Abstract
Background
Surgical resection is the mainstay of curative treatment for rectal cancer. Post-operative complications, low anterior resection syndrome (LARS), and the presence of a stoma may influence the quality of life after surgery. This study aimed to gain more insights into the long-term trade-off between stoma and anastomosis.
Methods
All patients who underwent sphincter-sparing surgical resection for rectal cancer in the Leiden University Medical Center and the Reinier de Graaf Gasthuis between January 2012 and January 2016 were included. Patients received the following questionnaires: EORTC-QLQ-CR29, EORTC-QLQ-C30, EQ-5D-5L, and the LARS score. A comparison was made between patients with a stoma and without a stoma after follow-up.
Results
Some 210 patients were included of which 149 returned the questionnaires (70.9%), after a mean follow-up of 3.69 years. Overall quality of life was not significantly different in patients with and without stoma after follow-up using the EORTC-QLQ-C30 (p = 0.15) or EQ-5D-5L (p = 0.28). However, after multivariate analysis, a significant difference was found for the presence of a stoma on global health status (p = 0.01) and physical functioning (p < 0.01). Additionally, there was no difference detected in the quality of life between patients with major LARS or a stoma.
Conclusion
This study shows that after correction for possible confounders, a stoma is associated with lower global health status and physical functioning. However, no differences were found in health-related quality of life between patients with major LARS and patients with a stoma. This suggests that the choice between stoma and anastomosis is mainly preferential and that shared decision-making is required.
Similar content being viewed by others
Introduction
With an estimated 704,000 new patients worldwide each year, rectal cancer has become the eighth most diagnosed cancer type in the world in 2018 [1]. Approximately 3,300 new patients are diagnosed with rectal cancer in the Netherlands every year [2]. Of these patients, 63.6% receive a (temporary) stoma [3]. Nowadays, the treatment of rectal cancer is adopting a more multimodal approach, but surgical resection is still the cornerstone of curative treatment [4]. Over the past decades, the 5-year survival has gone up to 75–80% [5]. The increased survival over the past decades and enlarged focus on value-based healthcare account for the growing interest in the quality of life after cancer treatment [6,7,8]. An example is the shift from abdominoperineal excision (APE) to sphincter-sparing techniques with low anastomosis in order to maintain organ preservation and bowel continence [9]. The ongoing upswing in overall survival after rectal cancer surgery brings about new dilemmas such as stoma presence, bowel dysfunction, and psychological and physical stress [10, 11].
After rectal cancer resection, surgeons are left with the decision on how to reconstruct. Should an anastomosis be constructed with or without a defunctioning stoma or should a definitive stoma be made? For this choice, two considerations are key: first of all, the risk of anastomotic leakage, its consequences, and whether a patient is able to cope with them [12]. An anastomotic leak can be a fatal insult to a frail patient. The other important consideration is the risk of a poor functional outcome. Approximately 41% of patients without a stoma after a sphincter-sparing surgical resection for rectal cancer experience major low anterior resection syndrome (LARS) 1 year after surgery [13]. LARS is described as a “disorder of bowel function after rectal resection, leading to a detriment in quality of life” [14, 15]. Frequently (≥ 35%) reported symptoms are clustering of bowel movement, incomplete evacuation, fecal incontinence, uncontrollable flatus, and urgency [16]. LARS has been shown to have a detrimental influence on short- and long-term health-related quality of life [17, 18]. Factors that have a negative impact on functional outcomes after rectal resection are low anastomosis, temporary stoma, or a stoma before surgery and (neo-)adjuvant radiotherapy. A definitive stoma may prevent these adverse functional outcomes. However, also, stoma-related complications such as parastomal hernia, retraction, prolapse, and stoma necrosis must be considered [19, 20]. This also goes for temporary stoma’s as they can significantly increase mid- to long-term morbidity and cause readmissions and re-interventions. Furthermore, up to 28.5% of temporary stomas are never reversed [21].
