% confidence interval (CI) 1.12–1.73, ptrend = 0.002]. We found no association between DII or EDIP score and overall or ovarian cancer-specific survival.
Conclusion
In conclusion, our results suggest that a pro-inflammatory diet modestly increases the risk of developing ovarian cancer.
Similar content being viewed by others
Change history
28 September 2018
In the original publication of this article on page 6, paragraph “Discussion”, line 4, ‘In a U.S. population-based case–control study (<Emphasis Type="Italic">n</Emphasis> = 493 cases) Peres et al., reported a non-significant association between DII score and risk of developing ovarian cancer of similar magnitude (OR DII score<Subscript>Q4 vs. Q1</Subscript> 1.35, 95% CI 0.93–1.97) [20]’. It should read as ‘In a U.S. population-based case–control study (<Emphasis Type="Italic">n</Emphasis> = 493 cases) Peres et al., reported a significant association between DII score and risk of developing ovarian cancer (OR DII score<Subscript>Q4 vs. Q1</Subscript> 1.72, 95% CI 1.18–2.51) [20]’.
References
Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A (2015) Global cancer statistics, 2012. CA Cancer J Clin 65:87–108
Schuler S, Ponnath M, Engel J, Ortmann O (2013) Ovarian epithelial tumors and reproductive factors: a systematic review. Arch Gynecol Obstet 287:1187–1204
Rice MS, Murphy MA, Tworoger SS (2012) Tubal ligation, hysterectomy and ovarian cancer: a meta-analysis. J Ovarian Res 5:13
Ness RB, Cottreau C (1999) Possible role of ovarian epithelial inflammation in ovarian cancer. J Natl Cancer Inst 91:1459–1467
Shan W, Liu J (2009) Inflammation: a hidden path to breaking the spell of ovarian cancer. Cell Cycle 8:3107–3111
Galland L (2010) Diet and inflammation. Nutr Clin Pract 25:634–640
Grosso G, Bella F, Godos J, Sciacca S, Del Rio D, Ray S et al (2017) Possible role of diet in cancer: systematic review and multiple meta-analyses of dietary patterns, lifestyle factors, and cancer risk. Nutr Rev 75:405–419
Nagle CM, Purdie DM, Webb PM, Green A, Harvey PW, Bain CJ (2003) Dietary influences on survival after ovarian cancer. Int J Cancer 106:264–269
Playdon MC, Nagle CM, Ibiebele TI, Ferrucci LM, Protani MM, Carter J et al (2017) Pre-diagnosis diet and survival after a diagnosis of ovarian cancer. Br J Cancer 116:1627–1637
Sueblinvong T, Carney ME (2009) Current understanding of risk factors for ovarian cancer. Curr Treat Options Oncol 10:67–81
World Cancer Research Fund /American Institute for Cancer Research (2015) Continuous update project report. Food, nutrition, physical activity, and the prevention of ovarian cancer 2014. http://www.dietandcancerreport.org/cup/cup_resources.php. Accessed 20 Jan 2018
Barkoukis H (2007) Importance of understanding food consumption patterns. J Am Diet Assoc 107:234–236
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13:3–9
Jacques PF, Tucker KL (2001) Are dietary patterns useful for understanding the role of diet in chronic disease? Am J Clin Nutr 73:1–2
Arem H, Reedy J, Sampson J, Jiao L, Hollenbeck AR, Risch H et al (2013) The Healthy Eating Index 2005 and risk for pancreatic cancer in the NIH-AARP study. J Natl Cancer Inst 105:1298–1305
Li WQ, Park Y, Wu JW, Goldstein AM, Taylor PR, Hollenbeck AR et al (2014) Index-based dietary patterns and risk of head and neck cancer in a large prospective study. Am J Clin Nutr 99:559–566
Qin B, Moorman PG, Kelemen LE, Alberg AJ, Barnholtz-Sloan JS, Bondy M et al (2017) Dietary quality and ovarian cancer risk in African–American women. Am J Epidemiol 185:1281–1289
Shivappa N, Steck SE, Hurley TG, Hussey JR, Hebert JR (2014) Designing and developing a literature-derived, population-based dietary inflammatory index. Public Health Nutr 17:1689–1696
Tabung FK, Smith-Warner SA, Chavarro JE, Wu K, Fuchs CS, Hu FB et al (2016) Development and validation of an Empirical Dietary Inflammatory Index. J Nutr 146:1560–1570
Peres LC, Bandera EV, Qin B, Guertin KA, Shivappa N, Hebert JR et al (2017) Dietary inflammatory index and risk of epithelial ovarian cancer in African American women. Int J Cancer 140:535–543
Shivappa N, Hebert JR, Paddock LE, Rodriguez-Rodriguez L, Olson SH, Bandera EV (2018) Dietary inflammatory index and ovarian cancer risk in a New Jersey case-control study. Nutrition 46:78–82
