Abstract
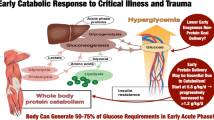
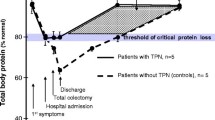
Discussion is continuing as to what constitutes optimal nutrition in the critically ill patient. According to the latest meta-analyses of currently available trials, there is agreement that the primary aim should be to initiate enteral nutrition as early as possible. It is still a matter of debate whether and when parenteral nutrition should be started in patients who cannot be appropriately fed by the enteral route. Recently, a grade B recommendation was given for parenteral nutrition in patients in whom enteral nutrition cannot be initiated within 24 hrs after admission to the intensive care unit or injury. Taking into account a caloric target of 24 kcal/kg BW/d the amount of substrates should not exceed: glucose 3 g/kg BW (serum glucose 110–120 mg%), lipids 0.8–1.2 g/kg BW (serum triglycerides <300 mg/dl) and amino acids 1–1.5 g/kg BW. There is high priority to avoid hyperglycemia and -triglyceridemia. Therefore, the caloric target has to be adapted according to substrate tolerance.
Zusammenfassung
In der Diskussion über die bestmögliche künstliche Ernährung des kritisch Kranken besteht auch nach den aktuellen Metaanalysen der verfügbaren Daten Konsens darüber, dass, wenn immer möglich, die enterale Zufuhr zu bevorzugen ist. Wann bei Patienten mit eingeschränkter enteraler Toleranz mit einer parenteralen Ernährung begonnen werden sollte, ist derzeit mangels entsprechender Studien offen. Es gibt jedoch die aktuelle Empfehlung (Grad B), bereits 24 h nach Aufnahme auf der Intensivstation oder nach Trauma mit der parenteralen Ernährung zu beginnen: Hierbei liegen die empfohlenen Zufuhrmengen bei 3–4 g Glukose/kg KG (Blutzuckerspiegel um 110–120 mg%), Lipide 0,8–1,2 g/kg KG (Serumtriglyzeride <300 mg/dl) und Aminosäuren 1–1,5 g/kg/KG. Angestrebt werden sollte eine Kalorienmenge von 24 kcal/kg und Tag. In der katabolen Flowphase gilt für die Vermeidung von Hyperglykämie und -triglyzeridämie höchste Priorität, so dass der Substrattoleranz entsprechend jederzeit das Unterschreiten des Kalorienziels einkalkuliert werden muss.
Similar content being viewed by others
Literatur
Dudrick SJ (2005) Rhoads Lecture: a 45-year obsession and passionate pursuit of optimal nutrition support: puppies, pediatrics, surgery, geriatrics, home TPN, A.S.P.E.N., et cetera. JPEN J Parenter Enteral Nutr 29:272–287
Gramlich L, Kichian K, Pinilla J, Rodych NJ, Dhaliwal R, Heyland DK (2004) Does enteral nutrition compared to parenteral nutrition result in better outcomes in critically ill adult patients? A systematic review of the literature. Nutrition 20:843–848
Peter JV, Moran JL, Philipps-Hughes J (2005) A metaanalysis of treatment outcomes of early enteral vs early parenteral nutrition in hospitalized patients. Crit Care Med 33:213–220
Heyland D, Dhaliwal R (2005) Early enteral nutrition vs early parenteral nutrition: an irrelevant question for the critically ill. Crit Care Med 33:260–261
Kreymann KG, Berger MM, Deutz NEP, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J (2006) ESPEN guidelines enteral nutrition: intensive care. Clin Nutr 25:210–223
Bistrian BR, Mc Cowen K (2006) Nutritional and metabolic support in the adult intensive care unit: key controversies. Crit Care Med 34:1525–1531
Koch T, Heller (2005) Auswirkungen einer parenteralen Ernährung nit n-3-Fettsäuren auf das Therapieergebnis–eine multizentrische Analyse von 661 Patienten. Aktuel Ernähr Med 30:15–20
