Abstract
Purpose
Diabetes and obesity are characterized by glucose intolerance, fat deposition, inflammation, and dyslipidemia. Recent reports postulated that distinct gut microbiota alterations were observed in obese/diabetic subjects and modulating gut microbiota beneficially through specific probiotics could be a potential therapeutic option for type 2 diabetes/obesity. Therefore, we attempted to study the efficacy of probiotics of Indian gut origin (Lactobacillus plantarum MTCC5690 and Lactobacillus fermentum MTCC5689) along with a positive control, Lactobacillus rhamnosus (LGG) on glucose/lipid homeostasis in high-fat-diet-induced diabetic animal model.
Methods
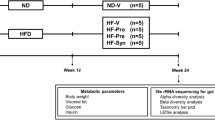
C57BL/6J male mice were divided into seven groups (n = 6 per group) comprising feeding on: (1) Normal Pellet Diet (NPD), (2) High-Fat Diet (HFD), (3) HFD with LGG, (4) HFD with MTCC5690, (5) HFD with MTCC5689, (6) HFD with metformin, and 7) HFD with vildagliptin for a period of 6 months. Biochemical markers, glucose tolerance, insulin resistance, and GLP-1 and LPS levels were assessed by standard protocols. Gut integrity was measured by intestinal permeability test. Transcriptional levels of tight junction proteins (TJPs) were probed in small intestinal tissues while inflammatory signals and other pathway specific genes were profiled in liver, visceral adipose tissue, and skeletal muscle.
Results
Mice fed with HFD became insulin resistant, glucose intolerant, hyperglycemic, and dyslipidemic. Diabetic mice were characterized to exhibit decreased levels of GLP-1, increased gut permeability, increased circulatory levels of LPS, decrease in the gene expression patterns of intestinal tight junction markers (occludin and ZO-1), and increased proinflammatory gene markers (TNFα and IL6) in visceral fat along with decreased mRNA expression of FIAF and adiponectin. Diabetic mice also exhibited increased mRNA expression of ER stress markers in skeletal muscle. In addition, liver from HFD-fed diabetic mice showed increased gene expressions of proinflammation, lipogenesis, and gluconeogenesis. Probiotic interventions (most prominently the MTCC5689) resisted insulin resistance and development of diabetes in mice under HFD feeding and beneficially modulated all the biochemical and molecular alterations in a mechanistic way in several tissues. The metabolic benefits offered by the probiotics were also more or less similar to that of standard drugs such as metformin and vildagliptin.
Conclusion
Native probiotic strains MTCC 5690 and MTCC 5689 appear to have potential against insulin resistance and type 2 diabetes with mechanistic, multiple tissue-specific mode of actions.









Similar content being viewed by others
Abbreviations
- MTCC 5690:
-
Lactobacillus plantarum Lp91
- MTCC 5689:
-
Lactobacillus fermentum Lf1
- LGG:
-
Lactobacillus rhamnosus GG
- FIAF:
-
Fasting-induced adipocyte factor
- ZO-1:
-
Zonula occludens-1
- NPD:
-
Normal pellet diet
- HFD:
-
High-fat diet
- IL6:
-
Interleukin 6
- TNFα:
-
Tumor necrosis factor alpha
- LPS:
-
Lipopolysaccharide
- GRP78:
-
Glucose-regulated protein 78
- PERK:
-
Protein kinase R (PKR)-like endoplasmic reticulum kinase
- IRE1-α:
-
Inositol-requiring enzyme 1 alpha
- XBP1:
-
X-box-binding protein 1
