Abstract
Background
Atrial fibrillation (AF) is a widespread type of sustained arrhythmia that poses significant health risks. Catheter ablation is the preferred treatment; however, arrhythmia recurrence remains challenging. Sodium-glucose co-transporter 2 inhibitors, particularly dapagliflozin (DAPA), have exhibited cardiovascular benefits. However, to date, the influence of these inhibitors on AF post-ablation remains unclear.
Methods
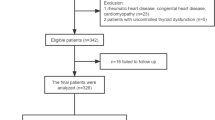
We analyzed the records of 272 patients who underwent catheter ablation for AF from January 2018 to December 2022. Patients were divided into the control (n = 199) and DAPA (n = 73) groups based on DAPA prescription post-ablation. The primary outcome was total atrial arrhythmia recurrence after a 3-month blanking period.
Results
The mean age was 72.19 ± 5.45 years; 86.8% of the patients were men. At 18 months post-ablation, 36.2% and 9.5% of the patients in the control and DAPA groups, respectively, reported atrial arrhythmia. Multivariate analysis revealed that DAPA use was associated with a significantly reduced risk of arrhythmia recurrence (adjusted hazard ratio [aHR]: 0.15, 95% confidence interval [CI]: 0.07–0.32, p < 0.001). After propensity score-matching (PSM) in 65 pairs, arrhythmia recurrence was lower in the DAPA group compared with the control (8.3% versus 30.8%, aHR: 0.17, 95% CI: 0.06–0.51, p = 0.002). Freedom from total arrhythmia recurrence was significantly higher in the DAPA group compared with the control group in both the overall and PSM population (log-rank test p < 0.01).
Conclusion
DAPA administration post-ablation was associated with significantly reduced atrial arrhythmia recurrence rates, indicating its potential as an adjunct therapy for enhancing the success of AF ablation.
Graphical abstract




Similar content being viewed by others
References
Chugh SS, Havmoeller R, Narayanan K et al (2014) Worldwide epidemiology of atrial fibrillation: a Global Burden of Disease 2010 Study. Circulation 129(8):837–847. https://doi.org/10.1161/CIRCULATIONAHA.113.005119
Andrade J, Khairy P, Dobrev D et al (2014) The clinical profile and pathophysiology of atrial fibrillation: relationships among clinical features, epidemiology, and mechanisms. Circ Res 114(9):1453–1468. https://doi.org/10.1161/CIRCRESAHA.114.303211
Calkins H, Hindricks G, Cappato R et al (2017) 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm 14(10):e275–e444. https://doi.org/10.1016/j.hrthm.2017.05.012
Zinman B, Wanner C, Lachin JM et al (2015) Empagliflozin, cardiovascular outcomes, and mortality in Type 2 diabetes. N Engl J Med 373(22):2117–2128. https://doi.org/10.1056/NEJMoa1504720
Wiviott SD, Raz I, Bonaca MP et al (2019) Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med 380(4):347–357. https://doi.org/10.1056/NEJMoa1812389
Zelniker TA, Wiviott SD, Raz I et al (2019) SGLT2 inhibitors for primary and secondary prevention of cardiovascular and renal outcomes in type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet 393(10166):31–39. https://doi.org/10.1016/S0140-6736(18)32590-X
Solomon SD, McMurray JJV, Claggett B et al (2022) Dapagliflozin in heart failure with mildly reduced or preserved ejection fraction. N Engl J Med 387(12):1089–1098. https://doi.org/10.1056/NEJMoa2206286
McMurray JJV, Solomon SD, Inzucchi SE et al (2019) Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 381(21):1995–2008. https://doi.org/10.1056/NEJMoa1911303
Fernandes GC, Fernandes A, Cardoso R et al (2021) Association of SGLT2 inhibitors with arrhythmias and sudden cardiac death in patients with type 2 diabetes or heart failure: a meta-analysis of 34 randomized controlled trials. Heart Rhythm 18(7):1098–1105. https://doi.org/10.1016/j.hrthm.2021.03.028
Qin T, Kong B, Dai C et al (2022) Protective effects of Dapagliflozin on the vulnerability of ventricular arrhythmia in rats with pulmonary artery hypertension induced by monocrotaline. Bioengineered 13(2):2697–2709. https://doi.org/10.1080/21655979.2021.2017652
Wu J, Liu T, Shi S et al (2022) Dapagliflozin reduces the vulnerability of rats with pulmonary arterial hypertension-induced right heart failure to ventricular arrhythmia by restoring calcium handling. Cardiovasc Diabetol 21(1):197. https://doi.org/10.1186/s12933-022-01614-5
Zelniker TA, Bonaca MP, Furtado RHM et al (2020) Effect of dapagliflozin on atrial fibrillation in patients with type 2 diabetes mellitus: insights from the DECLARE-TIMI 58 trial. Circulation 141(15):1227–1234. https://doi.org/10.1161/CIRCULATIONAHA.119.044183