Dhaliwal R, Jurewitsch B, Harrietha D, Heyland DK (2004) Combination enteral and parenteral nutrition in critically ill patients: harmful or beneficial? A systematic review of the evidence. Intensive Care Med 30:1666–1671
Simpson F, Doig GS (2005) Parenteral vs enteral nutrition in the critically ill patient: a meta-analysis of trials using the intention to treat principle. Intensive Care Med 31:12–23
Woodcock NP, Zeigler D, Palmer MD, Buckley P, Mitchell CJ, MacFie J (2001) Enteral vs parenteral nutrition: a pragmatic study. Nutrition 17:1–12
Barr J, Hecht M, Flavin KE, Khorana A, Gould MK (2004) Outcomes in critically ill patients before and after the implementation of an evidence-based nutritional management protocol. Chest 125:1446–1457
Petros S, Engelmann L (2006) Enteral nutrition delivery and energy expenditure in medical intensive care patients. Clin Nutr 25:51–59
Zaloga GP, Roberts PR, Marik P (2003) Feeding the hemodynamically unstable patient: a critical evaluation of the evidence. Nutr Clin Pract 18:285–293
Weimann A, Wirth Delia (2003) Probleme der künstlichen Ernährung–„Trouble Shooting“, Aktuel Ernähr Med 28:181–185
Van den Berghe G, Wouters P, Weekers F, Verwaest C, Bruyninckx F, Schetz M, Vlasselaers, D, Ferdinande P, Lauwers P, Bouillon R (2001) Intensive insulin therapy in the critically ill patients. N Engl J Med 345:1359–1367
Thorell A, Rooyackers O, Myrenfors P, Soop M, Nygren J, Ljungqvist OH (2004) Intensive insulin treatment in critically ill trauma patients normalizes glucose by reducing endogenous glucose production. J Clin Endocrinol Metab 89:5382–5386
Van den Berghe G, Wilmer A, Hermans G, Meerseman W, Wouters PJ, Milants I, Van Wijngaerden E, Bobbaers H, Bouillon R (2006) Intensive insulin therapy in the medical ICU. N Engl J Med 354:449–461
Pittas AG, Siegel RD, Lau J (2006) Insulin therapy and in-hospital mortality in critically ill patients: systematic review and meta-anaylsis of randomized controlled trials. JPEN J Parent Enteral Nutr 30:164–172
Vanhorebeek I, Langouche L, Berghe GV (2006) Intensive insulin therapy in the intensive care unit: update on clinical impact and mechanisms of action. Endocr Pract 12(Suppl 3):14–22
Siroen MP, van Leeuwen PA, Nijveldt RJ, Teerlink KT, Wouters PJ, Van den Berghe G (2005) Modulation of asymmetric dimetyhlarginine in critically ill patients receiving intensive insulin treatment: a possible explanation of reduced morbidity and mortality. Crit Care Med 33:504–510
Langouche L, Vanhorebeek I, Vlasselaers D, Vander Perre S, Wouters PJ, Skogstrand K, Hansen TK, Van den Berghe G (2005) Intensive insulin therapy protects the endothelium of critically ill patients. J Clin Invest 115:2277–2286
Nasraway SA (2006) Hyperglycemia during critical illness. JPEN J Parent Enteral Nutr 30:254–258
Brunkhorst FM, Werdan K (2006) Intensive care medicine: after positive studies questions occur. Dtsch Med Wochenschr 131:1441–1444
Dhaliwal R, Heyland DK (2005) Nutrition and infection in the intensive care unit: what does the evidence show? Curr Opin Crit Care 11:461–467
Battistella FD, Widergren JT, Anderson JT, Siepler JK, Weber JC, MacColl K (1997) A prospective, randomized trial of intravenous fat emulsion administration in trauma victims requiring total parenteral nutrition. J Trauma 43:52–58
