Abstract
Background
Up to 50% of patients with acute complicated diverticulitis require operative management on their index admission. There is ongoing debate as to whether primary anastomosis with diverting ileostomy versus a Hartmann’s procedure is the optimal surgical approach for these patients. This study aims to compare postoperative complications in patients undergoing either Hartmann’s procedure or primary anastomosis and diverting ileostomy for perforated diverticulitis using recent National Inpatient Sample data.
Methods
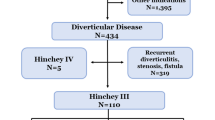
Patients who underwent either primary anastomosis with diverting ileostomy or Hartmann’s procedure for acute complicated diverticulitis from the 2015 to 2019 NIS database sample were included. Primary outcomes were postoperative in-hospital mortality and morbidity. Secondary outcomes were postoperative cause-specific complications, total admission cost, and length of stay (LOS). Univariate and multivariate regression were utilized to compare the two operative approaches.
Results
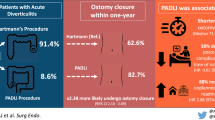
Overall, 642 patients underwent primary anastomosis with diverting ileostomy and 4,482 patients underwent Hartmann’s procedure. There was no difference in in-hospital mortality (OR 0.93, 95%CI 0.45–1.92, p = 0.84) or in-hospital morbidity (OR 1.10, 95%CI 0.90–1.35, p = 0.33). Adjusted analysis suggested shorter postoperative LOS for patients undergoing Hartmann’s procedure (MD 0.79 days, 95%CI 0.15–1.43 days, p = 0.013) and decreased total admission cost (MD $4,893.99, 95%CI $1,425.04-$8,362.94, p = 0.006).
Conclusions
The present study supports that primary anastomosis with diverting ileostomy is safe for properly selected patients presenting with complicated diverticulitis. Primary anastomosis with diverting ileostomy is associated with greater total hospitalization costs and LOS.
Similar content being viewed by others
Data availability
The data used in the current study is available upon request.
References
Tursi A, Scarpignato C, Strate LL et al (2020) Colonic diverticular disease. Nat Rev Dis Primers 2020 6:1 6:1–23. https://doi.org/10.1038/s41572-020-0153-5
Tursi A (2016) Diverticulosis today: unfashionable and still under-researched. Therap Adv Gastroenterol 9:213. https://doi.org/10.1177/1756283X15621228
Bollom A, Austrie J, Hirsch W et al (2017) Emergency Department Burden of Diverticulitis in the United States, 2006 to 2013. Dig Dis Sci 62:2694. https://doi.org/10.1007/S10620-017-4525-Y
Shahedi K, Fuller G, Bolus R et al (2013) Long-term Risk of Acute Diverticulitis Among Patients With Incidental Diverticulosis Found During Colonoscopy. Clin Gastroenterol Hepatol 11:1609. https://doi.org/10.1016/J.CGH.2013.06.020
von Strauss Und Torney M, Moffa G, Kaech M et al (2020) Risk of Emergency Surgery or Death After Initial Nonoperative Management of Complicated Diverticulitis in Scotland and Switzerland. JAMA Surg 155:600–606. https://doi.org/10.1001/JAMASURG.2020.0757
Bharucha AE, Parthasarathy G, Ditah I et al (2015) Temporal Trends in the Incidence and Natural History of Diverticulitis: A Population-Based Study. Am J Gastroenterol 110:1589. https://doi.org/10.1038/AJG.2015.302
Oberkofler CE, Rickenbacher A, Raptis DA et al (2012) A multicenter randomized clinical trial of primary anastomosis or Hartmann’s procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg 256:819–827. https://doi.org/10.1097/SLA.0B013E31827324BA
Nunes GC, Robnett AH, Kremer RM, Ahlquist RE (1979) The Hartmann Procedure for Complications of Diverticulitis. Arch Surg 114:425–429. https://doi.org/10.1001/ARCHSURG.1979.01370280079011
Hallam S, Mothe BS, Tirumulaju RMR (2018) Hartmann’s procedure, reversal and rate of stoma-free survival. Ann R Coll Surg Engl 100:301. https://doi.org/10.1308/RCSANN.2018.0006
Bridoux V, Regimbeau JM, Ouaissi M et al (2017) Hartmann’s Procedure or Primary Anastomosis for Generalized Peritonitis due to Perforated Diverticulitis: A Prospective Multicenter Randomized Trial (DIVERTI). J Am Coll Surg 225:798–805. https://doi.org/10.1016/J.JAMCOLLSURG.2017.09.004
Lambrichts DPV, Vennix S, Musters GD et al (2019) Hartmann’s procedure versus sigmoidectomy with primary anastomosis for perforated diverticulitis with purulent or faecal peritonitis (LADIES): a multicentre, parallel-group, randomised, open-label, superiority trial. Lancet Gastroenterol Hepatol 4:599–610. https://doi.org/10.1016/S2468-1253(19)30174-8