Post-operative complications, poor functional outcomes, and the presence of a stoma in patients may all influence the quality of life after surgery, making the decision between the formation of a (temporary) stoma or anastomosis a difficult one [22]. This decision should always be made together with the patient. Information on quality of life after rectal cancer surgery is vital for shared decision-making [23]. This study aims to determine the influence of a stoma on the health-related quality of life (HRQoL) after rectal cancer surgery and gain more insights into the trade-offs between stoma and anastomosis on the long run. In addition, the difference in HRQoL between patients with major LARS and a stoma is analyzed, using patient-reported outcome measures (PROMs).
Methods
Study population and treatment
The Medical Ethics Committee Leiden Den Haag Delft assessed this study protocol and concluded no formal review was needed, as this study is not being conducted under the Medical Research Involving Human Subjects Act (WMO). Consecutive patients who underwent surgical resection for rectal cancer in the Leiden University Medical Center, Leiden, The Netherlands, and the Reinier de Graaf Gasthuis, Delft, The Netherlands, between January 2012 and January 2016 with at least 1.5-year follow-up were reviewed for the current study. All patients signed an informed consent form before a review of their medical records and sending questionnaires. Patients that gave informed consent but did not return the questionnaires were called at least twice. These patients were excluded from the analyses, but their characteristics were included in Online Resource 1. Inclusion criteria were patients with a primary tumor of stages I–III located in the rectosigmoid and rectum treated with surgical resection. Patients who underwent emergency surgery, palliative intended surgery, or who were treated with an APE were excluded. Additionally, patients with < 90% completed questionnaires were excluded. Data regarding 30-day morbidity and mortality were extracted from the Dutch ColoRectal Audit (DCRA), a nationwide clinical audit [24]. The remaining data were extracted from the electronic patient record.
Baseline characteristics and outcomes
Distance from anus was measured during colonoscopy. Short-term endpoints were 90-day major complications, readmissions, and reinterventions. Major complications were defined according to the Clavien-Dindo classification as ≥ IIIa [25]. The HRQoL of patients was assessed as the primary outcome. Secondary outcomes at 1 and 2 years after surgery were unplanned re-admissions and re-interventions after the initial 30-day postoperative period.
Health-related quality of life assessment
After at least 1.5 years of follow-up, patients were asked to fill in the HRQoL questionnaires (EORTC QLQ-CR29, EORTC QLQ-C30, and EQ-5D-5L) [26,27,28]. In all questionnaires, a 4-point Likert scale was used, and subsequently, all responses were linearly converted to 0–100 scales.
Statistical analyses
The statistical analysis was performed with SPSS Statistics version 24. Patients were divided into two groups, patients who had a stoma at the time of follow-up and patients without a stoma at the time of follow-up. Chi-square test was used for categorical variables; the Mann–Whitney U test was used for numeric variables. Multivariate analysis using the linear regression was performed to correct for possible confounding with correction for Charlson comorbidity index and tumor recurrence. For sub-analysis, the population was divided into a group with major LARS and a group of patients with a stoma. After using the EQ-5D-5L questionnaire, a crosstab was made. The p-value of the VAS score was calculated using the Mann–Whitney U test. The p-values of mobility, self-care, usual activity, pain, and anxiety were calculated with Pearson’s chi squared test. A p-value of 0.05 was considered statistically significant. In line with current evidence, a HRQoL score difference of > 5% was considered clinically significant [29]. Outcomes were assumed significant if both statistically and clinically significant.
Results
Patient characteristics
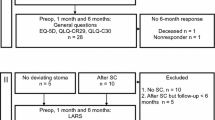
A total of 254 patients were eligible for the study, of which 44 (17.3%) refused to participate. Of the 210 patients that provided informed consent 149 (70.9%) filled out the questionnaires after a mean follow-up of 3.69 (range: 1–8) years (Fig. 1). The 61 patients (29.1%) that did consent to take part in the study but did not return the questionnaires were on average older in both the stoma and no stoma groups; other patient characteristics were comparable with those of patients that have returned the questionnaires (Online Resource 1). At the time of follow-up, 23 included patients (15.4%) had a stoma, of which 20 were a colostoma. In total, 103 (69.1%) patients underwent a low anterior resection (LAR) with primary anastomosis, 30 (20.1%) a LAR with a defunctioning stoma, and 16 (10.7%) a Hartmann resection (Table 1). In 46 patients (30.9%), a stoma was constructed during primary surgery and 9 (6.0%) in patients during a reintervention. Thirty-two patients (21.4%) had a temporary stoma, of which 2 were closed more than a year after surgery. Patients who still had a stoma at the time of follow-up were older (p = 0.03), had a lower tumor (p = < 0.01), received more frequent neoadjuvant therapy (p = 0.03), and had more major postoperative complications (p = 0.03). Patients with a stoma had significantly more unplanned readmissions in both the first (p < 0.01) and the second year of follow-up (p = 0.03) (Table 2). Moreover, significantly more unplanned reinterventions were performed in the stoma group in both the first (p < 0.01) and second years (p < 0.01) of follow-up.