Suchner U, Katz DP, Furst P, Beck K, Felbinger TW, Thiel M, Senftleben U, Goetz AE, Peter K (2002) Impact of sepsis, lung injury, and the the role of lipid infusion on circulating prostacyclin and thromboxane A(2). Intensive Care Med 28:122–129
Senkal M, Geier B, Hannemann M, Deska T, Linseisen J, Wolfram G, Adolph M (2007) Supplementation of Omega-3-fatty acids in total parenteral nutrition alters phospholipid fatty acid pattern. J Parent Enteral Nutr (JPEN) 31:12–17
Grimm H, Tibell A, Norrlind B, Blecher C, Wilker S, Schwemmle K (1994) Immunoregulation by parenteral lipids: impact of the n-3 to n-6-fatty acid ratio. JPEN J Parenter Enteral Nutr 18:417–421
Adolph M (2001) Lipid emulsions in total parenteral nutrition–state of the art and future perspectives. Clin Nutr 20(Suppl 4):11–14
Heller AR, Rössler S, Litz RJ, Stehr SN, Heller SC, Koch R, Koch T (2006) Omega-3-fatty acids improve the diagnosis-related clinical outcome. Crit Care Med 34:972–979
Shaw JHF, Wildbore M, Wolfe RR (1987) Whole body protein kinetics in severely septic patients. Ann Surg 205:288–294
Senftleben U, Felbinger T, Suchner U (1998) Pathophysiologie der Substratverwertung im Stressstoffwechsel: Bedeutung einer vollständigen hypoenergetischen Ernährungstherapie. Abt Ernähr Med 23:207–223
Weimann A, Ebener C, Holland-Cunz S, Jauch KW, Hausser L, Kemen M, Krähenbühl L, Kuse ER, Längle F (2007) Leitlinien Parenterale Ernährung Chirurgie und Transplantation, Akt Ernähr Med (in press)
Baines M, Shenkin A (2002) Lack of effectiveness of short-term intravenous micronutient nutrition in restoring plasma antioxidant status after surgery. Clin Nutr 21:145–150
Food and Drug Administration (FDA) (2000) Parenteral multivitamin products; drugs for human use; drug efficacy study implementation; amendment. Federal Register 65: 21200–21201
Heyland DK, Dhaliwal R, Suchner U, Berger MM (2005) Antioxidant nutrients: a systematic review of trace elements and vitamins in the critically ill patient. Intensive Care Med 31:327–337
Task Force for the Revision of Safe Practices for Parenteral Nutrition: Mirtallo J, Canada T, Johnson D, Kumpf V, Petersen C, Sacks G, Seres D, Guenter P (2004) Safe practices for parenteral nutrition. J Parent Enteral Nutr JPEN 29:S39–S70
Mühlhöfer A, Biesalski HK, Persson PB, Böhles HJ, Bischoff SC (2007) DGEM-Leitlinie. Parenterale Ernährung–Wasser, Elektrolyte, Vitamine und Spurenelemente. Aktuel Ernähr Med (in press)
Berger MM, Shenkin A (2006) Vitamins and trace elements: practical aspects of supplementation. Nutrition 22:952–955
Crimi E, Liguori, Condorelli M, Cioffi M, Astuto M, Bontempo P, Pignalosa O, Vietri MT, Molinari AM, Sica V, Della Corte F, Napoli C (2004) The beneficial effects of antioxidant supplenetation in enteral feeding in critically ill patients: a prospective randomized, double-blind, placebo-controlled trial. Anesth Analg 99:857–863
Heyland D, Dhaliwal R (2005) Immunonutrition in the critically ill: from old approaches to new paradigms. Intensive Care Med 31:501–503
Wernerman J (2005) Guidelines for nutritional support in intensive care unit patients: a critical analysis. Curr Opin Clin Nutr Metab Care 8:171–175
MacFie J (2004) European round table: the use of immunonutrition in the critically ill. Clin Nutr 23:1426–1429
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Weimann, A., Adolph, M. & Kreymann, G. Wieviel Ernährung braucht der Intensivpatient?. Intensivmed 44, 31–36 (2007). https://doi.org/10.1007/s00390-007-0770-1
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/s00390-007-0770-1