- CHOP:
-
CCAAT-enhancer-binding protein homologous protein
- SREBP-1c:
-
Sterol regulatory element-binding protein 1 (SREBP-1)
- GLUT4:
-
Glucose transporter, member 4
- MCP1:
-
Monocyte chemoattractant protein-1
- GCK:
-
Glucokinase
- PEPCK:
-
Phosphoenolpyruvate carboxykinase
- G6Pc:
-
Glucose-6-phosphatase catalytic subunit
- FOXO1:
-
Forkhead box protein O1
References
Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, Bhansali A, Joshi SR, Joshi PP, Yajnik CS, Dhandhania VK, Nath LM, Das AK, Rao PV, Madhu SV, Shukla DK, Kaur T, Priya M, Nirmal E, Parvathi SJ, Subhashini S, Subashini R, Ali MK, Mohan V, Group II (2011) Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: phase I results of the Indian Council of Medical Research- INdiaDIABetes (ICMR-INDIAB) study. Diabetologia 54:3022–3027. doi:10.1007/s00125-011-2291-5
Mohan V, Sudha V, Radhika G, Radha V, Rema M, Deepa R (2007) Gene-environment interactions and the diabetes epidemic in India. Forum Nutr 60:118–126. doi:10.1159/0000107088
Cani PD, Bibiloni R, Knauf C, Waget A, Neyrinck AM, Delzenne NM, Burcelin R (2008) Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57:1470–1481. doi:10.2337/db07-1403
FAO/WHO (2002) Working Group Report on Drafting Guidelines for the Evaluation of Probiotics in Food London, Ontario, Canada
Yadav H, Jain S, Sinha PR (2007) Antidiabetic effect of probiotic dahi containing Lactobacillus acidophilus and Lactobacillus casei in high fructose fed rats. Nutrition (Burbank, Los Angeles County, Calif.) 23:62–68. doi:10.1016/j.nut.2006.09.002
Matsuzaki T, Nagata Y, Kado S, Uchida K, Kato I, Hashimoto S, Yokokura T (1997) Prevention of onset in an insulin-dependent diabetes mellitus model, NOD mice, by oral feeding of Lactobacillus casei. Actapathol Microbiol Immunol Scand 105:643–649
Kadooka Y, Sato M, Imaizumi K, Ogawa A, Ikuyama K, Akai Y, Okano M, Kagoshima M, Tsuchida T (2010) Regulation of abdominal adiposity by probiotics (Lactobacillus gasseri SBT2055) in adults with obese tendencies in a randomized controlled trial. Euro J Clin Nutr 64:636–643. doi:10.1038/ejcn.2010.19
Cani PD, Lecourt E, Dewulf EM, Sohet FM, Pachikian BD, Naslain D, De Backer F, Neyrinck AM, Delzenne NM (2009) Gut microbiota fermentation of prebiotics increases satietogenic and incretin gut peptide production with consequences for appetite sensation and glucose response after a meal. Am J Clin Nutr 90:1236–1243. doi:10.3945/ajcn.2009.28095
Kaji I, Karaki S-I, Tanaka R, Kuwahara A (2011) Density distribution of free fatty acid receptor 2 (FFA2)-expressing and GLP-1-producing enteroendocrine L cells in human and rat lower intestine, and increased cell numbers after ingestion of fructo-oligosaccharide. J Mol Histol 42:27–38. doi:10.1007/s10735-010-9304-4
Simon M-CC, Strassburger K, Nowotny B, Kolb H, Nowotny P, Burkart V, Zivehe F, Hwang J-HH, Stehle P, Pacini G, Hartmann B, Holst JJ, MacKenzie C, Bindels LB, Martinez I, Walter J, Henrich B, Schloot NC, Roden M (2015) Intake of Lactobacillus reuteri improves incretin and insulin secretion in glucose-tolerant humans: a proof of concept. Diabetes Care 38:1827–1834. doi:10.2337/dc14-2690
Grover S, Sharma VK, Mallapa RH, Batish VK (2013) Draft Genome Sequence of Lactobacillus fermentum Lf1, an Indian isolate of human gut origin. Genome Announc 14(1(6)): pii: e00883–13. doi: 10.1128/genomeA.00883-13