Health-related quality of life
The overall quality of life more than 2 years after surgery was not significantly different between patients with and without a stoma, not in the EQ-5D-5L (p = 0.28) nor in the EORTC-QLQ-C30 (p = 0.15) (Fig. 2; Online Resource 2; Online Resource 4). However, patients with a stoma reported significantly lower physical functioning (p = 0.03), significantly more problems with self-care (p = 0.03), and usual activity (p = < 0.01). Moreover, patients who received a stoma had significantly more complaints of nausea and vomiting (p = 0.02), dry mouth (p = 0.03), hair loss (p = 0.02), sore skin (p < 0.01), impotence (p = 0.01), and lower body image (p = 0.03) (Fig. 2; Online Resource 3). Additionally, patients with a stoma reported more financial difficulties (p = 0.02).
Patient reported outcomes (PROMs). A EORTC-QLQ-C30, comparison between patients with stoma (red) and patients without stoma (blue) at follow-up. B Patient reported outcomes (PROMs) using EORTC-QLQ-CR29, comparison between patients with stoma and patients without stoma at follow up. C EORTC-QLQ-C30, comparison between patients with stoma (red), patients major low anterior resection syndrome (LARS) (blue) and control patients, without a stoma or major LARS (yellow) at follow up. D EORTC-QLQ-CR29, comparison between patients with stoma and patients major low anterior resection syndrome (LARS) control patients, without a stoma or major LARS (yellow) at follow-up. *p-value < 0.05
In a multivariate analysis, a stoma present at follow-up was associated with a lower global health status (RR: 0.93, 95%CI 0.88–0.99, p = 0.04) and physical functioning (RR: 0.91, 95CI% 0.86–0.96, p < 0.01) (Table S5, S6). Also, a higher cT score (RR: 0.97, 95%CI 0.95–0.99, p < 0.01) and neoadjuvant chemoradiotherapy (RR: 0.94, 95%CI 0.98–0.99, p = 0.02) were associated with a lower global health status (Online Resource 5).
Male sex (RR: 0.95, 95%CI 0.92–0.99, p = 0.01), higher ASA score (RR: 0.92, 95%CI 0.89–0.96, p < 0.01), a higher cN score (RR: 0.97, 95%CI 0.95–0.99, p = 0.01), and Hartmann procedure (RR: 0.90, 95%CI 0.84–0.96, p < 0.01) were significantly associated with a lower reported physical functioning (Online Resource 6).
Major-LARS and health-related quality of life
A sub-analysis was done for patients that did not have a stoma at follow-up and reported major-LARS (n = 30, 23.8%). No difference was found in global health status between major LARS patients and patients with a stoma (p = 0.50). Furthermore, no significant difference was found for any of the five functioning scales of the EORTC-QLQ-C30 (Fig. 2; Online Resource 7). Within the EORTC-QLQ-CR29, major-LARS patients reported more problems with flatulence (p = < 0.01) and stool frequency (p = 0.03) (Fig. 2; Online Resource 8). Moreover, patients with a major-LARS had more complaints of embarrassment compared to patients with a stoma (p = 0.02).
Discussion
This study evaluated the HRQoL in patients with an anastomosis or a stoma 2 years or more after sphincter-sparing rectal resection for cancer. It shows that postoperative global health status and physical functioning are negatively associated with the presence of a stoma in these patients after adjusting for possible cofounders (Charlson comorbidity index, tumor recurrence). In contrast, no clinically significant differences in HRQoL were found between patients with a stoma and patients with an anastomosis and major LARS. Patients with major LARS had more complaints of embarrassment than patients with a stoma. Patients with a stoma had a significantly higher unplanned readmission and reintervention rate in the first 2 years after surgery.