Lee JM, Chang BP, J, el Hechi M et al (2019) Hartmann’s Procedure vs Primary Anastomosis with Diverting Loop Ileostomy for Acute Diverticulitis: Nationwide Analysis of 2,729 Emergency Surgery Patients. J Am Coll Surg 229:48–55. https://doi.org/10.1016/J.JAMCOLLSURG.2019.03.007
Goldstone RN, Cauley CE, Chang DC et al (2019) The Effect of Surgical Training and Operative Approach on Outcomes in Acute Diverticulitis: Should Guidelines Be Revised? Dis Colon Rectum 62:71–78. https://doi.org/10.1097/DCR.0000000000001240
Cauley CE, Patel R, Bordeianou L (2018) Use of primary anastomosis with diverting ileostomy in patients with acute diverticulitis requiring urgent operative intervention. Dis Colon Rectum 61:586–592. https://doi.org/10.1097/DCR.0000000000001080
Tadlock MD, Karamanos E, Skiada D et al (2013) Emergency surgery for acute diverticulitis: Which operation? A national surgical quality improvement program study. J Trauma Acute Care Surg 74:1385–1391. https://doi.org/10.1097/TA.0B013E3182924A82
HCUP-US NIS Overview. https://www.hcup-us.ahrq.gov/nisoverview.jsp. Accessed 28 Oct 2022
Wei D, Johnston S, Goldstein L, Nagle D (2019) Minimally invasive colectomy is associated with reduced risk of anastomotic leak and other major perioperative complications and reduced hospital resource utilization as compared with open surgery: a retrospective population-based study of comparative effectiveness and trends of surgical approach. Surg Endosc 34(2):610–621. https://doi.org/10.1007/S00464-019-06805-Y
Kang CY, Halabi WJ, Chaudhry OO et al (2013) Risk Factors for Anastomotic Leakage After Anterior Resection for Rectal Cancer. JAMA Surg 148:65–71. https://doi.org/10.1001/2013.JAMASURG.2
Gawlick U, Nirula R (2012) Resection and primary anastomosis with proximal diversion instead of Hartmann’s: evolving the management of diverticulitis using NSQIP data. J Trauma Acute Care Surg 72:807–814. https://doi.org/10.1097/TA.0B013E31824EF90B
Binda GA, Karas JR, Serventi A et al (2012) Primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a prematurely terminated randomized controlled trial. Colorectal Dis 14:1403–1410. https://doi.org/10.1111/J.1463-1318.2012.03117.X
Hall J, Hardiman K, Lee S et al (2020) The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Left-Sided Colonic Diverticulitis. Dis Colon Rectum 63:728–747. https://doi.org/10.1097/DCR.0000000000001679
Sartelli M, Weber DG, Kluger Y et al (2020) 2020 update of the WSES guidelines for the management of acute colonic diverticulitis in the emergency setting. World J Emergency Surg 15:1–18. https://doi.org/10.1186/S13017-020-00313-4
Epstein AM (1995) US Teaching Hospitals in the Evolving Health Care System. JAMA 273:1203–1207. https://doi.org/10.1001/JAMA.1995.03520390063034
Onald D, Aylor HT, Avid D et al (1999) Effects of Admission to a Teaching Hospital on the Cost and Quality of Care for Medicare Beneficiaries. 340:293–299. https://doi.org/10.1056/NEJM199901283400408
Khuri SF, Najjar SF, Daley J et al (2001) Comparison of surgical outcomes between teaching and nonteaching hospitals in the Department of Veterans Affairs. Ann Surg 234:370–383. https://doi.org/10.1097/00000658-200109000-00011
Sutton E, Miyagaki H, Bellini G et al (2017) Risk factors for superficial surgical site infection after elective rectal cancer resection: a multivariate analysis of 8880 patients from the American College of Surgeons National Surgical Quality Improvement Program database. J Surg Res 207:205–214. https://doi.org/10.1016/J.JSS.2016.08.082
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Yung Lee and Tyler McKechnie. The first draft of the manuscript was written by Yung Lee, and Tyler McKechnie. Yasith Samarasinghe prepared Tables 1, 2, 3 and 4 and Appendix 1, and all authors edited and commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, Y., McKechnie, T., Samarasinghe, Y. et al. Primary anastomosis with diverting loop ileostomy versus Hartmann’s procedure for acute complicated diverticulitis: analysis of the National Inpatient Sample 2015–2019. Int J Colorectal Dis 38, 156 (2023). https://doi.org/10.1007/s00384-023-04452-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s00384-023-04452-3