Shivappa N, Hebert JR, Rosato V, Rossi M, Montella M, Serraino D et al (2016) Dietary inflammatory index and ovarian cancer risk in a large Italian case-control study. Cancer Causes Control 27:897–906
Tabung FK, Huang T, Giovannucci EL, Smith-Warner SA, Tworoger SS, Poole EM (2017) The inflammatory potential of diet and ovarian cancer risk: results from two prospective cohort studies. Br J Cancer 117:907–911
Merritt MA, Green AC, Nagle CM, Webb PM, Australian Cancer Study (Ovarian Cancer), Australian Ovarian Cancer Study Group (2008) Talcum powder, chronic pelvic inflammation and NSAIDs in relation to risk of epithelial ovarian cancer. Int J Cancer 122:170–176
Willett WC, Sampson L, Stampfer MJ, Rosner B, Bain C, Witschi J et al (1985) Reproducibility and validity of a semiquantitative food frequency questionnaire. Am J Epidemiol 122:51–65
Ashton B (1996) Under-reporting of energy intake in two methods of dietary assessment in the Nambour Trial. Aust J Nutr Diet 53:53–60
Marks GC, Hughes MC, van der Pols JC (2006) The effect of personal characteristics on the validity of nutrient intake estimates using a food-frequency questionnaire. Public Health Nutr 9:394–402
McNaughton SA, Marks GC, Gaffney P, Williams G, Green A (2005) Validation of a food-frequency questionnaire assessment of carotenoid and vitamin E intake using weighed food records and plasma biomarkers: the method of triads model. Eur J Clin Nutr 59:211–218
Marks GC, Hughes MC, van der Pols JC (2006) Relative validity of food intake estimates using a food frequency questionnaire is associated with sex, age, and other personal characteristics. J Nutr 136:459–465
Ibiebele TI, Parekh S, Mallitt KA, Hughes MC, O’Rourke PK, Webb PM et al (2009) Reproducibility of food and nutrient intake estimates using a semi-quantitative FFQ in Australian adults. Public Health Nutr 12:2359–2365
Food Standards Australia New Zealand (2007) NUTTAB 2006 Australian food composition tables. Food Standards Australian New Zealand, Canberra
Shivappa N, Steck SE, Hurley TG, Hussey JR, Ma Y, Ockene IS et al (2014) A population-based dietary inflammatory index predicts levels of C-reactive protein in the Seasonal Variation of Blood Cholesterol Study (SEASONS). Public Health Nutr 17:1825–1833
Tabung FK, Steck SE, Zhang J, Ma Y, Liese AD, Agalliu I et al (2015) Construct validation of the dietary inflammatory index among postmenopausal women. Ann Epidemiol 25:398–405
Hamalainen M, Nieminen R, Vuorela P, Heinonen M, Moilanen E (2007) Anti-inflammatory effects of flavonoids: genistein, kaempferol, quercetin, and daidzein inhibit STAT-1 and NF-kappaB activations, whereas flavone, isorhamnetin, naringenin, and pelargonidin inhibit only NF-kappaB activation along with their inhibitory effect on iNOS expression and NO production in activated macrophages. Mediators Inflamm 2007:10. https://doi.org/10.1155/2007/45673
Crane TE, Khulpateea BR, Alberts DS, Basen-Engquist K, Thomson CA (2014) Dietary intake and ovarian cancer risk: a systematic review. Cancer Epidemiol Biomarkers Prev 23:255–273
Ose J, Schock H, Tjonneland A, Hansen L, Overvad K, Dossus L et al (2015) Inflammatory markers and risk of epithelial ovarian cancer by tumor subtypes: the EPIC cohort. Cancer Epidemiol Biomarkers Prev 24:951–961
Trabert B, Pinto L, Hartge P, Kemp T, Black A, Sherman ME et al (2014) Pre-diagnostic serum levels of inflammation markers and risk of ovarian cancer in the prostate, lung, colorectal and ovarian cancer (PLCO) screening trial. Gynecol Oncol 135:297–304
Poole EM, Lee IM, Ridker PM, Buring JE, Hankinson SE, Tworoger SS (2013) A prospective study of circulating C-reactive protein, interleukin-6, and tumor necrosis factor alpha receptor 2 levels and risk of ovarian cancer. Am J Epidemiol 178:1256–1264
Gupta M, Babic A, Beck AH, Terry K (2016) TNF-alpha expression, risk factors, and inflammatory exposures in ovarian cancer: evidence for an inflammatory pathway of ovarian carcinogenesis? Hum Pathol 54:82–91
Renehan AG, Zwahlen M, Minder C, O’Dwyer ST, Shalet SM, Egger M (2004) Insulin-like growth factor (IGF)-I, IGF binding protein-3, and cancer risk: systematic review and meta-regression analysis. Lancet 363:1346–1353