Grover S, Sharma VK, Mallapa RH, Batish VK (2013) Draft genome sequence of lactobacillus plantarum strain Lp91, a promising Indian probiotic isolate of human gut origin. Genome Announc 21;1(6): pii:e00976–13. doi:10.1128/genomeA.00976-13
Kumar R, Grover S, Batish VK (2011) Hypocholesterolaemic effect of dietary inclusion of two putative probiotic bile salt hydrolase-producing Lactobacillus plantarum strains in Sprague-Dawley rats. Br J Nutr 105:561–573. doi:10.1017/S0007114510003740
Duary RK, Rajput YS, Batish VK, Grover S (2011) Assessing the adhesion of putative indigenous probiotic lactobacilli to human colonic epithelial cells. Indian J Med Res 134:664–671. doi:10.4103/0971-5916.90992
Duary RK, Bhausaheb MA, Batish VK, Grover S (2012) Anti-inflammatory and immunomodulatory efficacy of indigenous probiotic Lactobacillus plantarum Lp91 in colitis mouse model. Mol Biol Rep 39:4765–4775
Chandran A, Duary RK, Grover S, Batish VK (2013) Relative expression of bacterial and host specific genes associated with probiotic survival and viability in the mice gut fed with Lactobacillus plantarum Lp91. Microbiol Res 168:555–562
AparnaSudhakaran V, Panwar H, Chauhan R, Duary RK, Rathore RK, Batish VK, Grover S (2013) Modulation of anti-inflammatory response in lipopolysaccharide stimulated human THP-1 cell line and mouse model at gene expression level with indigenous putative probiotic lactobacilli. Genes Nutr 8:637–648
Chauhan R, Vasanthakumari AS, Panwar H, Mallapa RH, Duary RK, Batish VK, Grover SC (2014) Amelioration of colitis in mouse model by exploring antioxidative potentials of an indigenous probiotic strain of Lactobacillus fermentum Lf1. BioMed Res Int 2014:206732
Whiting MJ, Shephard MD, Tallis GA (1997) Measurement of plasma LDL cholesterol in patients with diabetes. Diabetes Care 20:12–14
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Zhang JQ, Gao CR, Huang QL (1997) Determination of insulin sensitivity by short insulin tolerance test using capillary blood glucose. Chin J Endocrinol Metab 13:77–80
Srinivasan K, Patole PS, Kaul CL, Ramarao P (2004) Reversal of glucose intolerance by pioglitazone in high fat diet-fed rats. Methods Find Exp Clin Pharmacol 26:327–333
Wang Q, Fang CH, Hasselgren PO (2001) Intestinal permeability is reduced and IL-10 levels are increased in septic IL-6 knockout mice. Am J Physiol Regul Integr Comp Physiol 281:23
Balasubramanyam M, Aravind S, Gokulakrishnan K, Prabu P, Sathishkumar C, Ranjani H, Mohan V (2011) Impaired miR-146a expression links subclinical inflammation and insulin resistance in Type 2 diabetes. Mol Cell Biochem 351:197–205. doi:10.1007/s11010-011-0727-3
Karimi G, Sabran MR, Jamaluddin R, Parvaneh K, Mohtarrudin N, Ahmad Z, Khazaai H, Khodavandi A (2015) The anti-obesity effects of Lactobacillus casei strain Shirota versus Orlistat on high fat diet-induced obese rats. Food Nutr Res 59:29273. doi:10.3402/fnr.v59.29273
Hsieh F-CC, Lee C-LL, Chai C-YY, Chen W-TT, Lu Y-CC, Wu C-SS (2013) Oral administration of Lactobacillus reuteri GMNL-263 improves insulin resistance and ameliorates hepatic steatosis in high fructose-fed rats. Nutr Metab 10:35. doi:10.1186/1743-7075-10-35