Earlier studies showed ambiguous results for the influence of a stoma on HRQoL. A Cochrane review found that out of the 26 studies included, only 10 reported significantly poorer HRQoL in patients with a permanent stoma [30]. Therefore, the authors concluded their study did not allow for firm conclusions about whether patients with or without permanent colostoma have a superior HRQoL after rectal cancer surgery. One explanation for a reduced quality of life with a stoma can be stoma-related problems. Vonk-Klaasen et al. demonstrated in their systematic review that stoma-related problems, defined as sexual problems, feeling depressed, constipation, body image, difficulties while traveling, and worry about stoma noises, lead to a lower HRQoL [22]. Furthermore, differences in body image were observed, which were most likely caused by the presence of a stoma. In addition, significantly more male patients with a stoma complained about impotence. It should be noted here that the patients with a stoma were significantly older and that some patients were not sexually active anymore at time of surgery. Some of the above reported differences may therefore be at least partly due to the influence of age.
When comparing patients with poor functional outcomes and patients with a stoma, this study did not show differences in HRQoL. Most studies on HRQoL of patients with major LARS only compared patients with and without major-LARS. These studies agree that major LARS is associated with a decreased HRQoL [14, 15, 31, 32]. However, also, patient and treatment characteristics (e.g., age, radiotherapy, low anastomosis) of patients that develop major LARS are likely to influence HRQoL [31, 33]. In this study, patients with major LARS had significantly more complaints of embarrassment than patients with a stoma, which can be an important issue to discuss with a patient when a high risk of major LARS is anticipated. The Pre-Operative LARS score (POLARS) can be used to make an estimation of LARS score to predict the postoperative functional outcome [34].
The current study showed that patients with a stoma had significantly more readmissions and reinterventions. These results are in line with current literature [19, 35]. Additionally, stoma-related complications (e.g., bulge, peristomal hernia) were shown to be associated with a decrease in HRQoL, which could have impacted the results of this study [19, 36]. The increased number of readmissions and reinterventions in patients with a stoma as well as stoma-related complications are also relevant in the tradeoff between a stoma and an anastomosis.
A factor that should be taken into account when comparing different studies on quality of life after rectal cancer surgery is the timing of measuring PROMs [37]. Compared to the population norm, HRQoL improves 3 to 6 months after surgery with patients reaching role-, physical-, and emotional functioning [38, 39]. Studies suggest that HRQoL improvement during this period is caused by fewer defecation or stoma-related complaints, as well as the reversal of temporary stomas, which possibly contributes to this positive effect [39,40,41]. Furthermore, the age of patients might be an important factor in HRQoL studies after rectal cancer surgery. Recent studies have shown that younger patients (< 65 years) are more affected in their quality of life than elderly patients [38, 39]. Several other studies have shown that the overall quality of life in colorectal cancer survivors is comparable to that of the population norms, suggesting that cancer survivors are very resilient and cope well with their treatment [38, 39, 42]. Colorectal cancer survivors have persisting concerns, such as having to adapt to living with a stoma, these concerns consist of clothing difficulties, dietary changes, and bowel functioning [43]. How well patients cope with these problems hugely influences their quality of life and should be considered regarding PROMs. Additionally, comparison of patients with an anastomosis or a stoma may be troubled by confounding by indication; i.e., the choice for a stoma is influenced by the (perceived) risk of adverse postoperative outcomes. In this study, this is reflected by the fact that patients with a stoma had a more advanced age, lower tumor location, and received more neoadjuvant therapy. In general, advancing age goes hand in hand with a declining HRQoL [44]. This preoperative patient selection and the subsequent difference in patient characteristics and treatment decisions are inevitable in retrospective HRQoL research.