Chan YH, Chao TF, Chen SW et al (2022) The risk of incident atrial fibrillation in patients with type 2 diabetes treated with sodium glucose cotransporter-2 inhibitors, glucagon-like peptide-1 receptor agonists, and dipeptidyl peptidase-4 inhibitors: a nationwide cohort study. Cardiovasc Diabetol 21(1):118. https://doi.org/10.1186/s12933-022-01549-x
Engström A, Wintzell V, Melbye M et al (2023) Sodium-glucose cotransporter 2 inhibitor treatment and risk of atrial fibrillation: Scandinavian cohort study. Diabetes Care 46(2):351–360. https://doi.org/10.2337/dc22-0714
Okunrintemi V, Mishriky BM, Powell JR et al (2021) Sodium-glucose co-transporter-2 inhibitors and atrial fibrillation in the cardiovascular and renal outcome trials. Diabetes Obes Metab 23(1):276–280. https://doi.org/10.1111/dom.14211
Zheng RJ, Wang Y, Tang JN et al (2022) Association of SGLT2 inhibitors with risk of atrial fibrillation and stroke in patients with and without type 2 diabetes: a systemic review and meta-analysis of randomized controlled trials. J Cardiovasc Pharmacol 79(2):e145–e152. https://doi.org/10.1097/FJC.0000000000001183
Fatima K, Suri A, Rija A et al (2023) The effect of sodium-glucose co-transporter 2 inhibitors on stroke and atrial fibrillation: a systematic review and meta-analysis. Curr Probl Cardiol 48(4):101582. https://doi.org/10.1016/j.cpcardiol.2022.101582
Luo F, Sun L, Wang Z et al (2022) Effect of dapagliflozin on the outcome of radiofrequency catheter ablation in patients with type 2 diabetes mellitus and atrial fibrillation. Cardiovasc Drugs Ther. https://doi.org/10.1007/s10557-022-07368-2
Abu-Qaoud MR, Kumar A, Tarun T et al (2023) Impact of SGLT2 inhibitors on atrial fibrillation recurrence after catheter ablation in patients with type-2-Diabetes. JACC Clin Electrophysiol 9(10):2109–2118. https://doi.org/10.1016/j.jacep.2023.06.008
Lahnwong S, Chattipakorn SC, Chattipakorn N (2018) Potential mechanisms responsible for cardioprotective effects of sodium-glucose co-transporter 2 inhibitors. Cardiovasc Diabetol 17(1):101. https://doi.org/10.1186/s12933-018-0745-5
Verma S, McMurray JJV, Cherney DZI (2017) The Metabolodiuretic promise of sodium-dependent glucose cotransporter 2 inhibition: the search for the sweet spot in heart failure. JAMA Cardiol 2(9):939–940. https://doi.org/10.1001/jamacardio.2017.1891
Neeland IJ, McGuire DK, Chilton R et al (2016) Empagliflozin reduces body weight and indices of adipose distribution in patients with type 2 diabetes mellitus. Diab Vasc Dis Res 13(2):119–126. https://doi.org/10.1177/1479164115616901
Lavie CJ, Pandey A, Lau DH et al (2017) Obesity and atrial fibrillation prevalence, pathogenesis, and prognosis: effects of weight loss and exercise. J Am Coll Cardiol 70(16):2022–2035. https://doi.org/10.1016/j.jacc.2017.09.002
Sun X, Han F, Lu Q et al (2020) Empagliflozin ameliorates obesity-related cardiac dysfunction by regulating Sestrin2-mediated AMPK-mTOR signaling and redox homeostasis in high-fat diet-induced obese mice. Diabetes 69(6):1292–1305. https://doi.org/10.2337/db19-0991
Sato T, Aizawa Y, Yuasa S et al (2020) The effect of dapagliflozin treatment on epicardial adipose tissue volume and P-wave indices: an ad-hoc analysis of the previous randomized clinical trial. J Atheroscler Thromb 27(12):1348–1358. https://doi.org/10.5551/jat.48009
Uthman L, Baartscheer A, Bleijlevens B et al (2018) Class effects of SGLT2 inhibitors in mouse cardiomyocytes and hearts: inhibition of Na(+)/H(+) exchanger, lowering of cytosolic Na(+) and vasodilation. Diabetologia 61(3):722–726. https://doi.org/10.1007/s00125-017-4509-7
Ye Y, Jia X, Bajaj M et al (2018) Dapagliflozin attenuates Na(+)/H(+) Exchanger-1 in cardiofibroblasts via AMPK activation. Cardiovasc Drugs Ther 32(6):553–558. https://doi.org/10.1007/s10557-018-6837-3
Funding
This study was supported by the VHS Medical Center Research Grant from the Republic of Korea (grant number VHSMC23021).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Noh, H.J., Cha, S.J., Kim, C.H. et al. Efficacy of dapagliflozin in improving arrhythmia-related outcomes after ablation for atrial fibrillation: a retrospective single-center study. Clin Res Cardiol 113, 924–932 (2024). https://doi.org/10.1007/s00392-024-02389-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00392-024-02389-3