Ooi L-GG, Liong M-TT (2010) Cholesterol-lowering effects of probiotics and prebiotics: a review of in vivo and in vitro findings. Int J Mol Sci 11:2499–2522. doi:10.3390/ijms11062499
Corcos M, Guilbaud O, Paterniti S, Moussa M, Chambry J, Chaouat G, Consoli SM, Jeammet P (2003) Involvement of cytokines in eating disorders: a critical review of the human literature. Psychoneuroendocrinology 28:229–249
Kim K-AA, Gu W, Lee I-AA, Joh E-HH, Kim D-HH (2012) High fat diet-induced gut microbiota exacerbates inflammation and obesity in mice via the TLR4 signaling pathway. PloS One 7. doi:10.1371/journal.pone.0047713
Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, Bastelica D, Neyrinck AM, Fava F, Tuohy KM, Chabo C, Waget A, Delmée E, Cousin B, Sulpice T, Chamontin B, Ferrières J, Tanti J-FF, Gibson GR, Casteilla L, Delzenne NM, Alessi MC, Burcelin R (2007) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56:1761–1772. doi:10.2337/db06-1491
Everard A, Cani PD (2013) Diabetes, obesity and gut microbiota. Best practice & research. Clin Gastroenterol 27:73–83. doi:10.1016/j.bpg.2013.03.007
Jayashree B, Bibin YS, Prabhu D, Shanthirani CS, Gokulakrishnan K, Lakshmi BS, Mohan V, Balasubramanyam M (2014) Increased circulatory levels of lipopolysaccharide (LPS) and zonulin signify novel biomarkers of proinflammation in patients with type 2 diabetes. Mol Cell Biochem 388:203–210. doi:10.1007/s11010-013-1911-4
Naito E, Yoshida Y, Makino K, Kounoshi Y, Kunihiro S, Takahashi R, Matsuzaki T, Miyazaki K, Ishikawa F (2011) Beneficial effect of oral administration of Lactobacillus casei strain Shirota on insulin resistance in diet-induced obesity mice. J Appl Microbiol 110:650–657. doi:10.1111/j.1365-2672.2010.04922.x
Amar J, Chabo C, Waget A, Klopp P, Vachoux C, Bermúdez-Humarán LG, Smirnova N, Bergé M, Sulpice T, Lahtinen S, Ouwehand A, Langella P, Rautonen N, Sansonetti PJ, Burcelin R (2011) Intestinal mucosal adherence and translocation of commensal bacteria at the early onset of type 2 diabetes: molecular mechanisms and probiotic treatment. EMBO Mol Med 3:559–572. doi:10.1002/emmm.201100159
D’Alessio DA, Denney AM, Hermiller LM, Prigeon RL, Martin JM, Tharp WG, Saylan ML, He Y, Dunning BE, Foley JE, Pratley RE (2009) Treatment with the dipeptidyl peptidase-4 inhibitor vildagliptin improves fasting islet-cell function in subjects with type 2 diabetes. J Clin Endocrinol Metab 94:81–88. doi:10.1210/jc.2008-1135
Mannucci E, Tesi F, Bardini G, Ognibene A, Petracca MG, Ciani S, Pezzatini A, BrogiM Dicembrini I, Cremasco F, Messeri G, Rotella CM (2004) Effects of metformin on glucagon-like peptide-1 levels in obese patients with and without Type 2 diabetes. Diab Nutr Metab 17:336–342
Lim GE, Huang GJ, Flora N, LeRoith D, Rhodes CJ, Brubaker PL (2009) Insulin regulates glucagon-like peptide-1 secretion from the enteroendocrine L cell. Endocrinology 150:580–591. doi:10.1210/en.2008-0726
Stenman LK, Waget A, Garret C, Briand F, Burcelin R, Sulpice T, Lahtinen S (2015) Probiotic B420 and prebiotic polydextrose improve efficacy of antidiabetic drugs in mice. Diabetol Metab Syndr 7:75. doi:10.1186/s13098-015-0075-7
Wong JM, de Souza R, Kendall CW, Emam A, Jenkins DJ (2006) Colonic health: fermentation and short chain fatty acids. J Clin Gastroenterol 40:235–243