As stated, the decision between an anastomosis and a (temporary) stoma after sphincter-sparing rectal cancer surgery is motivated by the risk of adverse events (e.g., anastomotic leakage) and the expected functional outcomes [12, 33, 45]. However, since this decision is usually not a straightforward one, caused by the lack of a clinically “best choice,” considering the risks of poor functional outcome makes this decision preference-sensitive and therefore particularly relevant for shared decision-making [34, 46, 47]. The presented HRQoL effects of a stoma and major LARS in this study might provide information that can be used as patient information to assist in shared decision-making. Furthermore, explicit patient consideration of the trade-off between anastomosis or a stoma might positively influence the long-term quality of life and lead to a higher acceptance of possible consequences [48].
Limitations
The fact that this study excluded all patients that underwent an APE could be scrutinized. However, with a classic APE, there is no decision to be made between a stoma or an anastomosis, as the latter is not an option. Furthermore, APE patients typically have lower rectal tumors with invasion of the sphincter complex or sphincter insufficiency, which is associated with typical and worse pre-operative symptoms [35, 49]. Nonetheless, patients could have been excluded that had intersphincteric APEs as an alternative for a Hartmann. In these patients, the same considerations about an anastomosis or a stoma could have been made, but surgeons could have been reluctant to leave the rectal stump. The decision whether to perform an APE as an alternative to a low Hartmann is an ongoing debate; the main reason this is done is to avoid the risk of staple line rupture and subsequent leakage and pelvic abscesses as well as persisting mucus production and diversion proctitis [50, 51]. However, an APE is associated with additional risks of perineal wound complications [52]. In our hospitals, the rectal stump is typically left in place except in very low resections. Another limitation of this study was the small sample size, especially in the stoma group. The latter could have been consequential to the exclusion of APE patients as mentioned above and stoma reversal before follow-up and answering the PROM questionnaires. An additional limitation is that the sample size did not allow for sub-analysis of patients with an ileostoma and a colostoma or stoma formation during primary surgery and stoma formation during reintervention. Furthermore, a limitation is the variation in follow-up. In this study, we included all patients operated from 2012 until 2016. The follow-up and time of receiving the questionnaires after operation varied between 2 and 7 years. However, to our knowledge, this is the first study to make a comparison of long-term HRQoL between patients with a stoma and major LARS.
Conclusion
This study shows that after correction for possible confounders, a stoma is associated with a lower global health status and physical functioning. However, no clinically significant difference was found in HRQoL between patients with major LARS and patients with a stoma. This suggests that the choice between stoma and anastomosis is mainly preferential and should be made together with the patient. This study offers leads for improved patient information and enhanced shared decision-making before rectal cancer surgery.
References
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
IKNL Incidentie darmkanker (2022) Available from: https://iknl.nl/kankersoorten/darmkanker/registratie/incidentie
Annual report Dutch Colorectal Cancer Audit (2019) Available from: https://dica.nl/jaarrapportage-2019/Dcra
Bahadoer RR et al (2021) Short-course radiotherapy followed by chemotherapy before total mesorectal excision (TME) versus preoperative chemoradiotherapy, TME, and optional adjuvant chemotherapy in locally advanced rectal cancer (RAPIDO): a randomised, open-label, phase 3 trial. Lancet Oncol 22(1):29–42
Creavin B et al (2021) Oncological outcomes of laparoscopic versus open rectal cancer resections: meta-analysis of randomized clinical trials. Br J Surg 108(5):469–476
Becker N, Muscat JE, Wynder EL (2001) Cancer mortality in the United States and Germany. J Cancer Res Clin Oncol 127(5):293–300