Lukanova A, Lundin E, Micheli A, Arslan A, Ferrari P, Rinaldi S et al (2004) Circulating levels of sex steroid hormones and risk of endometrial cancer in postmenopausal women. Int J Cancer 108:425–432
Lukanova A, Kaaks R (2005) Endogenous hormones and ovarian cancer: epidemiology and current hypotheses. Cancer Epidemiol Biomarkers Prev 14:98–107
Kaaks R (2001) Plasma insulin, IGF-I and breast cancer. Gynecol Obstet Fertil 29:185–191
Kaaks R, Lukanova A, Rinaldi S, Biessy C, Soderberg S, Olsson T et al (2003) Interrelationships between plasma testosterone, SHBG, IGF-I, insulin and leptin in prostate cancer cases and controls. Eur J Cancer Prev 12:309–315
Zhu J, Wang H, Liu CC, Lu Y, Tang H (2016) The Glasgow Prognostic Score (GPS) is a novel prognostic indicator in advanced epithelial ovarian cancer: a multicenter retrospective study. J Cancer Res Clin Oncol 142:2339–2345
Lu Y, Huang S, Li P, Chen B, Liu W, Chen Z et al (2015) Prognostic evaluation of preoperative serum C-reactive protein concentration in patients with epithelial ovarian cancer. Exp Ther Med 9:2003–2007
Zhang WW, Liu KJ, Hu GL, Liang WJ (2015) Preoperative platelet/lymphocyte ratio is a superior prognostic factor compared to other systemic inflammatory response markers in ovarian cancer patients. Tumour Biol 36:8831–8837
Omichi C, Nakamura K, Haraga J, Masuyama H, Hiramatsu Y (2016) Glasgow prognostic score is an independent marker for poor prognosis with all cases of epithelial ovarian cancer. Cancer Med 5:1074–1080
Scambia G, Testa U, Benedetti Panici P, Foti E, Martucci R, Gadducci A et al (1995) Prognostic significance of interleukin 6 serum levels in patients with ovarian cancer. Br J Cancer 71:354–356
Lutgendorf SK, Weinrib AZ, Penedo F, Russell D, DeGeest K, Costanzo ES et al (2008) Interleukin-6, cortisol, and depressive symptoms in ovarian cancer patients. J Clin Oncol 26:4820–4827
Deng FE, Shivappa N, Tang Y, Mann JR, Hebert JR (2017) Association between diet-related inflammation, all-cause, all-cancer, and cardiovascular disease mortality, with special focus on prediabetics: findings from NHANES III. Eur J Nutr 56:1085–1093
Shivappa N, Blair CK, Prizment AE, Jacobs DR Jr, Steck SE, Hebert JR (2016) Association between inflammatory potential of diet and mortality in the Iowa Women’s Health study. Eur J Nutr 55:1491–1502
Shivappa N, Harris H, Wolk A, Hebert JR (2016) Association between inflammatory potential of diet and mortality among women in the Swedish Mammography Cohort. Eur J Nutr 55:1891–1900
Zucchetto A, Gini A, Shivappa N, Hebert JR, Stocco C, Dal Maso L et al (2016) Dietary inflammatory index and prostate cancer survival. Int J Cancer 139:2398–2404
Shivappa N, Hebert JR, Kivimaki M, Akbaraly T (2017) Alternate Healthy Eating Index 2010, Dietary Inflammatory Index and risk of mortality: results from the Whitehall II cohort study and meta-analysis of previous Dietary Inflammatory Index and mortality studies. Br J Nutr 118:210–221
Shivappa N, Steck SE, Hussey JR, Ma Y, Hebert JR (2017) Inflammatory potential of diet and all-cause, cardiovascular, and cancer mortality in National Health and Nutrition Examination Survey III Study. Eur J Nutr 56:683–692
Thomson CA, T EC, Wertheim BC, Neuhouser ML, Li W, Snetselaar LG et al (2014) Diet quality and survival after ovarian cancer: results from the Women’s Health Initiative. J Natl Cancer Inst 106
Scheurig AC, Thorand B, Fischer B, Heier M, Koenig W (2008) Association between the intake of vitamins and trace elements from supplements and C-reactive protein: results of the MONICA/KORA Augsburg study. Eur J Clin Nutr 62:127–137
Fleischauer AT, Olson SH, Mignone L, Simonsen N, Caputo TA, Harlap S (2001) Dietary antioxidants, supplements, and risk of epithelial ovarian cancer. Nutr Cancer 40:92–98
Cramer DW, Kuper H, Harlow BL, Titus-Ernstoff L (2001) Carotenoids, antioxidants and ovarian cancer risk in pre- and postmenopausal women. Int J Cancer 94:128–134
Gifkins D, Olson SH, Paddock L, King M, Demissie K, Lu SE et al (2012) Total and individual antioxidant intake and risk of epithelial ovarian cancer. BMC Cancer 12:211
Tung KH, Wilkens LR, Wu AH, McDuffie K, Hankin JH, Nomura AM et al (2005) Association of dietary vitamin A, carotenoids, and other antioxidants with the risk of ovarian cancer. Cancer Epidemiol Biomarkers Prev 14:669–676