S-i Karaki, Mitsui R, Hayashi H, Kato I, Sugiya H, Iwanaga T, Furness JB, Kuwahara A (2006) Short-chain fatty acid receptor, GPR43, is expressed by enteroendocrine cells and mucosal mast cells in rat intestine. Cell Tissue Res 324:353–360. doi:10.1007/s00441-005-0140-x
Pereira DI, Gibson GR (2002) Effects of consumption of probiotics and prebiotics on serum lipid levels in humans. Crit Rev Biochem Mol Biol 37:259–281. doi:10.1080/10409230290771519
Qin J, Li Y, Cai Z, Li S, Zhu J, Zhang F, Liang S, Zhang W, Guan Y, Shen D, Peng Y, Zhang D, Jie Z, Wu W, Qin Y, Xue W, Li J, Han L, Lu D, Wu P, Dai Y, Sun X, Li Z, Tang A, Zhong S, Li X, Chen W, Xu R, Wang M, Feng Q, Gong M, Yu J, Zhang Y, Zhang M, Hansen T, Sanchez G, Raes J, Falony G, Okuda S, Almeida M, LeChatelier E, Renault P, Pons N, Batto J-MM, Zhang Z, Chen H, Yang R, Zheng W, Li S, Yang H, Wang J, Ehrlich SD, Nielsen R, Pedersen O, Kristiansen K, Wang J (2012) A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 490:55–60. doi:10.1038/nature11450
Forslund K, Hildebrand F, Nielsen T, Falony G, Le Chatelier E, Sunagawa S, Prifti E, Vieira-Silva S, Gudmundsdottir V, Krogh Pedersen H, Arumugam M, Kristiansen K, Voigt AY, Vestergaard H, Hercog R, Igor Costea P, Kultima JR, Li J, Jørgensen T, Levenez F, Dore J, consortium M, Nielsen HB, Brunak S, Raes J, Hansen T, Wang J, Ehrlich SD, Bork P, Pedersen O (2015) Disentangling type 2 diabetes and metformin treatment signatures in the human gut microbiota. Nature 528:262–266. doi:10.1038/nature15766
Mandard S, Zandbergen F, van Straten E, Wahli W, Kuipers F, Müller M, Kersten S (2006) The fasting-induced adipose factor/angiopoietin-like protein 4 is physically associated with lipoproteins and governs plasma lipid levels and adiposity. J Biol Chem 281:934–944. doi:10.1074/jbc.M506519200
Shen J, Obin MS, Zhao L (2013) The gut microbiota, obesity and insulin resistance. Mol Aspects Med 34:39–58. doi:10.1016/j.mam.2012.11.001
Bäckhed F, Manchester JK, Semenkovich CF, Gordon JI (2007) Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci USA 104:979–984. doi:10.1073/pnas.0605374104
Aronsson L, Huang Y, Parini P, Korach-André M, Håkansson J, Gustafsson J-ÅÅ, Pettersson S, Arulampalam V, Rafter J (2010) Decreased fat storage by Lactobacillus paracasei is associated with increased levels of angiopoietin-like 4 protein (ANGPTL4). PloS One 5. doi:10.1371/journal.pone.0013087
Kim SW, Park KY, Kim B, Kim E, Hyun CK (2013) Lactobacillus rhamnosus GG improves insulin sensitivity and reduces adiposity in high-fat diet-fed mice through enhancement of adiponectin production. Biochem Biophys Res Commun 431:258–263. doi:10.1016/j.bbrc.2012.12.121
Flamment M, Hajduch E, Ferré P, Foufelle F (2012) New insights into ER stress-induced insulin resistance. Trend Endocrinol Metab 23:381–390. doi:10.1016/j.tem.2012.06.003
Lenin R, Sankaramoorthy A, Mohan V, Balasubramanyam M (2015) Altered immunometabolism at the interface of increased endoplasmic reticulum (ER) stress in patients with type 2 diabetes. J Leukocyte Biol 98:615–622. doi:10.1189/jlb.3A1214-609R
Park KY, Kim B, Hyun CK (2015) Lactobacillus rhamnosus GG improves glucose tolerance through alleviating ER stress and suppressing macrophage activation in db/db mice. J Clin Biochem Nutr 56:240–246. doi:10.3164/jcbn.14-116