Greenlee RT et al (2001) Cancer statistics, 2001. CA Cancer J Clin 51(1):15–36
Weir HK et al (2003) Annual report to the nation on the status of cancer, 1975–2000, featuring the uses of surveillance data for cancer prevention and control. J Natl Cancer Inst 95(17):1276–1299
Ricciardi R et al (2007) The status of radical proctectomy and sphincter-sparing surgery in the United States. Dis Colon Rectum 50(8):p. 1119–27, discussion 1126–7
Jehle EC et al (1995) Level of the anastomosis does not influence functional outcome after anterior rectal resection for rectal cancer. Am J Surg 169(1):p. 147–52, discussion 152–3
Påhlman L (2001) The rectal cancer debate. Eur J Surg Oncol 27(5):439
Tan WS et al (2009) Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg 96(5):462–472
Croese AD et al (2018) A meta-analysis of the prevalence of low anterior resection syndrome and systematic review of risk factors. Int J Surg 56:234–241
Keane C et al (2017) Defining low anterior resection syndrome: a systematic review of the literature. Colorectal Dis 19(8):713–722
Bryant CL et al (2012) Anterior resection syndrome. Lancet Oncol 13(9):e403–e408
Scheer AS et al (2011) The long-term gastrointestinal functional outcomes following curative anterior resection in adults with rectal cancer: a systematic review and meta-analysis. Dis Colon Rectum 54(12):1589–1597
Pieniowski EHA et al (2019) Low anterior resection syndrome and quality of life after sphincter-sparing rectal cancer surgery: a long-term longitudinal follow-up. Dis Colon Rectum 62(1):14–20
Chen TY et al (2015) Bowel function 14 years after preoperative short-course radiotherapy and total mesorectal excision for rectal cancer: report of a multicenter randomized trial. Clin Colorectal Cancer 14(2):106–114
Näsvall P et al (2017) Quality of life in patients with a permanent stoma after rectal cancer surgery. Qual Life Res 26(1):55–64
Ihnát P et al (2016) Diverting ileostomy in laparoscopic rectal cancer surgery: high price of protection. Surg Endosc 30(11):4809–4816
Kuryba AJ et al (2016) Determinants of stoma reversal in rectal cancer patients who had an anterior resection between 2009 and 2012 in the English National Health Service. Colorectal Dis 18(6):O199-205
Vonk-Klaassen SM et al (2016) Ostomy-related problems and their impact on quality of life of colorectal cancer ostomates: a systematic review. Qual Life Res 25(1):125–133
van der Valk MJM et al (2020) Importance of patient reported and clinical outcomes for patients with locally advanced rectal cancer and their treating physicians. Do clinicians know what patients want? Eur J Surg Oncol 46(9):1634–1641
Van Leersum NJ et al (2013) The Dutch surgical colorectal audit. Eur J Surg Oncol 39(10):1063–1070
Clavien PA et al (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250(2):187–196
Aaronson NK et al (1993) The European Organization for Research and Treatment of Cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 85(5):365–376
EuroQol (1990) A new facility for the measurement of health-related quality of life. Health Policy 16(3):199–208
Whistance RN et al (2009) Clinical and psychometric validation of the EORTC QLQ-CR29 questionnaire module to assess health-related quality of life in patients with colorectal cancer. Eur J Cancer 45(17):3017–3026
Ringash J et al (2007) Interpreting clinically significant changes in patient-reported outcomes. Cancer 110(1):196–202
Pachler J, Wille-Jørgensen P (2005) Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev (2):Cd004323
Ketelaers SHJ et al (2022) Functional bowel complaints and the impact on quality of life after colorectal cancer surgery in the elderly. Front Oncol
Emmertsen KJ, Laurberg S (2013) Impact of bowel dysfunction on quality of life after sphincter-preserving resection for rectal cancer. Br J Surg 100(10):1377–1387
Benli S, Çolak T, Türkmenoğlu M (2021) Factors influencing anterior/low anterior resection syndrome after rectal or sigmoid resections. Turk J Med Sci 51(2):623–630
Battersby NJ et al (2018) Development and external validation of a nomogram and online tool to predict bowel dysfunction following restorative rectal cancer resection: the POLARS score. Gut 67(4):688–696