Pandeya N, Williams GM, Green AC, Webb PM, Whiteman DC (2009) Do low control response rates always affect the findings? Assessments of smoking and obesity in two Australian case-control studies of cancer. Aust N Z J Public Health 33:312–319
Acknowledgements
We gratefully acknowledge the members of the Australian Ovarian Cancer Study Group including all the clinical and scientific collaborators, participating institutions, study nurses and research assistants (see http://www.aocstudy.org/ for a complete listing), and thank all of the women who participated in the study. We also acknowledge staff at the Australian Institute of Health and Welfare for conducting the linkage to the Australian National Death Index and Maria Celia Hughes from the QIMR Berghofer Medical Research Institute for preparation of the dietary data.
Funding
The Australian Ovarian Cancer Study was supported by the U.S. Army Medical Research and Materiel Command (DAMD17-01-1-0729), the National Health and Medical Research Council (NHMRC) of Australia (Grants 400281, 400413, 199600), the Cancer Councils of Victoria, Queensland, New South Wales, South Australia and Tasmania and the Cancer Foundation of Western Australia. CMN and TII were supported by NHMRC Program Grant, PMW by a fellowship from the NHMRC and AdeF was funded by the University of Sydney Cancer Research Fund and the Cancer Institute NSW through the Sydney-West Translational Cancer Research Centre. The funders had no role in the design, analysis or writing of this article.
Author information
Authors and Affiliations
Consortia
Contributions
The authors’ responsibilities were as follows—CMN : designed the analysis, wrote the manuscript, and took responsibility for the final content; TI: was responsible for the dietary data including calculation of EDIP, and conducted the statistical analysis; AdF: was responsible for collection of the clinical data; NS and JRH calculated the DII and edited the manuscript; PMW designed the founding case–control study, contributed to the analysis and interpretation of the results; and all authors contributed to, reviewed, and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
We declare no conflicts of interest.
Disclosure
Dr. Hébert owns controlling interest in Connecting Health Innovations LLC (CHI), a company planning to license the right to his invention of the dietary inflammatory index (DII) from the University of South Carolina to develop computer and smart phone applications for patient counseling and dietary intervention in clinical settings. Dr. Nitin Shivappa is an employee of CHI.
Ethical considerations
The study received approval from the appropriate ethics committee and all participants provided informed consent.
Declaration
All named authors have read the manuscript and have agreed to submit the paper in its present form. The research has not been and will not be submitted simultaneously to another journal, in whole or in part. The paper reports previously unpublished work. All those named as authors have made a sufficient contribution to the work. Any specific consent to publish required by employers or funding bodies was obtained.
Additional information
The original version of this article was revised. On page 6, paragraph “Discussion”, line 4, ‘In a U.S. population-based case–control study (n = 493 cases) Peres et al., reported a non-significant association between DII score and risk of developing ovarian cancer of similar magnitude (OR DII scoreQ4 vs. Q1 1.35, 95% CI 0.93–1.97) [20]’. It should read as ‘In a U.S. population-based case–control study (n = 493 cases) Peres et al., reported a significant association between DII score and risk of developing ovarian cancer (OR DII scoreQ4 vs. Q1 1.72, 95% CI 1.18–2.51) [20]’.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Nagle, C.M., Ibiebele, T., Shivappa, N. et al. The association between the inflammatory potential of diet and risk of developing, and survival following, a diagnosis of ovarian cancer. Eur J Nutr 58, 1747–1756 (2019). https://doi.org/10.1007/s00394-018-1779-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-018-1779-x