Bleau C, Karelis AD, St-Pierre DH, Lamontagne L (2015) Crosstalk between intestinal microbiota, adipose tissue and skeletal muscle as an early event in systemic low-grade inflammation and the development of obesity and diabetes. Diabetes Metab Res Rev 31:545–561. doi:10.1002/dmrr.2617
Yoo SR, Kim YJ, Park DY, Jung UJ, Jeon SM, Ahn YT, Huh CS, McGregor R, Choi MS (2013) Probiotics L. plantarum and L. curvatus in combination alter hepatic lipid metabolism and suppress diet-induced obesity. Obesity (Silver Spring) 21:2571–2578. doi:10.1002/oby.20428
Firouzi S, Majid HA, Ismail A, Kamaruddin NA, Barakatun-Nisak M-YY (2016) Effect of multi-strain probiotics (multi-strain microbial cell preparation) on glycemic control and other diabetes-related outcomes in people with type 2 diabetes: a randomized controlled trial. Eur J Nutr. doi:10.1007/s00394-016-1199-8
Rajkumar H, Kumar M, Das N, Kumar SN, Challa HR, Nagpal R (2015) Effect of probiotic lactobacillussalivarius UBL S22 and prebiotic fructo-oligosaccharide on serum lipids, inflammatory markers, insulin sensitivity, and gut bacteria in healthy young volunteers: a randomized controlled single-blind pilot study. J Cardiovascularpharmacol Therap 20:289–298
Sun J, Buys NJ (2016) Glucose- and glycemic factor lowering effects of probiotics on diabetes: a meta-analysis of randomisedplacebo-controlled trials. Br J Nutr 115:1167–1177
Tonucci LB, Olbrich Dos Santos KM, Licursi de Oliveira L, Rocha Ribeiro SM, Duarte Martino HS (2015) Clinical application of probiotics in type 2 diabetes mellitus: A randomized, double-blind, placebo-controlled study. Clin Nutr. doi:10.1016/j.clnu.2015.11.011
Sáez-Lara MJ, Robles-Sanchez C, Ruiz-Ojeda FJ, Plaza-Diaz J, Gil A (2016) Effects of probiotics and synbiotics on obesity, insulin resistance syndrome, type 2 diabetes and non-alcoholic fatty liver disease: a review of human clinical trials. Int J Mol Sci 13;17: pii: E928. doi:10.3390/ijms17060928
Acknowledgments
Financial assistance from Department of Biotechnology (DBT, New Delhi, Government of India) is greatly acknowledged. BM acknowledges Council of Scientific and Industrial Research (CSIR), New Delhi for Research Associateship.
Authors contributions
MB conceived, designed, supervised, and commented on all drafts of this paper. BM, DP, PP, CS, SR, AS, NR and RK coordinated the animal study, conducted the overall experiments and participated in the data collection and analysis, molecular investigations and helped in the drafts. VM, SG, VKB, and MB contributed to data interpretation and manuscript completion.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was conducted as per the compliance of Committee for the Purpose of Control And Supervision of Experiments on Animals (CPCSEA) guidelines, Government of India.
Conflict of interest
The authors have no conflict of interest to disclose.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Balakumar, M., Prabhu, D., Sathishkumar, C. et al. Improvement in glucose tolerance and insulin sensitivity by probiotic strains of Indian gut origin in high-fat diet-fed C57BL/6J mice. Eur J Nutr 57, 279–295 (2018). https://doi.org/10.1007/s00394-016-1317-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-016-1317-7