Monastyrska E et al (2016) Prospective assessment of the quality of life in patients treated surgically for rectal cancer with lower anterior resection and abdominoperineal resection. Eur J Surg Oncol 42(11):1647–1653
Blok RD et al (2018) Impact of an institutional change from routine to highly selective diversion of a low anastomosis after TME for rectal cancer. Eur J Surg Oncol 44(8):1220–1225
Chambers SK et al (2012) A five-year prospective study of quality of life after colorectal cancer. Qual Life Res 21(9):1551–1564
Arndt V et al (2004) Quality of life in patients with colorectal cancer 1 year after diagnosis compared with the general population: a population-based study. J Clin Oncol 22(23):4829–4836
Wilson TR, Alexander DJ (2008) Clinical and non-clinical factors influencing postoperative health-related quality of life in patients with colorectal cancer. Br J Surg 95(11):1408–1415
Camilleri-Brennan J, Steele RJ (2002) Prospective analysis of quality of life after reversal of a defunctioning loop ileostomy. Colorectal Dis 4(3):167–171
Engel J et al (2003) Quality of life in rectal cancer patients: a four-year prospective study. Ann Surg 238(2):203–213
Jansen L et al (2010) Quality of life among long-term (≥5 years) colorectal cancer survivors–systematic review. Eur J Cancer 46(16):2879–2888
Sun V et al (2013) Surviving colorectal cancer: long-term, persistent ostomy-specific concerns and adaptations. J Wound Ostomy Continence Nurs 40(1):61–72
Kind P et al (1998) Variations in population health status: results from a United Kingdom national questionnaire survey. BMJ 316(7133):736–741
van Kooten RT et al (2021) Preoperative risk factors for major postoperative complications after complex gastrointestinal cancer surgery: a systematic review. Eur J Surg Oncol 47(12):3049–3058
Stiggelbout AM et al (2012) Shared decision making: really putting patients at the centre of healthcare. BMJ 344:e256
Ivatury SJ, Durand MA, Elwyn G (2019) Shared decision-making for rectal cancer treatment: a path forward. Dis Colon Rectum 62(12):1412–1413
Pieterse AH et al (2019) Patient explicit consideration of tradeoffs in decision making about rectal cancer treatment: benefits for decision process and quality of life. Acta Oncol 58(7):1069–1076
Konanz J et al (2013) Quality of life of patients after low anterior, intersphincteric, and abdominoperineal resection for rectal cancer—a matched-pair analysis. Int J Colorectal Dis 28(5):679–688
Molina Rodríguez JL et al (2011) Low rectal cancer: abdominoperineal resection or low Hartmann resection? A postoperative outcome analysis. Dis Colon Rectum 54(8):958–962
Westerduin E et al (2017) Low Hartmann’s procedure or intersphincteric proctectomy for distal rectal cancer: a retrospective comparative cohort study. Int J Colorectal Dis 32(11):1583–1589
Asplund D et al (2015) Persistent perineal morbidity is common following abdominoperineal excision for rectal cancer. Int J Colorectal Dis 30(11):1563–1570
Author information
Authors and Affiliations
Contributions
Study concepts: Jelle P. A. Algie, Koen C. M. J. Peeters, Jan Willem T. Dekker; study design: Jelle P. A. Algie, Robert T. van Kooten, Rob A. E. M. Tollenaar, Michel W. J. M. Wouters, Koen C. M. J. Peeters, Jan Willem T. Dekker; data acquisition: Jelle P. A. Algie, Robert T. van Kooten; quality control of data: Jelle P. A. Algie, Robert T. van Kooten, Rob A. E. M. Tollenaar, Michel W. J. M. Wouters, Koen C. M. J. Peeters, Jan Willem T. Dekker; data analysis and interpretation: Jelle P. A. Algie, Robert T. van Kooten, Rob A. E. M. Tollenaar, Michel W. J. M. Wouters, Koen C. M. J. Peeters, Jan Willem T. Dekker; statistical analysis: Jelle P. A. Algie, Robert T. van Kooten, Jan Willem T. Dekker; manuscript preparation: Jelle P. A. Algie, Robert T. van Kooten; manuscript editing: Jelle P. A. Algie, Robert T. van Kooten, Jan Willem T. Dekker; manuscript review: Rob A. E. M. Tollenaar, Michel W. J. M. Wouters, Koen C. M. J. Peeters, Jan Willem T. Dekker.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Algie, J.P.A., van Kooten, R.T., Tollenaar, R.A.E.M. et al. Stoma versus anastomosis after sphincter-sparing rectal cancer resection; the impact on health-related quality of life. Int J Colorectal Dis 37, 2197–2205 (2022). https://doi.org/10.1007/s00384-022-04257-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04257-w